Korean J Radiol.
2017 Jun;18(3):536-542. 10.3348/kjr.2017.18.3.536.
Value of the Post-Operative CT in Predicting Delayed Flap Failures Following Head and Neck Cancer Surgery
- Affiliations
-
- 1Department of Radiology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul 05355, Korea. evee0914@chollian.net
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Ilsong Memorial Institute of Head and Neck Cancer, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul 05355, Korea.
- 3Department of Plastic Surgery, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul 05355, Korea.
- KMID: 2427309
- DOI: http://doi.org/10.3348/kjr.2017.18.3.536
Abstract
OBJECTIVE
To identify post-operative computed tomography (CT) findings associated with delayed flap failures following head and neck cancer surgery.
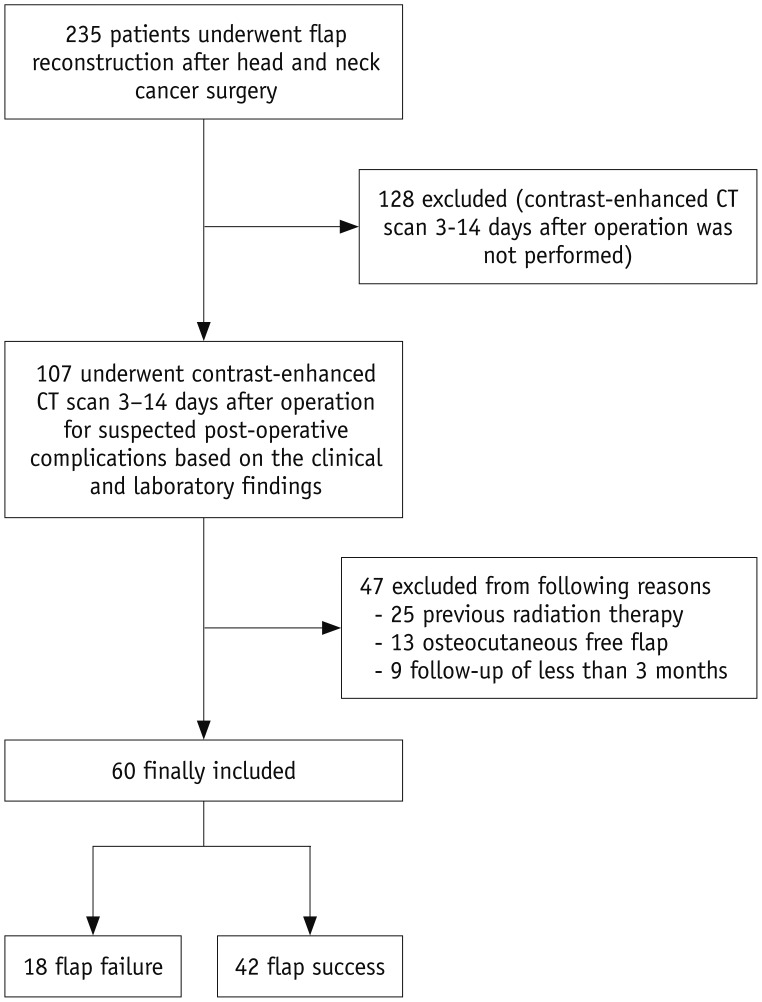
MATERIALS AND METHODS
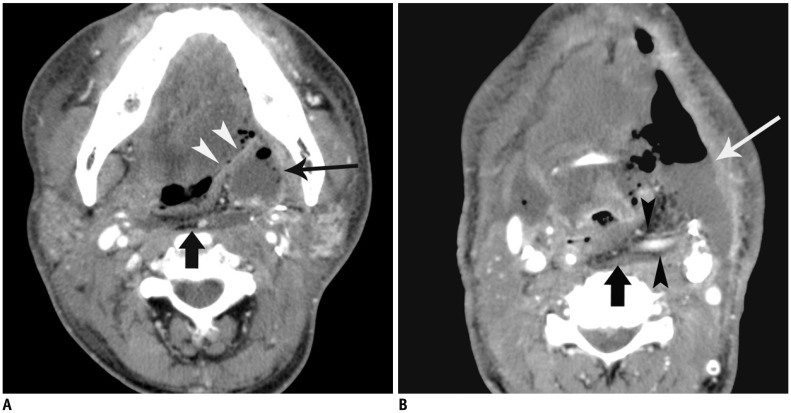
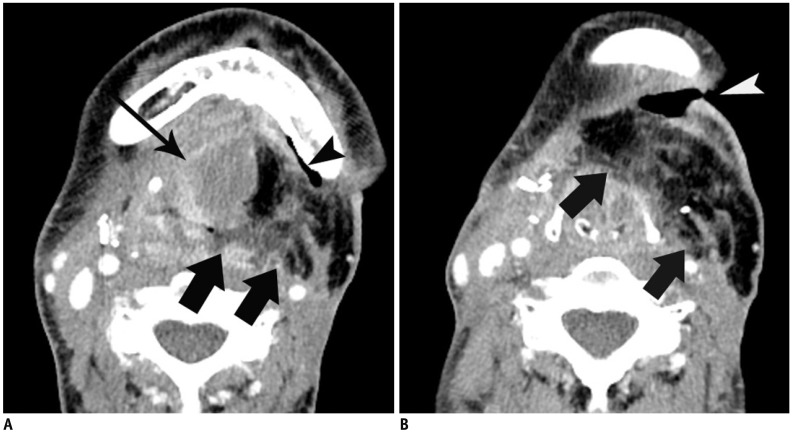
We retrospectively reviewed 60 patients who underwent flap reconstruction after head and neck cancer surgery and post-operative (3-14 days) contrast-enhanced CT scans for suspected complications. Patients were divided into two groups: delayed flap failure patients (patients required flap revision) (n = 18) and flap success patients (n = 42). Clinical data (age, sex, T-stage, type of flap, and time interval between reconstruction surgery and CT) and post-operative CT findings of flap status (maximum dimension of the flap, intra- or peri-flap fluid collection and intra- or peri-flap air collection, fat infiltration within the flap, fistula to adjacent aerodigestive tract or skin, and enhanced vascular pedicle) were assessed and compared between the two groups.
RESULTS
CT findings showed that the following flap anomalies were observed more frequently in the delayed flap failure group than in the flap success group: intra- or peri-flap fluid collection > 4 cm (61.1% vs. 23.8%, p < 0.05), intra- or peri-flap air collection > 2 cm (61.1% vs. 2.4%, p < 0.001), and fistula to adjacent aerodigestive tract or skin (44.4% vs. 0%, p < 0.001). The maximum dimension of the flap, fat infiltration within the flap, and enhanced vascular pedicle were not associated with delayed flap failures.
CONCLUSION
A large amount of fluid or air collection and fistula are the CT findings that were associated with delayed flap failures in patients with suspected post-operative complications after head and neck cancer surgery.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Age of Data in Contemporary Research Articles Published in Representative General Radiology Journals
Ji Hun Kang, Dong Hwan Kim, Seong Ho Park, Jung Hwan Baek
Korean J Radiol. 2018;19(6):1172-1178. doi: 10.3348/kjr.2018.19.6.1172.
Reference
-
1. le Nobel GJ, Higgins KM, Enepekides DJ. Predictors of complications of free flap reconstruction in head and neck surgery: analysis of 304 free flap reconstruction procedures. Laryngoscope. 2012; 122:1014–1019. PMID: 22407907.
Article2. Shum J, Markiewicz MR, Park E, Bui T, Lubek J, Bell RB, et al. Low prealbumin level is a risk factor for microvascular free flap failure. J Oral Maxillofac Surg. 2014; 72:169–177. PMID: 23911143.
Article3. Kim BD, Ver Halen JP, Grant DW, Kim JY. Anesthesia duration as an independent risk factor for postoperative complications in free flap surgery: a review of 1,305 surgical cases. J Reconstr Microsurg. 2014; 30:217–226. PMID: 24163224.
Article4. Song H, Kim JH, Park MC, Park DH, Lee K, Lee IJ. Usefulness of serum C-reactive protein level for predicting flap complication after performing free microvascular head and neck reconstruction. J Craniofac Surg. 2014; 25:1348–1351. PMID: 24892417.
Article5. Bourget A, Chang JT, Wu DB, Chang CJ, Wei FC. Free flap reconstruction in the head and neck region following radiotherapy: a cohort study identifying negative outcome predictors. Plast Reconstr Surg. 2011; 127:1901–1908. PMID: 21228745.
Article6. Singh B, Cordeiro PG, Santamaria E, Shaha AR, Pfister DG, Shah JP. Factors associated with complications in microvascular reconstruction of head and neck defects. Plast Reconstr Surg. 1999; 103:403–411. PMID: 9950525.
Article7. Khouri RK, Cooley BC, Kunselman AR, Landis JR, Yeramian P, Ingram D, et al. A prospective study of microvascular free-flap surgery and outcome. Plast Reconstr Surg. 1998; 102:711–721. PMID: 9727436.
Article8. Bozikov K, Arnez ZM. Factors predicting free flap complications in head and neck reconstruction. J Plast Reconstr Aesthet Surg. 2006; 59:737–742. PMID: 16782570.
Article9. Mücke T, Rau A, Weitz J, Ljubic A, Rohleder N, Wolff KD, et al. Influence of irradiation and oncologic surgery on head and neck microsurgical reconstructions. Oral Oncol. 2012; 48:367–371. PMID: 22155256.
Article10. Genden EM, Rinaldo A, Suárez C, Wei WI, Bradley PJ, Ferlito A. Complications of free flap transfers for head and neck reconstruction following cancer resection. Oral Oncol. 2004; 40:979–984. PMID: 15509488.
Article11. Mücke T, Wolff KD, Wagenpfeil S, Mitchell DA, Hölzle F. Immediate microsurgical reconstruction after tumor ablation predicts survival among patients with head and neck carcinoma. Ann Surg Oncol. 2010; 17:287–295. PMID: 19841982.
Article12. Frederick JW, Sweeny L, Carroll WR, Peters GE, Rosenthal EL. Outcomes in head and neck reconstruction by surgical site and donor site. Laryngoscope. 2013; 123:1612–1617. PMID: 23686870.
Article13. Fisher J, Wood MB. Late necrosis of a latissimus dorsi free flap. Plast Reconstr Surg. 1984; 74:274–281. PMID: 6463151.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Free-flap reconstruction in recurrent head and neck cancer: A retrospective review of 124 cases
- Contribution of Perforator Flaps in the Flap Selection for Head and Neck Reconstruction
- Reconstruction of Multiple Defects after Head and Neck Cancer Ablation
- Free flap reconstructions for head and neck cancer
- Lateral Arm Free Flap for Oral Cavity and Oropharyngeal Reconstruction