Korean J Radiol.
2017 Oct;18(5):852-859. 10.3348/kjr.2017.18.5.852.
A Novel Flow Diverter (Tubridge) for the Treatment of Recurrent Aneurysms: A Single-Center Experience
- Affiliations
-
- 1Department of Neurosurgery, Changhai Hospital, Second Military Medical University, Shanghai 200433, P.R. China. chstroke@163.com
- KMID: 2427222
- DOI: http://doi.org/10.3348/kjr.2017.18.5.852
Abstract
OBJECTIVE
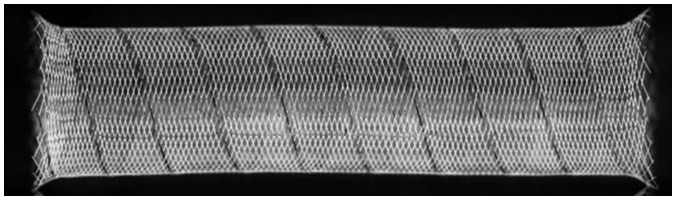
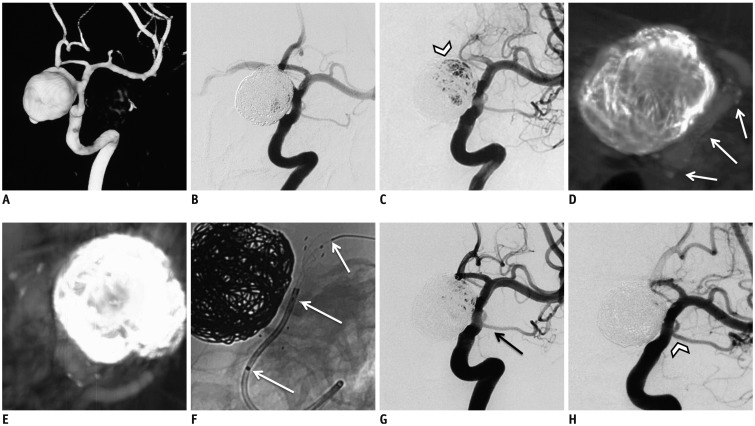
The Tubridge flow diverter (FD) is a novel device aimed at reconstructing the parent artery and occluding complex aneurysms. Retreatment of recurrent aneurysms using the FD is challenging. We report our initial experience in the repair of aneurysm recurrence with the FD.
MATERIALS AND METHODS
A database was reviewed prospectively, and 8 patients with 8 recurrent aneurysms (mean size, 16.7 mm) were identified. Four aneurysms had previously ruptured. The previous aneurysm treatment consisted of coiling in 1 aneurysm and single-stent-assisted coiling in 7 aneurysms. The procedural complications and clinical and angiographic outcomes were analyzed.
RESULTS
Six aneurysms were treated by using a single Tubridge FD alone, while the remaining 2 were treated with FD + coiling. The immediate results of the 8 aneurysms were that they all showed incomplete occlusion. Neither major ischemic nor hemorrhagic complications occurred; however, 1 patient experienced a vasospasm. Follow-up angiographies were available for 7 aneurysms; the mean follow-up was 16.9 months (7-36 months). Five aneurysms were completely occluded, whereas 2 had a residual neck. Severe asymptomatic stenosis of 1 parent artery of a vertebral artery dissecting aneurysm was found. All visible branches covered by the FD were patent. All patients were clinically assessed as having attained a favorable outcome (modified Rankin Scale score ≤ 2) at discharge and follow-up.
CONCLUSION
In selected patients, the Tubridge FD can provide a safe and efficient option for the retreatment of recurrent aneurysms. Nevertheless, attention should be paid to several technical points.
MeSH Terms
Figure
Cited by 2 articles
-
Age of Data in Contemporary Research Articles Published in Representative General Radiology Journals
Ji Hun Kang, Dong Hwan Kim, Seong Ho Park, Jung Hwan Baek
Korean J Radiol. 2018;19(6):1172-1178. doi: 10.3348/kjr.2018.19.6.1172.A Newly-Developed Flow Diverter (FloWise) for Internal Carotid Artery Aneurysm: Results of a Pilot Clinical Study
Byung Moon Kim, Keun Young Park, Jae Whan Lee, Joonho Chung, Dong Joon Kim, Dong Ik Kim
Korean J Radiol. 2019;20(3):505-512. doi: 10.3348/kjr.2018.0421.
Reference
-
1. McDonald JS, McDonald RJ, Fan J, Kallmes DF, Lanzino G, Cloft HJ. Comparative effectiveness of unruptured cerebral aneurysm therapies: propensity score analysis of clipping versus coiling. Stroke. 2013; 44:988–994. PMID: 23449260.2. Lin N, Cahill KS, Frerichs KU, Friedlander RM, Claus EB. Treatment of ruptured and unruptured cerebral aneurysms in the USA: a paradigm shift. J Neurointerv Surg. 2012; 4:182–189. PMID: 21990481.
Article3. Campi A, Ramzi N, Molyneux AJ, Summers PE, Kerr RS, Sneade M, et al. Retreatment of ruptured cerebral aneurysms in patients randomized by coiling or clipping in the International Subarachnoid Aneurysm Trial (ISAT). Stroke. 2007; 38:1538–1544. PMID: 17395870.
Article4. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet. 2002; 360:1267–1274. PMID: 12414200.
Article5. Ferns SP, Sprengers ME, van Rooij WJ, Rinkel GJ, van Rijn JC, Bipat S, et al. Coiling of intracranial aneurysms: a systematic review on initial occlusion and reopening and retreatment rates. Stroke. 2009; 40:e523–e529. PMID: 19520984.6. Dorfer C, Gruber A, Standhardt H, Bavinzski G, Knosp E. Management of residual and recurrent aneurysms after initial endovascular treatment. Neurosurgery. 2012; 70:537–553. discussion 553-554. PMID: 21904266.
Article7. Kim BM, Kim DJ, Kim DI. A new flow-diverter (the FloWise): in-vivo evaluation in an elastase-induced rabbit aneurysm model. Korean J Radiol. 2016; 17:151–158. PMID: 26798228.
Article8. Huang QH, Yang PF, Zhang X, Shi Y, Shao XM, Liu JM. [Effects of flow diverter with low porosity on cerebral aneurysms: a numerical stimulative study]. Zhonghua Yi Xue Za Zhi. 2010; 90:1024–1027. PMID: 20646519.9. Simgen A, Ley D, Roth C, Yilmaz U, Körner H, Mühl-Benninghaus R, et al. Evaluation of a newly designed flow diverter for the treatment of intracranial aneurysms in an elastase-induced aneurysm model, in New Zealand white rabbits. Neuroradiology. 2014; 56:129–137. PMID: 24496551.
Article10. Zhou Y, Yang PF, Fang YB, Xu Y, Hong B, Zhao WY, et al. A novel flow-diverting device (Tubridge) for the treatment of 28 large or giant intracranial aneurysms: a single-center experience. AJNR Am J Neuroradiol. 2014; 35:2326–2333. PMID: 24722307.
Article11. Hong B, Wang K, Huang Q, Xu Y, Fang X, Li Z, et al. Effects of metal coverage rate of flow diversion device on neointimal growth at side branch ostium and stented artery: an animal experiment in rabbit abdominal aorta. Neuroradiology. 2012; 54:849–855. PMID: 22170078.
Article12. Suh SH, Cloft HJ, Lanzino G, Woodward K, Kallmes DF. Interobserver agreement after pipeline embolization device implantation. AJNR Am J Neuroradiol. 2013; 34:1215–1218. PMID: 23275597.
Article13. Roy D, Milot G, Raymond J. Endovascular treatment of unruptured aneurysms. Stroke. 2001; 32:1998–2004. PMID: 11546888.
Article14. Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005; 366:809–817.
Article15. Darsaut TE, Raymond J. Barrow Ruptured Aneurysm Trial: 3-year results. J Neurosurg. 2013; 119:1642–1644.16. Taki W, Sakai N, Suzuki H. Prospective Registry of Subarachnoid Aneurysms Treatment (PRESAT) group. Importance of independent evaluation of initial anatomic results after endovascular coiling for ruptured cerebral aneurysms. J Clin Neurosci. 2013; 20:527–531. PMID: 23324438.
Article17. Taki W. PRESAT group. Sakai N, Suzuki H. Factors predicting retreatment and residual aneurysms at 1 year after endovascular coiling for ruptured cerebral aneurysms: Prospective Registry of Subarachnoid Aneurysms Treatment (PRESAT) in Japan. Neuroradiology. 2012; 54:597–606. PMID: 21861080.18. Nguyen TN, Hoh BL, Amin-Hanjani S, Pryor JC, Ogilvy CS. Comparison of ruptured vs unruptured aneurysms in recanalization after coil embolization. Surg Neurol. 2007; 68:19–23. PMID: 17586214.
Article19. Raymond J, Guilbert F, Weill A, Georganos SA, Juravsky L, Lambert A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003; 34:1398–1403. PMID: 12775880.
Article20. Chalouhi N, Tjoumakaris S, Gonzalez LF, Dumont AS, Starke RM, Hasan D, et al. Coiling of large and giant aneurysms: complications and long-term results of 334 cases. AJNR Am J Neuroradiol. 2014; 35:546–552. PMID: 23945229.
Article21. Johnston SC, Dowd CF, Higashida RT, Lawton MT, Duckwiler GR, Gress DR. CARAT Investigators. Predictors of rehemorrhage after treatment of ruptured intracranial aneurysms: the Cerebral Aneurysm Rerupture After Treatment (CARAT) study. Stroke. 2008; 39:120–125. PMID: 18048860.22. Ringer AJ, Rodriguez-Mercado R, Veznedaroglu E, Levy EI, Hanel RA, Mericle RA, et al. Defining the risk of retreatment for aneurysm recurrence or residual after initial treatment by endovascular coiling: a multicenter study. Neurosurgery. 2009; 65:311–315. discussion 315. PMID: 19625910.23. Renowden SA, Koumellis P, Benes V, Mukonoweshuro W, Molyneux AJ, McConachie NS. Retreatment of previously embolized cerebral aneurysms: the risk of further coil embolization does not negate the advantage of the initial embolization. AJNR Am J Neuroradiol. 2008; 29:1401–1404. PMID: 18436614.
Article24. Henkes H, Fischer S, Liebig T, Weber W, Reinartz J, Miloslavski E, et al. Repeated endovascular coil occlusion in 350 of 2759 intracranial aneurysms: safety and effectiveness aspects. Neurosurgery. 2008; 62(6 Suppl 3):1532–1537. PMID: 18695570.
Article25. Tähtinen OI, Manninen HI, Vanninen RL, Rautio R, Haapanen A, Seppänen J, et al. Stent-assisted embolization of recurrent or residual intracranial aneurysms. Neuroradiology. 2013; 55:1221–1231. PMID: 23861213.
Article26. Zhang X, Lv N, Wang C, Cao W, Liu J, Huang Q. Late recurrence of a completely occluded large intracranial aneurysm treated with a Tubridge flow diverter. J Neurointerv Surg. 2017; 9:e6. PMID: 27342762.
Article27. Fischer S, Vajda Z, Aguilar Perez M, Schmid E, Hopf N, Bäzner H, et al. Pipeline embolization device (PED) for neurovascular reconstruction: initial experience in the treatment of 101 intracranial aneurysms and dissections. Neuroradiology. 2012; 54:369–382. PMID: 21881914.
Article28. Chalouhi N, Chitale R, Starke RM, Jabbour P, Tjoumakaris S, Dumont AS, et al. Treatment of recurrent intracranial aneurysms with the pipeline embolization device. J Neurointerv Surg. 2014; 6:19–23. PMID: 23345630.
Article29. Heiferman DM, Billingsley JT, Kasliwal MK, Johnson AK, Keigher KM, Frudit ME, et al. Use of flow-diverting stents as salvage treatment following failed stent-assisted embolization of intracranial aneurysms. J Neurointerv Surg. 2016; 8:692–695. PMID: 26041098.
Article30. Daou B, Starke RM, Chalouhi N, Tjoumakaris S, Hasan D, Khoury J, et al. Pipeline embolization device in the treatment of recurrent previously stented ccerebral aneurysms. AJNR Am J Neuroradiol. 2016; 37:849–855. PMID: 26611991.31. Sedat J, Chau Y, Moubarak K, Vargas J, Lonjon M. Endovascular treatment of recurrent coiled aneurysms: assessment of complications and rebleeding during a decade in a single center. Interv Neuroradiol. 2012; 18:14–19. PMID: 22440596.
Article32. Wagner A, Cortsen M, Hauerberg J, Romner B, Wagner MP. Treatment of intracranial aneurysms. Reconstruction of the parent artery with flow-diverting (Silk) stent. Neuroradiology. 2012; 54:709–718. PMID: 21894512.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Failure of Flow Diverter Treatment of Intracranial Aneurysms Related to the Fetal-type Posterior Communicating Artery
- Flow Diverter Device for Treatment of Cerebral Aneurysm with Short-Term Follow Up: Two Case Reports
- Treatment of a posterior cerebral artery aneurysm in the context of complex cardio-cerebrovascular variations using the Tubridge flow diverter
- Retreatment of a recurrent giant aneurysm of the internal carotid artery after treatment with a flow-diverting stent
- Blood flow in intracranial aneurysms treated with Pipeline embolization devices: computational simulation and verification with Doppler ultrasonography on phantom models