Arch Hand Microsurg.
2018 Dec;23(4):281-289. 10.12790/ahm.2018.23.4.281.
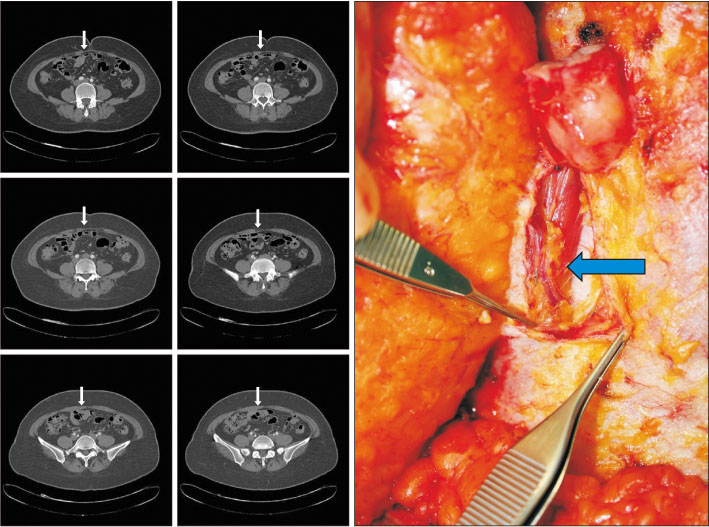
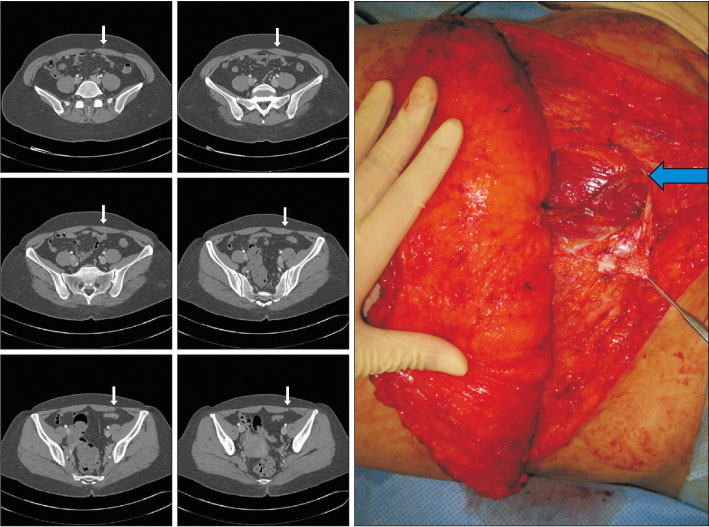
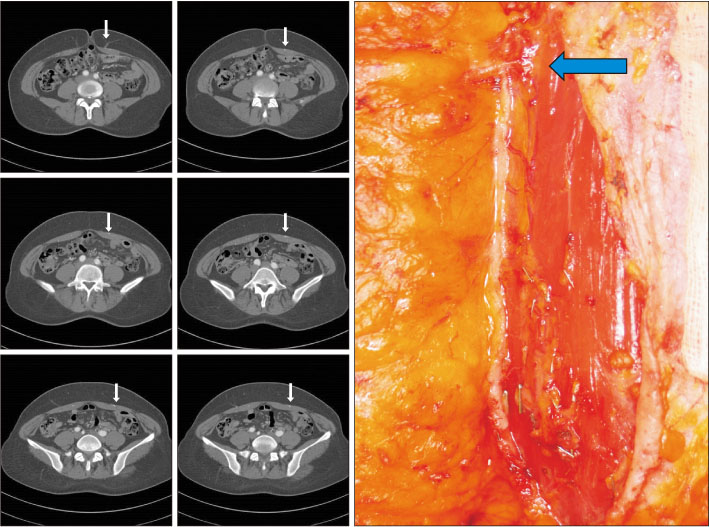
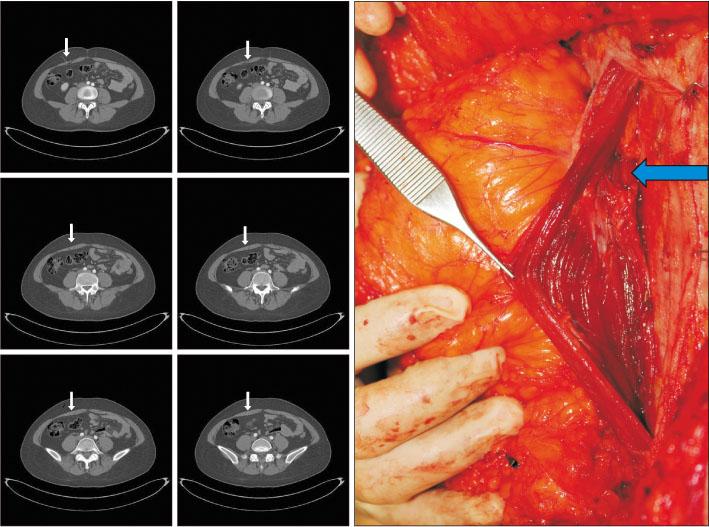
Classification of Deep Inferior Epigastric Perforator Courses Based on Computed Tomography Angiography: Incidences and Clinical Implications
- Affiliations
-
- 1Department of Plastic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. nicekek@korea.com
- 2Woori Plastic Surgery Clinic, Seoul, Korea.
- KMID: 2427396
- DOI: http://doi.org/10.12790/ahm.2018.23.4.281
Abstract
- PURPOSE
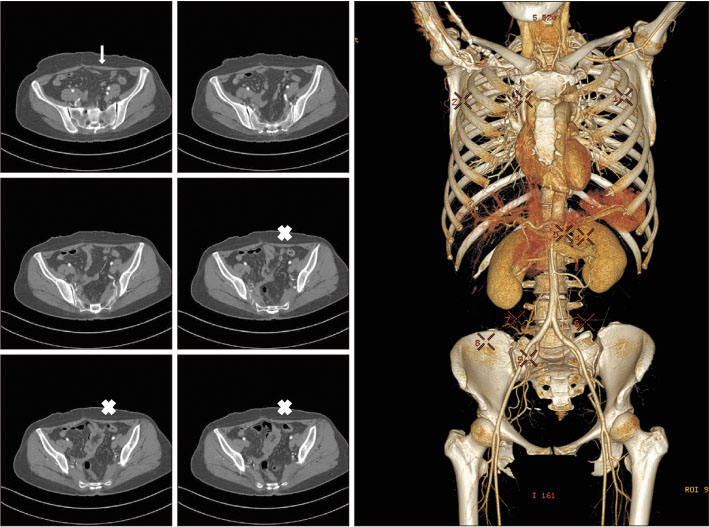
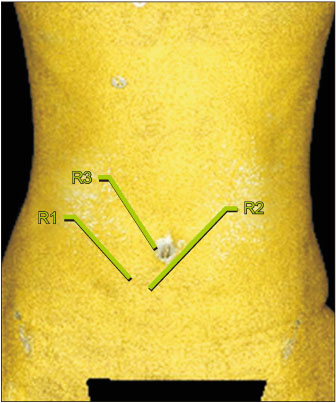
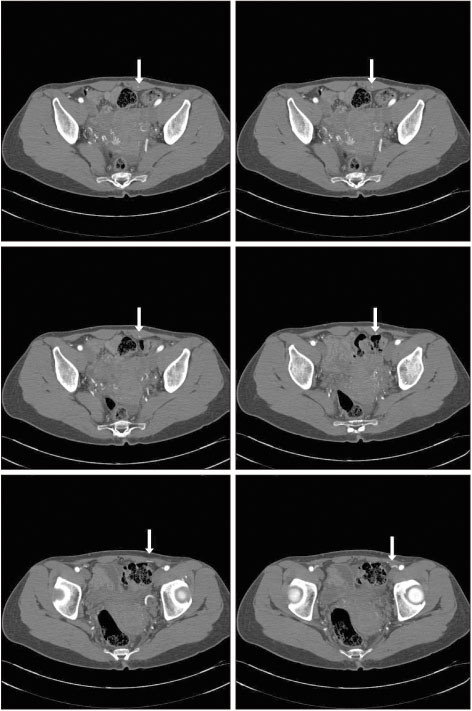
Preoperative surgical planning utilizing computed tomography angiography (CTA) has now become a routine in many practices. We analyzed the course of the deep inferior epigastric artery (DIEA) and its perforators (DIEP) that would either facilitate or hinder flap dissection based on CTA to aid surgical planning.
METHODS
The 115 consecutive patients who underwent abdominally based free flap breast reconstruction were enrolled in this prospective study. DIEA/P courses were categorized mainly according to their intramuscular courses and their incidences were investigated.
RESULTS
A total of 425 perforators were identified preoperatively on the CTA, with an average number of 3.7 distinctly visualized in the entire flap territory. Eighty-nine perforators (20.9%) had a favorable (less than 1 cm intramuscular course) pattern, namely long submuscular (34.8% of the patients), long subfascial (15.6%), and total circummuscular (13.9%). Overall 56.5% of the patients had at least one favorable DIEA/P. On the other hand, absence of DIEA and absence of adequate (>1 mm) DIEP was reported in 3 and 8 hemiabdomen.
CONCLUSION
Preoperative CTA evaluation of DIEA/P can be used to identify favorable as well as unfavorable courses for dissection to aid surgical planning.
MeSH Terms
Figure
Reference
-
1. Laporta R, Longo B, Sorotos M, Farcomeni A, Amorosi V, Santanelli di Pompeo F. Time-dependent factors in DIEP flap breast reconstruction. Microsurgery. 2017; 37:793–799.
Article2. Marsh D, Patel NG, Rozen WM, Chowdhry M, Sharma H, Ramakrishnan VV. Three routine free flaps per day in a single operating theatre: principles of a process mapping approach to improving surgical efficiency. Gland Surg. 2016; 5:107–114.3. Mathes DW, Neligan PC. Preoperative imaging techniques for perforator selection in abdomen-based microsurgical breast reconstruction. Clin Plast Surg. 2010; 37:581–591, xi.
Article4. Nahabedian MY. Overview of perforator imaging and flap perfusion technologies. Clin Plast Surg. 2011; 38:165–174.
Article5. Rozen WM, Chubb D, Grinsell D, Ashton MW. Computed tomographic angiography: clinical applications. Clin Plast Surg. 2011; 38:229–239.
Article6. Chubb D, Rozen WM, Ashton MW. Complete absence of the deep inferior epigastric artery: an increasingly detected anomaly detected with the use of advanced imaging technologies. J Reconstr Microsurg. 2010; 26:209–210.
Article7. Garusi C, Lohsiriwat V, de Lorenzi F, Manconi A, de Fiori E, Bellomi M. A subfascial variant of the deep inferior epigastric artery demonstrated by preoperative multidetector computed tomographic angiography: a case report. Microsurgery. 2010; 30:156–158.
Article8. Heo C, Yoo J, Minn K, Kim S. Circummuscular variant of the deep inferior epigastric perforator in breast reconstruction: importance of preoperative multidetector computed tomographic angiography. Aesthetic Plast Surg. 2008; 32:817–819.
Article9. Rozen WM, Houseman ND, Ashton MW. The absent inferior epigastric artery: a unique anomaly and implications for deep inferior epigastric artery perforator flaps. J Reconstr Microsurg. 2009; 25:289–293.
Article10. Whitaker IS, Rozen WM, Smit JM, Dimopoulou A, Ashton MW, Acosta R. Peritoneo-cutaneous perforators in deep inferior epigastric perforator flaps: a cadaveric dissection and computed tomographic angiography study. Microsurgery. 2009; 29:124–127.
Article11. Smit JM, Dimopoulou A, Liss AG, et al. Preoperative CT angiography reduces surgery time in perforator flap reconstruction. J Plast Reconstr Aesthet Surg. 2009; 62:1112–1117.
Article12. Wade RG, Watford J, Wormald JCR, Bramhall RJ, Figus A. Perforator mapping reduces the operative time of DIEP flap breast reconstruction: a systematic review and metaanalysis of preoperative ultrasound, computed tomography and magnetic resonance angiography. J Plast Reconstr Aesthet Surg. 2018; 71:468–477.
Article13. Fitzgerald O'Connor E, Rozen WM, Chowdhry M, Band B, Ramakrishnan VV, Griffiths M. Preoperative computed tomography angiography for planning DIEP flap breast reconstruction reduces operative time and overall complications. Gland Surg. 2016; 5:93–98.14. Keys KA, Louie O, Said HK, Neligan PC, Mathes DW. Clinical utility of CT angiography in DIEP breast reconstruction. J Plast Reconstr Aesthet Surg. 2013; 66:e61–e65.
Article15. Kim EK, Kang BS, Hong JP. The distribution of the perforators in the anterolateral thigh and the utility of multidetector row computed tomography angiography in preoperative planning. Ann Plast Surg. 2010; 65:155–160.
Article16. Katz RD, Manahan MA, Rad AN, Flores JI, Singh NK, Rosson GD. Classification schema for anatomic variations of the inferior epigastric vasculature evaluated by abdominal CT angiograms for breast reconstruction. Microsurgery. 2010; 30:593–602.
Article17. Ireton JE, Lakhiani C, Saint-Cyr M. Vascular anatomy of the deep inferior epigastric artery perforator flap: a systematic review. Plast Reconstr Surg. 2014; 134:810e–821e.18. Godfrey PM, Godfrey NV, Romita MC. The “circummuscular” free TRAM pedicle: a trap. Plast Reconstr Surg. 1994; 93:178–180.19. Hill C, Millar R. Vascular assymetry in a “circummuscular” free TRAM pedicle--a potential hazard. Plast Reconstr Surg. 1997; 99:1199–1200.
Article20. Bar-Meir ED, Reish RG, Yueh JH, McArdle C, Tobias AM, Lee BT. The Maylard incision: a low transverse incision variant seen in DIEP flap breast reconstruction. J Plast Reconstr Aesthet Surg. 2009; 62:e447–e452.
Article21. Selber JC, Serletti JM. The deep inferior epigastric perforator flap: myth and reality. Plast Reconstr Surg. 2010; 125:50–58.
Article22. Wang XL, Liu LB, Song FM, Wang QY. Meta-analysis of the safety and factors contributing to complications of MS-TRAM, DIEP, and SIEA flaps for breast reconstruction. Aesthetic Plast Surg. 2014; 38:681–691.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Preoperative Marking Template for Deep Inferior Epigastric Artery Perforator Flap Perforators in Breast Reconstruction
- Atypical Patterns of Deep Inferior Epigastric Artery: Clinical Implication of Preoperative CT Angiography
- The Value of Preoperative Multidetector Computed Tomography for Deep Inferior Epigastric Artery Perforator Free Flap
- Anatomical Study for Vascular Distribution of the Perforator of Deep Inferior Epigastric Artery in Koreans
- "Mini-Flow-Through" Deep Inferior Epigastric Perforator Flap for Breast Reconstruction with Preservation of Both Internal Mammary and Deep Inferior Epigastric Vessels