Korean J Radiol.
2017 Oct;18(5):753-762. 10.3348/kjr.2017.18.5.753.
Calcification Remodeling Index Characterized by Cardiac CT as a Novel Parameter to Predict the Use of Rotational Atherectomy for Coronary Intervention of Lesions with Moderate to Severe Calcification
- Affiliations
-
- 1Institute of Diagnostic and Interventional Radiology, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, Shanghai 200233, China. andrewssmu@msn.com
- 2Department of Cardiology, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, Shanghai 200233, China.
- KMID: 2427212
- DOI: http://doi.org/10.3348/kjr.2017.18.5.753
Abstract
OBJECTIVE
To assess the feasibility of calcification characterization by coronary computed tomography angiography (CCTA) to predict the use of rotational atherectomy (RA) for coronary intervention of lesions with moderate to severe calcification.
MATERIALS AND METHODS
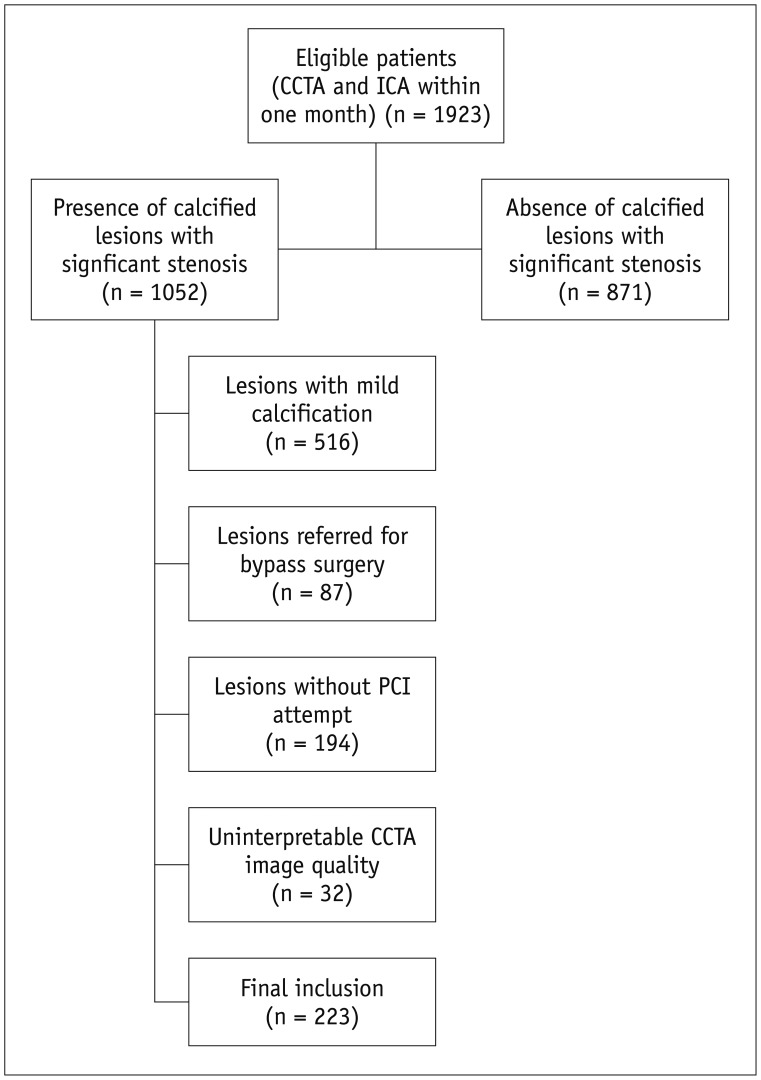
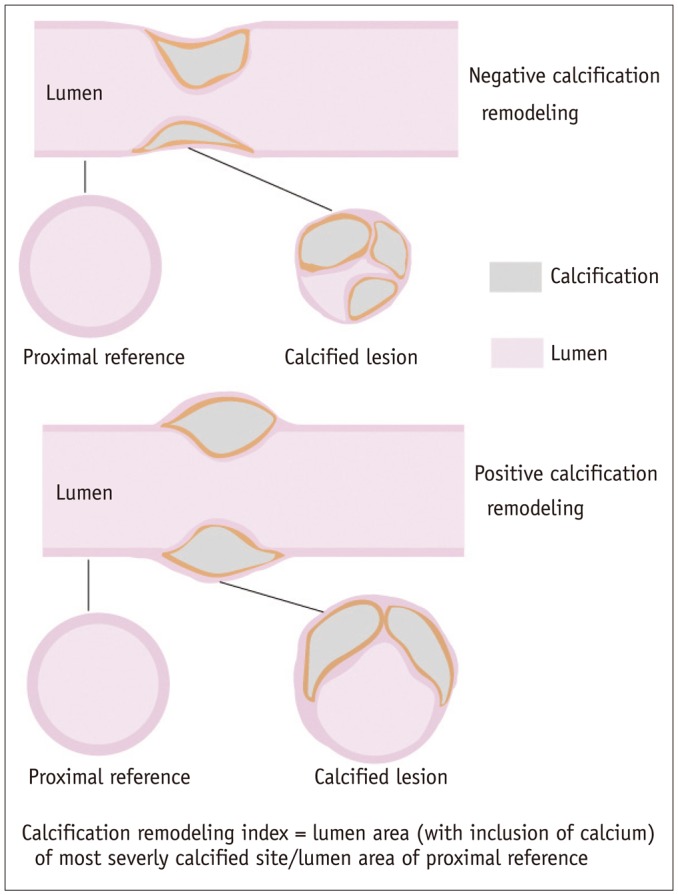
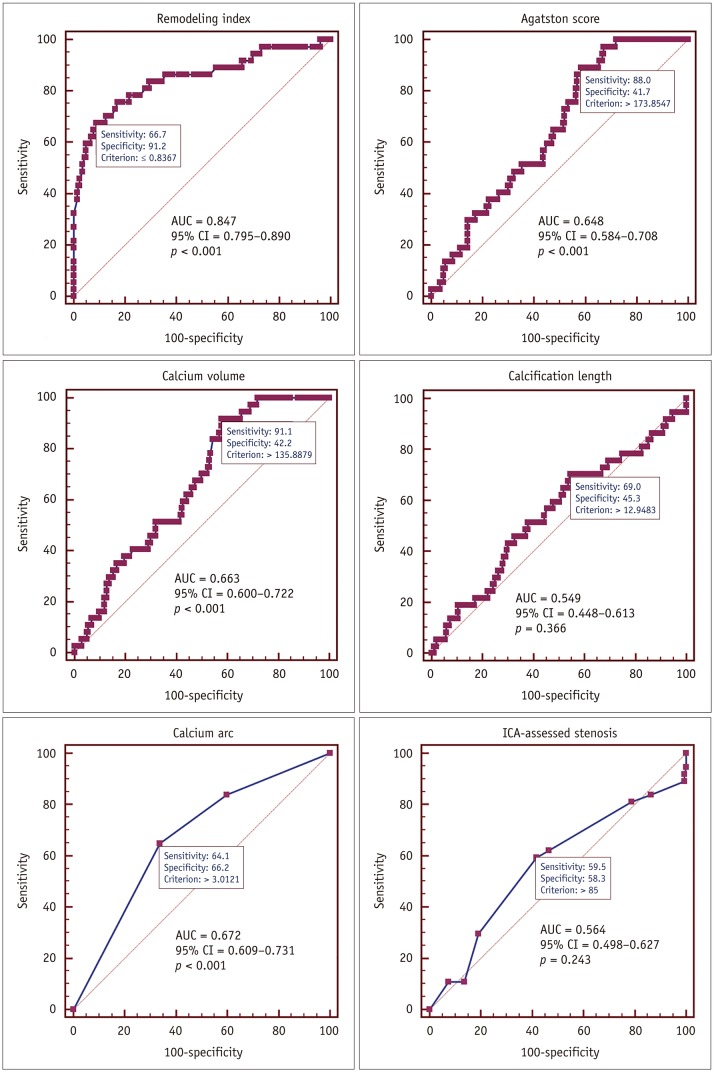
Patients with calcified lesions treated by percutaneous coronary intervention (PCI) who underwent both CCTA and invasive coronary angiography were retrospectively included in this study. Calcification remodeling index was calculated as the ratio of the smallest vessel cross-sectional area of the lesion to the proximal reference luminal area. Other parameters such as calcium volume, regional Agatston score, calcification length, and involved calcium arc quadrant were also recorded.
RESULTS
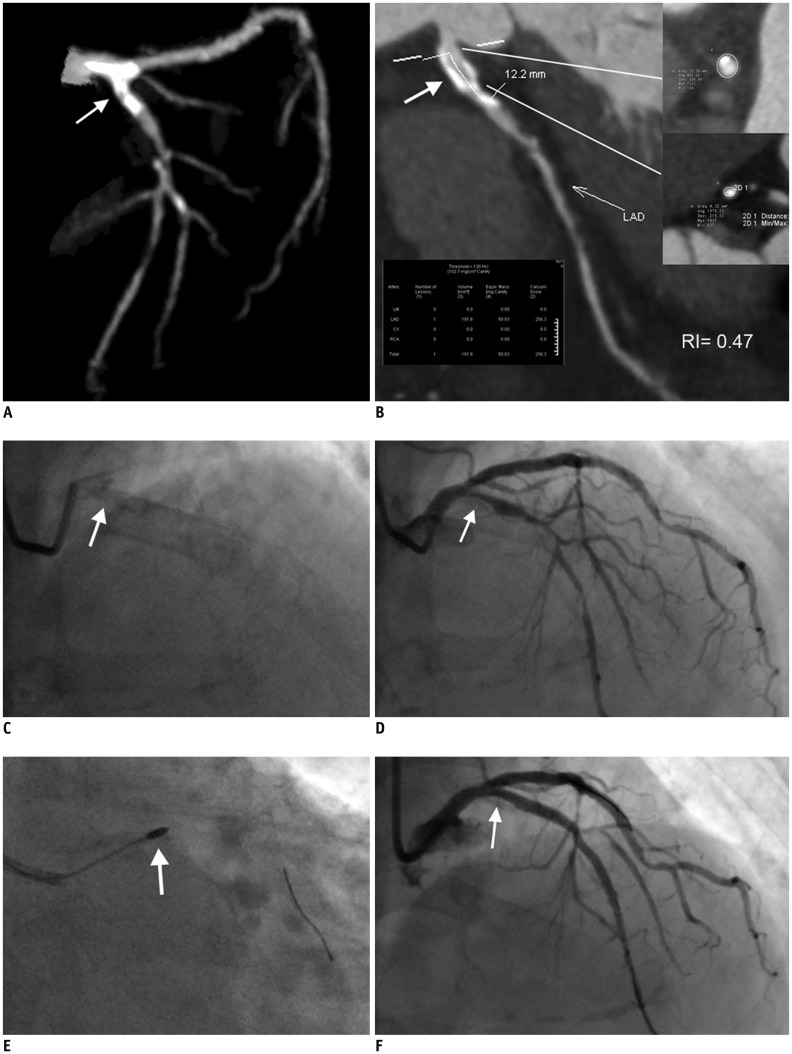
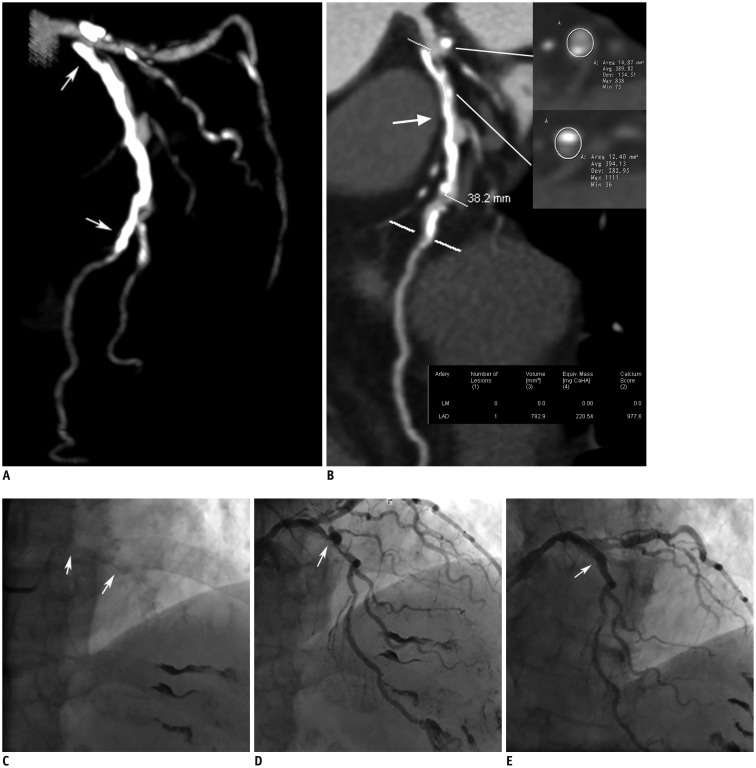
A total of 223 patients with 241 calcified lesions were finally included. Lesions with RA tended to have larger calcium volume, higher regional Agatston score, more involved calcium arc quadrants, and significantly smaller calcification remodeling index than lesions without RA. Receiver operating characteristic curve analysis revealed that the best cutoff value of calcification remodeling index was 0.84 (area under curve = 0.847, p < 0.001). Calcification remodeling index ≤ 0.84 was the strongest independent predictor (odds ratio: 251.47, p < 0.001) for using RA.
CONCLUSION
Calcification remodeling index was significantly correlated with the incidence of using RA to aid PCI. Calcification remodeling index ≤ 0.84 was the strongest independent predictor for using RA prior to stent implantation.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Area Under Curve
Atherectomy, Coronary
Computed Tomography Angiography
Female
Humans
Male
Middle Aged
Multivariate Analysis
Odds Ratio
Percutaneous Coronary Intervention
ROC Curve
Retrospective Studies
Severity of Illness Index
Vascular Calcification/diagnostic imaging/*pathology/surgery
Figure
Cited by 1 articles
-
Age of Data in Contemporary Research Articles Published in Representative General Radiology Journals
Ji Hun Kang, Dong Hwan Kim, Seong Ho Park, Jung Hwan Baek
Korean J Radiol. 2018;19(6):1172-1178. doi: 10.3348/kjr.2018.19.6.1172.
Reference
-
1. Ritchie JL, Hansen DD, Intlekofer MJ, Hall M, Auth DC. Rotational approaches to atherectomy and thrombectomy. Z Kardiol. 1987; 76(Suppl 6):59–65. PMID: 3439260.2. Bangalore S, Vlachos HA, Selzer F, Wilensky RL, Kip KE, Williams DO, et al. Percutaneous coronary intervention of moderate to severe calcified coronary lesions: insights from the National Heart, Lung, and Blood Institute Dynamic Registry. Catheter Cardiovasc Interv. 2011; 77:22–28. PMID: 20506328.
Article3. Moussa I, Ellis SG, Jones M, Kereiakes DJ, McMartin D, Rutherford B, et al. Impact of coronary culprit lesion calcium in patients undergoing paclitaxel-eluting stent implantation (a TAXUS-IV sub study). Am J Cardiol. 2005; 96:1242–1247. PMID: 16253590.
Article4. Tuzcu EM, Berkalp B, De Franco AC, Ellis SG, Goormastic M, Whitlow PL, et al. The dilemma of diagnosing coronary calcification: angiography versus intravascular ultrasound. J Am Coll Cardiol. 1996; 27:832–838. PMID: 8613611.
Article5. Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011; 364:226–235. PMID: 21247313.
Article6. Vliegenthart R, Oudkerk M, Hofman A, Oei HH, van Dijck W, van Rooij FJ, et al. Coronary calcification improves cardiovascular risk prediction in the elderly. Circulation. 2005; 112:572–577. PMID: 16009800.
Article7. Vavere AL, Arbab-Zadeh A, Rochitte CE, Dewey M, Niinuma H, Gottlieb I, et al. Coronary artery stenoses: accuracy of 64-detector row CT angiography in segments with mild, moderate, or severe calcification--a subanalysis of the CORE-64 trial. Radiology. 2011; 261:100–108. PMID: 21828192.
Article8. Kim YJ, Yong HS, Kim SM, Kim JA, Yang DH, Hong YJ, et al. Korean guidelines for the appropriate use of cardiac CT. Korean J Radiol. 2015; 16:251–285. PMID: 25741189.
Article9. Li Y, Zhang J, Lu Z, Pan J. Discrepant findings of computed tomography quantification of minimal lumen area of coronary artery stenosis: correlation with intravascular ultrasound. Eur J Radiol. 2012; 81:3270–3275. PMID: 22472144.
Article10. Tomey MI, Kini AS, Sharma SK. Current status of rotational atherectomy. JACC Cardiovasc Interv. 2014; 7:345–353. PMID: 24630879.
Article11. Taylor AJ, Burke AP, Farb A, Yousefi P, Malcom GT, Smialek J, et al. Arterial remodeling in the left coronary system: the role of high-density lipoprotein cholesterol. J Am Coll Cardiol. 1999; 34:760–767. PMID: 10483958.12. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011; 58:e44–e122. PMID: 22070834.13. McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: results from the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2006; 113:30–37. PMID: 16365194.14. Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004; 291:210–215. PMID: 14722147.
Article15. Tan K, Sulke N, Taub N, Sowton E. Clinical and lesion morphologic determinants of coronary angioplasty success and complications: current experience. J Am Coll Cardiol. 1995; 25:855–865. PMID: 7884088.
Article16. Lee RT, Grodzinsky AJ, Frank EH, Kamm RD, Schoen FJ. Structure-dependent dynamic mechanical behavior of fibrous caps from human atherosclerotic plaques. Circulation. 1991; 83:1764–1770. PMID: 2022029.
Article17. Hoffmann R, Mintz GS, Popma JJ, Satler LF, Kent KM, Pichard AD, et al. Treatment of calcified coronary lesions with Palmaz-Schatz stents. An intravascular ultrasound study. Eur Heart J. 1998; 19:1224–1231. PMID: 9740344.
Article18. Khattab AA, Otto A, Hochadel M, Toelg R, Geist V, Richardt G. Drug-eluting stents versus bare metal stents following rotational atherectomy for heavily calcified coronary lesions: late angiographic and clinical follow-up results. J Interv Cardiol. 2007; 20:100–106. PMID: 17391217.
Article19. Kawasaki M, Bouma BE, Bressner J, Houser SL, Nadkarni SK, MacNeill BD, et al. Diagnostic accuracy of optical coherence tomography and integrated backscatter intravascular ultrasound images for tissue characterization of human coronary plaques. J Am Coll Cardiol. 2006; 48:81–88. PMID: 16814652.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Experience in High Speed Rotational Coronary Atherectomy
- Interventions in Coronary Lesions Associated with Kawasaki Disease
- Rotational Atherectomy through Inner Guiding Catheter System for 1.25 mm Rotational Burr Non-Crossable Heavily Calcified Coronary Stenosis
- Contemporary Interventional Approach to Calcified Coronary Artery Disease
- Initial Experience of Rotational Atherectomy in Coronary Artery Disease