Korean J Radiol.
2017 Dec;18(6):915-925. 10.3348/kjr.2017.18.6.915.
Incidental, Small (< 3 cm), Unilocular, Pancreatic Cysts: Factors That Predict Lesion Progression during Imaging Surveillance
- Affiliations
-
- 1Department of Radiology, Chonnam National University Hospital, Gwangju 61469, Korea.
- 2Department of Radiology, Chonnam National University Medical School, Gwangju 61469, Korea. kjradsss@dreamwiz.com
- 3Center for Aging and Geriatrics, Chonnam National University Medical School, Gwangju 61469, Korea.
- 4Department of Gastroenterology, Chonnam National University Medical School, Gwangju 61469, Korea.
- KMID: 2427201
- DOI: http://doi.org/10.3348/kjr.2017.18.6.915
Abstract
OBJECTIVE
To explore the features that predict size increase and development of potential malignant features in incidentally detected, unilocular cystic pancreatic lesions (CPLs) less than 3 cm in diameter, during subsequent follow-up.
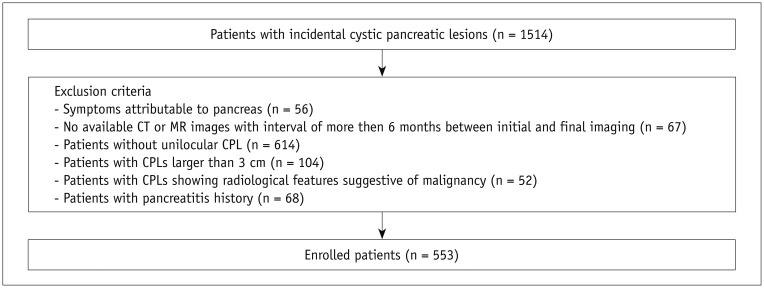
MATERIALS AND METHODS
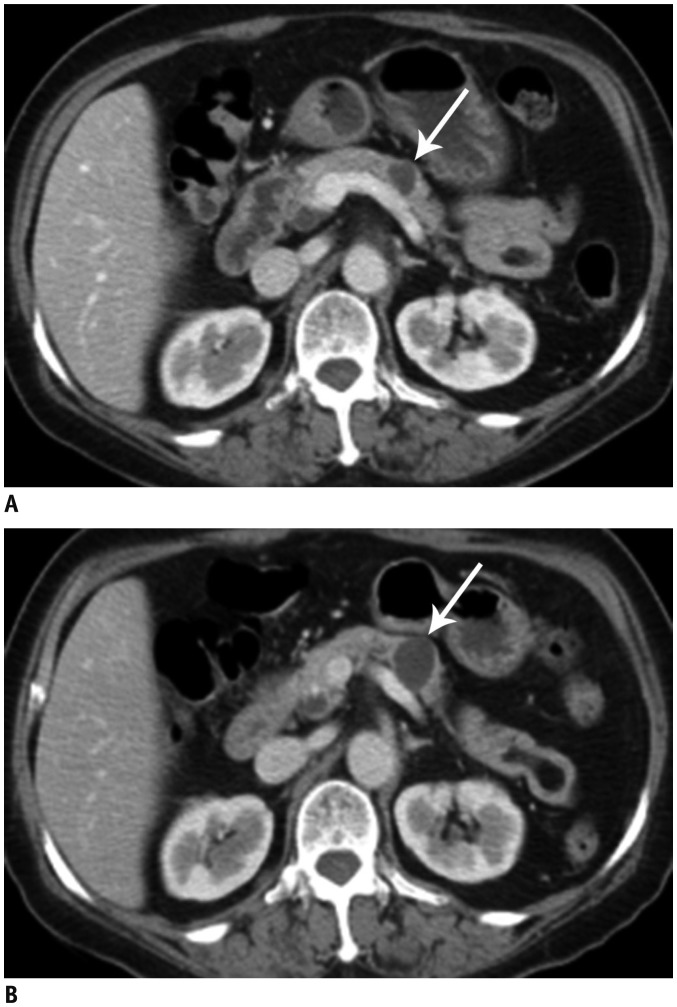
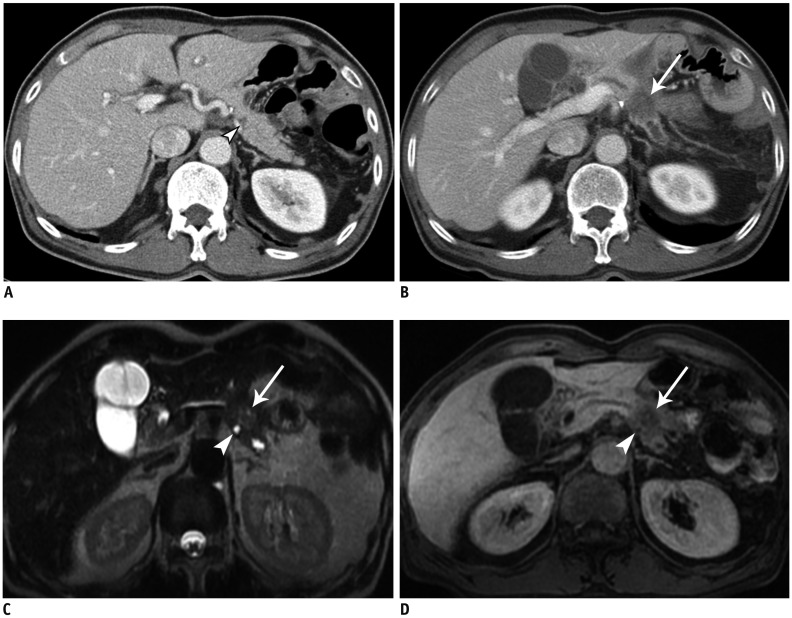
We retrieved data of patients diagnosed with unilocular CPLs less than 3 cm in diameter during the period from November 2003 through December 2014, using a computerized search. All serial CT and MR images were analyzed to identify the number, size, and location of CPLs; dilatation of the main pancreatic duct; and occurrence of worrisome features and high-risk stigmata of malignancy in the lesion. The characteristics of CPLs were compared between the increase (i.e., size increase during subsequent follow-up) and no-increase groups. For CPLs in the increase group, subgroup analysis was performed according to the lesion size at the last follow-up (< 3 cm vs. ≥ 3 cm).
RESULTS
Among 553 eligible patients, 132 (23.9%) had CPLs that increased in size, and 421 (76.1%) had CPLs that did not, during follow-up. Of the 132, 12 (9.1%) CPLs increased to diameters ≥ 3 cm at the final follow-up. Among the various factors, follow-up duration was a significant independent factor for an interval size increase of CPLs (p < 0.001). In the increase group, initial cyst size was a significant independent factor to predict later size increase to or beyond 3 cm in diameter (p < 0.001), and the initial cyst diameter ≥ 1.5 cm predicted such a growth with a sensitivity and specificity of 83% and 72%, respectively. No significant factors to predict the development of potential malignant features were identified.
CONCLUSION
Follow-up duration was associated with an interval size increase of CPLs. Among the growing CPLs, initial cyst size was associated with future lesion growth to and beyond 3 cm.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Disease Progression
Female
Follow-Up Studies
Humans
Image Processing, Computer-Assisted
Magnetic Resonance Imaging
Male
Middle Aged
Multivariate Analysis
Pancreatic Cyst/*diagnosis/diagnostic imaging/pathology
Pancreatic Neoplasms/*diagnosis/epidemiology/pathology
Retrospective Studies
Risk Factors
Tomography, X-Ray Computed
Figure
Reference
-
1. Zhang XM, Mitchell DG, Dohke M, Holland GA, Parker L. Pancreatic cysts: depiction on single-shot fast spin-echo MR images. Radiology. 2002; 223:547–553. PMID: 11997566.
Article2. Laffan TA, Horton KM, Klein AP, Berlanstein B, Siegelman SS, Kawamoto S, et al. Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol. 2008; 191:802–807. PMID: 18716113.
Article3. de Jong K, Nio CY, Hermans JJ, Dijkgraaf MG, Gouma DJ, van Eijck CH, et al. High prevalence of pancreatic cysts detected by screening magnetic resonance imaging examinations. Clin Gastroenterol Hepatol. 2010; 8:806–811. PMID: 20621679.
Article4. Lee KS, Sekhar A, Rofsky NM, Pedrosa I. Prevalence of incidental pancreatic cysts in the adult population on MR imaging. Am J Gastroenterol. 2010; 105:2079–2084. PMID: 20354507.
Article5. Scheiman JM, Hwang JH, Moayyedi P. American gastroenterological association technical review on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 2015; 148:824–848.e22. PMID: 25805376.
Article6. Handrich SJ, Hough DM, Fletcher JG, Sarr MG. The natural history of the incidentally discovered small simple pancreatic cyst: long-term follow-up and clinical implications. AJR Am J Roentgenol. 2005; 184:20–23. PMID: 15615944.
Article7. Kim YH, Saini S, Sahani D, Hahn PF, Mueller PR, Auh YH. Imaging diagnosis of cystic pancreatic lesions: pseudocyst versus nonpseudocyst. Radiographics. 2005; 25:671–685. PMID: 15888617.
Article8. Sahani DV, Kadavigere R, Saokar A, Fernandez-del Castillo C, Brugge WR, Hahn PF. Cystic pancreatic lesions: a simple imaging-based classification system for guiding management. Radiographics. 2005; 25:1471–1484. PMID: 16284129.
Article9. Sahani DV, Saokar A, Hahn PF, Brugge WR, Fernandez-Del Castillo C. Pancreatic cysts 3 cm or smaller: how aggressive should treatment be? Radiology. 2006; 238:912–919. PMID: 16439566.
Article10. Nougaret S, Reinhold C, Chong J, Escal L, Mercier G, Fabre JM, et al. Incidental pancreatic cysts: natural history and diagnostic accuracy of a limited serial pancreatic cyst MRI protocol. Eur Radiol. 2014; 24:1020–1029. PMID: 24569848.
Article11. Sahani DV, Kambadakone A, Macari M, Takahashi N, Chari S, Fernandez-del Castillo C. Diagnosis and management of cystic pancreatic lesions. AJR Am J Roentgenol. 2013; 200:343–354. PMID: 23345356.
Article12. Fernández-del Castillo C, Targarona J, Thayer SP, Rattner DW, Brugge WR, Warshaw AL. Incidental pancreatic cysts: clinicopathologic characteristics and comparison with symptomatic patients. Arch Surg. 2003; 138:427–434. PMID: 12686529.13. Gore RM, Wenzke DR, Thakrar KH, Newmark GM, Mehta UK, Berlin JW. The incidental cystic pancreas mass: a practical approach. Cancer Imaging. 2012; 12:414–421. PMID: 23022726.
Article14. Adsay NV. Cystic neoplasia of the pancreas: pathology and biology. J Gastrointest Surg. 2008; 12:401–404. PMID: 17957438.
Article15. Parra-Herran CE, Garcia MT, Herrera L, Bejarano PA. Cystic lesions of the pancreas: clinical and pathologic review of cases in a five year period. JOP. 2010; 11:358–364. PMID: 20601810.16. de Jong K, van Hooft JE, Nio CY, Gouma DJ, Dijkgraaf MG, Bruno MJ, et al. Accuracy of preoperative workup in a prospective series of surgically resected cystic pancreatic lesions. Scand J Gastroenterol. 2012; 47:1056–1063. PMID: 22571417.
Article17. Fernández-Del Castillo C, Tanaka M. Management of pancreatic cysts: the evidence is not here yet. Gastroenterology. 2015; 148:685–687. PMID: 25724457.
Article18. Hol L, Bruno MJ, Cahen DL. Follow-up of asymptomatic pancreatic cysts in clinical practice: a vignette questionnaire. Pancreatology. 2016; 16:416–422. PMID: 26973156.19. Walsh RM, Vogt DP, Henderson JM, Zuccaro G, Vargo J, Dumot J, et al. Natural history of indeterminate pancreatic cysts. Surgery. 2005; 138:665–670. discussion 670-671. PMID: 16269295.
Article20. Hoffman RL, Gates JL, Kochman ML, Ginsberg GG, Ahmad NA, Chandrasekhara V, et al. Analysis of cyst size and tumor markers in the management of pancreatic cysts: support for the original Sendai criteria. J Am Coll Surg. 2015; 220:1087–1095. PMID: 25868415.
Article21. Ip IK, Mortele KJ, Prevedello LM, Khorasani R. Focal cystic pancreatic lesions: assessing variation in radiologists’ management recommendations. Radiology. 2011; 259:136–141. PMID: 21292867.
Article22. Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012; 12:183–197. PMID: 22687371.
Article23. Edge MD, Hoteit M, Patel AP, Wang X, Baumgarten DA, Cai Q. Clinical significance of main pancreatic duct dilation on computed tomography: single and double duct dilation. World J Gastroenterol. 2007; 13:1701–1705. PMID: 17461473.
Article24. Lennon AM, Manos LL, Hruban RH, Ali SZ, Fishman EK, Kamel IR, et al. Role of a multidisciplinary clinic in the management of patients with pancreatic cysts: a single-center cohort study. Ann Surg Oncol. 2014; 21:3668–3674. PMID: 24806116.
Article25. Macari M, Megibow AJ. Focal cystic pancreatic lesions: variability in radiologists’ recommendations for follow-up imaging. Radiology. 2011; 259:20–23. PMID: 21436094.
Article26. Curry CA, Eng J, Horton KM, Urban B, Siegelman S, Kuszyk BS, et al. CT of primary cystic pancreatic neoplasms: can CT be used for patient triage and treatment? AJR Am J Roentgenol. 2000; 175:99–103. PMID: 10882255.27. Visser BC, Yeh BM, Qayyum A, Way LW, McCulloch CE, Coakley FV. Characterization of cystic pancreatic masses: relative accuracy of CT and MRI. AJR Am J Roentgenol. 2007; 189:648–656. PMID: 17715113.
Article28. Chiang AL, Lee LS. Clinical approach to incidental pancreatic cysts. World J Gastroenterol. 2016; 22:1236–1245. PMID: 26811661.
Article29. Yamada Y, Mori H, Matsumoto S, Kamei N, Hongo N. Invasive carcinomas derived from intraductal papillary mucinous neoplasms of the pancreas: a long-term follow-up assessment with CT imaging. J Comput Assist Tomogr. 2006; 30:885–890. PMID: 17082690.30. Tanno S, Nakano Y, Nishikawa T, Nakamura K, Sasajima J, Minoguchi M, et al. Natural history of branch duct intraductal papillary-mucinous neoplasms of the pancreas without mural nodules: long-term follow-up results. Gut. 2008; 57:339–343. PMID: 17660227.
Article31. Fritz S, Klauss M, Bergmann F, Hackert T, Hartwig W, Strobel O, et al. Small (Sendai negative) branch-duct IPMNs: not harmless. Ann Surg. 2012; 256:313–320. PMID: 22791105.32. Wong J, Weber J, Centeno BA, Vignesh S, Harris CL, Klapman JB, et al. High-grade dysplasia and adenocarcinoma are frequent in side-branch intraductal papillary mucinous neoplasm measuring less than 3 cm on endoscopic ultrasound. J Gastrointest Surg. 2013; 17:78–84. discussion 84-85. PMID: 22948841.33. Campbell NM, Katz SS, Escalon JG, Do RK. Imaging patterns of intraductal papillary mucinous neoplasms of the pancreas: an illustrated discussion of the International Consensus Guidelines for the Management of IPMN. Abdom Imaging. 2015; 40:663–677. PMID: 25219664.
Article34. Tanaka S, Nakao M, Ioka T, Takakura R, Takano Y, Tsukuma H, et al. Slight dilatation of the main pancreatic duct and presence of pancreatic cysts as predictive signs of pancreatic cancer: a prospective study. Radiology. 2010; 254:965–972. PMID: 20177107.
Article35. Matsubara S, Tada M, Akahane M, Yagioka H, Kogure H, Sasaki T, et al. Incidental pancreatic cysts found by magnetic resonance imaging and their relationship with pancreatic cancer. Pancreas. 2012; 41:1241–1246. PMID: 22699201.
Article36. Chernyak V, Flusberg M, Haramati LB, Rozenblit AM, Bellin E. Incidental pancreatic cystic lesions: is there a relationship with the development of pancreatic adenocarcinoma and all-cause mortality? Radiology. 2015; 274:161–169. PMID: 25117591.
Article37. Brook OR, Beddy P, Pahade J, Couto C, Brennan I, Patel P, et al. Delayed growth in incidental pancreatic cysts: are the current American College of Radiology recommendations for follow-up appropriate? Radiology. 2016; 278:752–761. PMID: 26348231.
Article38. Uehara H, Nakaizumi A, Ishikawa O, Iishi H, Tatsumi K, Takakura R, et al. Development of ductal carcinoma of the pancreas during follow-up of branch duct intraductal papillary mucinous neoplasm of the pancreas. Gut. 2008; 57:1561–1565. PMID: 18477671.
Article39. Vege SS, Ziring B, Jain R, Moayyedi P. Clinical Guidelines Committee. American Gastroenterology Association. American gastroenterological association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 2015; 148:819–822. PMID: 25805375.
Article40. Das A, Wells CD, Nguyen CC. Incidental cystic neoplasms of pancreas: what is the optimal interval of imaging surveillance? Am J Gastroenterol. 2008; 103:1657–1662. PMID: 18564119.
Article41. Wu BU, Sampath K, Berberian CE, Kwok KK, Lim BS, Kao KT, et al. Prediction of malignancy in cystic neoplasms of the pancreas: a population-based cohort study. Am J Gastroenterol. 2014; 109:121–129. PMID: 24080609.
Article42. Spinelli KS, Fromwiller TE, Daniel RA, Kiely JM, Nakeeb A, Komorowski RA, et al. Cystic pancreatic neoplasms: observe or operate. Ann Surg. 2004; 239:651–657. discussion 657-659. PMID: 15082969.43. Tsai HM, Chuang CH, Shan YS, Liu YS, Chen CY. Features associated with progression of small pancreatic cystic lesions: a retrospective study. World J Gastroenterol. 2015; 21:13309–13315. PMID: 26715814.
Article44. Yoen H, Kim JH, Lee DH, Ahn SJ, Yoon JH, Han JK. Fate of small pancreatic cysts (< 3 cm) after long-term follow-up: analysis of significant radiologic characteristics and proposal of follow-up strategies. Eur Radiol. 2017; 27:2591–2599. PMID: 27651145.45. Berland LL, Silverman SG, Gore RM, Mayo-Smith WW, Megibow AJ, Yee J, et al. Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol. 2010; 7:754–773. PMID: 20889105.
Article46. Singhi AD, Zeh HJ, Brand RE, Nikiforova MN, Chennat JS, Fasanella KE, et al. American Gastroenterological Association guidelines are inaccurate in detecting pancreatic cysts with advanced neoplasia: a clinicopathologic study of 225 patients with supporting molecular data. Gastrointest Endosc. 2016; 83:1107–1117.e2. PMID: 26709110.
Article47. Del Chiaro M, Verbeke C, Salvia R, Klöppel G, Werner J, McKay C, et al. European experts consensus statement on cystic tumours of the pancreas. Dig Liver Dis. 2013; 45:703–711. PMID: 23415799.
Article48. Kang MJ, Jang JY, Kim SJ, Lee KB, Ryu JK, Kim YT, et al. Cyst growth rate predicts malignancy in patients with branch duct intraductal papillary mucinous neoplasms. Clin Gastroenterol Hepatol. 2011; 9:87–93. PMID: 20851216.
Article49. Italian Association of Hospital Gastroenterologists and Endoscopists. Italian Association for the Study of the Pancreas. Buscarini E, Pezzilli R, Cannizzaro R, De Angelis C, et al. Italian consensus guidelines for the diagnostic workup and follow-up of cystic pancreatic neoplasms. Dig Liver Dis. 2014; 46:479–493. PMID: 24809235.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Squamoid cyst of pancreatic ducts: A case report
- Recent Strategies for Differentiation and Management of Incidental Pancreatic Cystic Lesions
- Imaging Diagnosis and Management of Pancreatic Cystic Neoplasms
- Paratracheal Air Cysts of Thoracic Inlet in Adults: CT Findings
- Diagnosis and Surveillance of Incidental Pancreatic Cystic Lesions: 2017 Consensus Recommendations of the Korean Society of Abdominal Radiology