Mechanisms by Which Atopic Dermatitis Predisposes to Food Allergy and the Atopic March
- Affiliations
-
- 1Department of Paediatrics, Yong Loo Lin School of Medicine, National University of Singapore, Singapore.
- 2Khoo Teck Puat-National University Children's Medical Institute, National University Hospital, National University Health System, Singapore.
- 3Department of Pediatrics, National Jewish Health, Denver, CO, USA. LeungD@njhealth.org
- 4Department of Pediatrics, University of Colorado at Denver Health Sciences Center, Aurora, CO, USA.
- KMID: 2426781
- DOI: http://doi.org/10.4168/aair.2019.11.1.4
Abstract
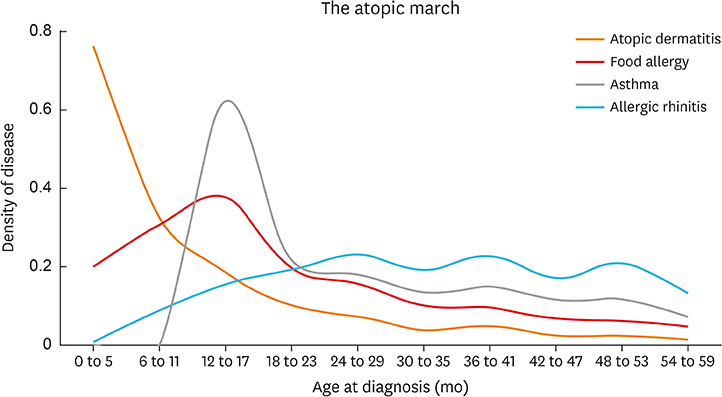
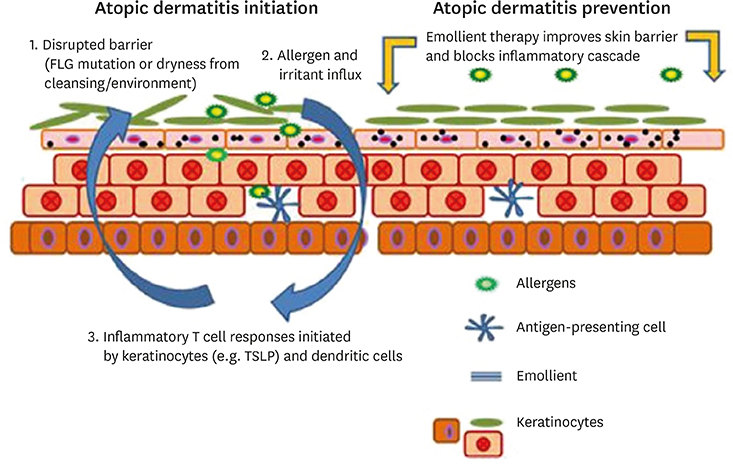
- The Atopic march denotes the progression from atopic dermatitis (AD) to the development of other allergic disorders such as immunoglobulin (Ig) E-mediated food allergy, allergic rhinitis and asthma in later childhood. There is increasing evidence from prospective birth cohort studies that early-onset AD is a risk factor for other allergic diseases or is found in strong association with them. Animal studies now provide mechanistic insights into the pathways that may be responsible for triggering the progression from the skin barrier dysfunction seen in AD to epicutaneous sensitization, food allergy and allergic airway disorders. Recent large randomized controlled trials have demonstrated the efficacy of early interventions targeted at AD and food allergy prevention. These show great promise for research into future strategies aimed at prevention of the atopic march.
MeSH Terms
Figure
Cited by 3 articles
-
Interactions Between Atopic Dermatitis and Staphylococcus aureus Infection: Clinical Implications
Jihyun Kim, Byung Eui Kim, Kangmo Ahn, Donald Y. M. Leung
Allergy Asthma Immunol Res. 2019;11(5):593-603. doi: 10.4168/aair.2019.11.5.593.Imbalance of Gut Streptococcus, Clostridium, and Akkermansia Determines the Natural Course of Atopic Dermatitis in Infant
Yoon Mee Park, So-Yeon Lee, Mi-Jin Kang, Bong-Soo Kim, Min-Jung Lee, Sung Su Jung, Ji Sun Yoon, Hyun-Ju Cho, Eun Lee, Song-I Yang, Ju-Hee Seo, Hyo-Bin Kim, Dong In Suh, Youn Ho Shin, Kyung Won Kim, Kangmo Ahn, Soo-Jong Hong
Allergy Asthma Immunol Res. 2020;12(2):322-337. doi: 10.4168/aair.2020.12.2.322.Clinical Characteristics of Atopic Dermatitis in Korean School-Aged Children and Adolescents According to Onset Age and Severity
You Hoon Jeon, Kangmo Ahn, Jihyun Kim, Meeyong Shin, Soo-Jong Hong, So-Yeon Lee, Bok Yang Pyun, Taek Ki Min, Minyoung Jung, Jeongmin Lee, Tae Won Song, Hye-Young Kim, Sooyoung Lee, Kyunguk Jeong, Yoonha Hwang, Minji Kim, Yong Ju Lee, Min Jung Kim, Ji Young Lee, Hye Yung Yum, Gwang Cheon Jang, Young A Park, Jeong Hee Kim,
J Korean Med Sci. 2022;37(4):e30. doi: 10.3346/jkms.2022.37.e30.
Reference
-
1. Mallol J, Crane J, von Mutius E, Odhiambo J, Keil U, Stewart A, et al. The International Study of Asthma and Allergies in Childhood (ISAAC) phase three: a global synthesis. Allergol Immunopathol (Madr). 2013; 41:73–85.
Article2. Sicherer SH, Sampson HA. Food allergy: epidemiology, pathogenesis, diagnosis, and treatment. J Allergy Clin Immunol. 2014; 133:291–307.
Article3. Johansson E, Hershey GK. Contribution of an impaired epithelial barrier to the atopic march. Ann Allergy Asthma Immunol. 2018; 120:118–119.
Article4. Hill DA, Spergel JM. The atopic march: critical evidence and clinical relevance. Ann Allergy Asthma Immunol. 2018; 120:131–137.5. Belgrave DC, Granell R, Simpson A, Guiver J, Bishop C, Buchan I, et al. Developmental profiles of eczema, wheeze, and rhinitis: two population-based birth cohort studies. PLoS Med. 2014; 11:e1001748.
Article6. Saunes M, Øien T, Dotterud CK, Romundstad PR, Storrø O, Holmen TL, et al. Early eczema and the risk of childhood asthma: a prospective, population-based study. BMC Pediatr. 2012; 12:168.
Article7. von Kobyletzki LB, Bornehag CG, Hasselgren M, Larsson M, Lindström CB, Svensson Å. Eczema in early childhood is strongly associated with the development of asthma and rhinitis in a prospective cohort. BMC Dermatol. 2012; 12:11.
Article8. Carlsten C, Dimich-Ward H, Ferguson A, Watson W, Rousseau R, Dybuncio A, et al. Atopic dermatitis in a high-risk cohort: natural history, associated allergic outcomes, and risk factors. Ann Allergy Asthma Immunol. 2013; 110:24–28.
Article9. Tran MM, Lefebvre DL, Dharma C, Dai D, Lou WY, Subbarao P, et al. Predicting the atopic march: results from the Canadian Healthy Infant Longitudinal Development Study. J Allergy Clin Immunol. 2018; 141:601–607.e8.
Article10. Alduraywish SA, Standl M, Lodge CJ, Abramson MJ, Allen KJ, Erbas B, et al. Is there a march from early food sensitization to later childhood allergic airway disease? Results from two prospective birth cohort studies. Pediatr Allergy Immunol. 2017; 28:30–37.
Article11. Alduraywish SA, Lodge CJ, Campbell B, Allen KJ, Erbas B, Lowe AJ, et al. The march from early life food sensitization to allergic disease: a systematic review and meta-analyses of birth cohort studies. Allergy. 2016; 71:77–89.
Article12. Hill DA, Grundmeier RW, Ram G, Spergel JM. The epidemiologic characteristics of healthcare provider-diagnosed eczema, asthma, allergic rhinitis, and food allergy in children: a retrospective cohort study. BMC Pediatr. 2016; 16:133.
Article13. Lack G. Epidemiologic risks for food allergy. J Allergy Clin Immunol. 2008; 121:1331–1336.
Article14. Berdyshev E, Goleva E, Bronova I, Dyjack N, Rios C, Jung J, et al. Lipid abnormalities in atopic skin are driven by type 2 cytokines. JCI Insight. 2018; 3:98006.
Article15. Kim BE, Leung DY. Significance of skin barrier dysfunction in atopic dermatitis. Allergy Asthma Immunol Res. 2018; 10:207–215.
Article16. Barker JN, Palmer CN, Zhao Y, Liao H, Hull PR, Lee SP, et al. Null mutations in the filaggrin gene (FLG) determine major susceptibility to early-onset atopic dermatitis that persists into adulthood. J Invest Dermatol. 2007; 127:564–567.
Article17. Margolis DJ, Kim B, Apter AJ, Gupta J, Hoffstad O, Papadopoulos M, et al. Thymic stromal lymphopoietin variation, filaggrin loss of function, and the persistence of atopic dermatitis. JAMA Dermatol. 2014; 150:254–259.
Article18. Cole C, Kroboth K, Schurch NJ, Sandilands A, Sherstnev A, O'Regan GM, et al. Filaggrin-stratified transcriptomic analysis of pediatric skin identifies mechanistic pathways in patients with atopic dermatitis. J Allergy Clin Immunol. 2014; 134:82–91.
Article19. Ewald DA, Malajian D, Krueger JG, Workman CT, Wang T, Tian S, et al. Meta-analysis derived atopic dermatitis (MADAD) transcriptome defines a robust AD signature highlighting the involvement of atherosclerosis and lipid metabolism pathways. BMC Med Genomics. 2015; 8:60.
Article20. Ashley SE, Tan HT, Vuillermin P, Dharmage SC, Tang ML, Koplin J, et al. The skin barrier function gene SPINK5 is associated with challenge-proven IgE-mediated food allergy in infants. Allergy. 2017; 72:1356–1364.21. Marenholz I, Esparza-Gordillo J, Lee YA. The genetics of the skin barrier in eczema and other allergic disorders. Curr Opin Allergy Clin Immunol. 2015; 15:426–434.
Article22. Hirota T, Nakayama T, Sato S, Yanagida N, Matsui T, Sugiura S, et al. Association study of childhood food allergy with genome-wide association studies-discovered loci of atopic dermatitis and eosinophilic esophagitis. J Allergy Clin Immunol. 2017; 140:1713–1716.
Article23. Kelleher M, Dunn-Galvin A, Hourihane JO, Murray D, Campbell LE, McLean WH, et al. Skin barrier dysfunction measured by transepidermal water loss at 2 days and 2 months predates and predicts atopic dermatitis at 1 year. J Allergy Clin Immunol. 2015; 135:930–935.e1.24. Lack G. Update on risk factors for food allergy. J Allergy Clin Immunol. 2012; 129:1187–1197.
Article25. Strid J, Hourihane J, Kimber I, Callard R, Strobel S. Disruption of the stratum corneum allows potent epicutaneous immunization with protein antigens resulting in a dominant systemic Th2 response. Eur J Immunol. 2004; 34:2100–2109.
Article26. Spergel JM, Mizoguchi E, Brewer JP, Martin TR, Bhan AK, Geha RS. Epicutaneous sensitization with protein antigen induces localized allergic dermatitis and hyperresponsiveness to methacholine after single exposure to aerosolized antigen in mice. J Clin Invest. 1998; 101:1614–1622.
Article27. Fallon PG, Sasaki T, Sandilands A, Campbell LE, Saunders SP, Mangan NE, et al. A homozygous frameshift mutation in the mouse FLG gene facilitates enhanced percutaneous allergen priming. Nat Genet. 2009; 41:602–608.
Article28. Bartnikas LM, Gurish MF, Burton OT, Leisten S, Janssen E, Oettgen HC, et al. Epicutaneous sensitization results in IgE-dependent intestinal mast cell expansion and food-induced anaphylaxis. J Allergy Clin Immunol. 2013; 131:451–460.e1-6.
Article29. Noti M, Kim BS, Siracusa MC, Rak GD, Kubo M, Moghaddam AE, et al. Exposure to food allergens through inflamed skin promotes intestinal food allergy through the thymic stromal lymphopoietin-basophil axis. J Allergy Clin Immunol. 2014; 133:1390–1399. 1399.e1–1396.
Article30. Hussain M, Borcard L, Walsh KP, Pena Rodriguez M, Mueller C, Kim BS, et al. Basophil-derived IL-4 promotes epicutaneous antigen sensitization concomitant with the development of food allergy. J Allergy Clin Immunol. 2018; 141:223–234.e5.
Article31. Galand C, Leyva-Castillo JM, Yoon J, Han A, Lee MS, McKenzie AN, et al. IL-33 promotes food anaphylaxis in epicutaneously sensitized mice by targeting mast cells. J Allergy Clin Immunol. 2016; 138:1356–1366.
Article32. Kelleher MM, Dunn-Galvin A, Gray C, Murray DM, Kiely M, Kenny L, et al. Skin barrier impairment at birth predicts food allergy at 2 years of age. J Allergy Clin Immunol. 2016; 137:1111–1116.e8.33. Lack G, Fox D, Northstone K, Golding J. Avon Longitudinal Study of Parents and Children Study Team. Factors associated with the development of peanut allergy in childhood. N Engl J Med. 2003; 348:977–985.
Article34. Boussault P, Léauté-Labrèze C, Saubusse E, Maurice-Tison S, Perromat M, Roul S, et al. Oat sensitization in children with atopic dermatitis: prevalence, risks and associated factors. Allergy. 2007; 62:1251–1256.
Article35. Lowe AJ, Abramson MJ, Hosking CS, Carlin JB, Bennett CM, Dharmage SC, et al. The temporal sequence of allergic sensitization and onset of infantile eczema. Clin Exp Allergy. 2007; 37:536–542.
Article36. Martin PE, Eckert JK, Koplin JJ, Lowe AJ, Gurrin LC, Dharmage SC, et al. Which infants with eczema are at risk of food allergy? Results from a population-based cohort. Clin Exp Allergy. 2015; 45:255–264.
Article37. Tauber M, Balica S, Hsu CY, Jean-Decoster C, Lauze C, Redoules D, et al. Staphylococcus aureus density on lesional and nonlesional skin is strongly associated with disease severity in atopic dermatitis. J Allergy Clin Immunol. 2016; 137:1272–1274.e3.38. Czarnowicki T, Krueger JG, Guttman-Yassky E. Skin barrier and immune dysregulation in atopic dermatitis: an evolving story with important clinical implications. J Allergy Clin Immunol Pract. 2014; 2:371–379.
Article39. Forbes-Blom E, Camberis M, Prout M, Tang SC, Le Gros G. Staphylococcal-derived superantigen enhances peanut induced Th2 responses in the skin. Clin Exp Allergy. 2012; 42:305–314.
Article40. Jones AL, Curran-Everett D, Leung DY. Food allergy is associated with Staphylococcus aureus colonization in children with atopic dermatitis. J Allergy Clin Immunol. 2016; 137:1247–1248.e3.41. Lowe AJ, Angelica B, Su J, Lodge CJ, Hill DJ, Erbas B, et al. Age at onset and persistence of eczema are related to subsequent risk of asthma and hay fever from birth to 18 years of age. Pediatr Allergy Immunol. 2017; 28:384–390.42. Gustafsson D, Sjöberg O, Foucard T. Development of allergies and asthma in infants and young children with atopic dermatitis--a prospective follow-up to 7 years of age. Allergy. 2000; 55:240–245.43. Strachan DP, Butland BK, Anderson HR. Incidence and prognosis of asthma and wheezing illness from early childhood to age 33 in a national British cohort. BMJ. 1996; 312:1195–1199.
Article44. Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ, et al. Asthma and wheezing in the first six years of life. N Engl J Med. 1995; 332:133–138.
Article45. Ferreira MA, Vonk JM, Baurecht H, Marenholz I, Tian C, Hoffman JD, et al. Shared genetic origin of asthma, hay fever and eczema elucidates allergic disease biology. Nat Genet. 2017; 49:1752–1757.46. Weidinger S, Willis-Owen SA, Kamatani Y, Baurecht H, Morar N, Liang L, et al. A genome-wide association study of atopic dermatitis identifies loci with overlapping effects on asthma and psoriasis. Hum Mol Genet. 2013; 22:4841–4856.
Article47. Marenholz I, Esparza-Gordillo J, Rüschendorf F, Bauerfeind A, Strachan DP, Spycher BD, et al. Meta-analysis identifies seven susceptibility loci involved in the atopic march. Nat Commun. 2015; 6:8804.
Article48. Johansson E, Biagini Myers JM, Martin LJ, He H, Pilipenko V, Mersha T, et al. KIF3A genetic variation is associated with pediatric asthma in the presence of eczema independent of allergic rhinitis. J Allergy Clin Immunol. 2017; 140:595–598.e5.
Article49. Akei HS, Brandt EB, Mishra A, Strait RT, Finkelman FD, Warrier MR, et al. Epicutaneous aeroallergen exposure induces systemic TH2 immunity that predisposes to allergic nasal responses. J Allergy Clin Immunol. 2006; 118:62–69.
Article50. Cianferoni A, Spergel J. The importance of TSLP in allergic disease and its role as a potential therapeutic target. Expert Rev Clin Immunol. 2014; 10:1463–1474.
Article51. Han H, Xu W, Headley MB, Jessup HK, Lee KS, Omori M, et al. Thymic stromal lymphopoietin (TSLP)-mediated dermal inflammation aggravates experimental asthma. Mucosal Immunol. 2012; 5:342–351.
Article52. Jiang H, Hener P, Li J, Li M. Skin thymic stromal lymphopoietin promotes airway sensitization to inhalant house dust mites leading to allergic asthma in mice. Allergy. 2012; 67:1078–1082.
Article53. Dunkin D, Berin MC, Mayer L. Allergic sensitization can be induced via multiple physiologic routes in an adjuvant-dependent manner. J Allergy Clin Immunol. 2011; 128:1251–1258.e2.
Article54. Yagami A, Aihara M, Ikezawa Z, Hide M, Kishikawa R, Morita E, et al. Outbreak of immediate-type hydrolyzed wheat protein allergy due to a facial soap in Japan. J Allergy Clin Immunol. 2017; 140:879–881.e7.
Article55. Deckers J, Sichien D, Plantinga M, Van Moorleghem J, Vanheerswynghels M, Hoste E, et al. Epicutaneous sensitization to house dust mite allergen requires interferon regulatory factor 4-dependent dermal dendritic cells. J Allergy Clin Immunol. 2017; 140:1364–1377.e2.
Article56. Stremnitzer C, Manzano-Szalai K, Starkl P, Willensdorfer A, Schrom S, Singer J, et al. Epicutaneously applied Der p 2 induces a strong TH 2-biased antibody response in C57BL/6 mice, independent of functional TLR4. Allergy. 2014; 69:741–751.57. Walker MT, Green JE, Ferrie RP, Queener AM, Kaplan MH, Cook-Mills JM. Mechanism for initiation of food allergy: dependence on skin barrier mutations and environmental allergen costimulation. J Allergy Clin Immunol. 2018; 141:1711–1725.e9.
Article58. Horimukai K, Morita K, Narita M, Kondo M, Kitazawa H, Nozaki M, et al. Application of moisturizer to neonates prevents development of atopic dermatitis. J Allergy Clin Immunol. 2014; 134:824–830.e6.
Article59. Simpson EL, Chalmers JR, Hanifin JM, Thomas KS, Cork MJ, McLean WH, et al. Emollient enhancement of the skin barrier from birth offers effective atopic dermatitis prevention. J Allergy Clin Immunol. 2014; 134:818–823.
Article60. Glatz M, Jo JH, Kennedy EA, Polley EC, Segre JA, Simpson EL, et al. Emollient use alters skin barrier and microbes in infants at risk for developing atopic dermatitis. PLoS One. 2018; 13:e0192443.
Article61. Lowe AJ, Su JC, Allen KJ, Abramson MJ, Cranswick N, Robertson CF, et al. A randomized trial of a barrier lipid replacement strategy for the prevention of atopic dermatitis and allergic sensitization: the PEBBLES pilot study. Br J Dermatol. 2018; 178:e19–21.
Article62. Chalmers JR, Haines RH, Mitchell EJ, Thomas KS, Brown SJ, Ridd M, et al. Effectiveness and cost-effectiveness of daily all-over-body application of emollient during the first year of life for preventing atopic eczema in high-risk children (The BEEP trial): protocol for a randomised controlled trial. Trials. 2017; 18:343.
Article63. Lowe AJ, Leung DY, Tang ML, Su JC, Allen KJ. The skin as a target for prevention of the atopic march. Ann Allergy Asthma Immunol. 2018; 120:145–151.
Article64. Fiocchi A, Pawankar R, Cuello-Garcia C, Ahn K, Al-Hammadi S, Agarwal A, et al. World Allergy Organization-McMaster University Guidelines for Allergic Disease Prevention (GLAD-P): probiotics. World Allergy Organ J. 2015; 8:4.
Article65. Ohya Y. Prevention of Allergy via Cutaneous Intervention (PACI) study. Trial registration ID: UMIN000028043 [Internet]. Tokyo: National Center for Child Health and Development;2017. cited 2018 Jan 7. Available from: http://paci-study.jp/english.html.66. Du Toit G, Roberts G, Sayre PH, Bahnson HT, Radulovic S, Santos AF, et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015; 372:803–813.
Article67. Natsume O, Kabashima S, Nakazato J, Yamamoto-Hanada K, Narita M, Kondo M, et al. Two-step egg introduction for prevention of egg allergy in high-risk infants with eczema (PETIT): a randomised, double-blind, placebo-controlled trial. Lancet. 2017; 389:276–286.
Article68. Beasley R, Semprini A, Mitchell EA. Risk factors for asthma: is prevention possible? Lancet. 2015; 386:1075–1085.
Article69. Tsilochristou OA, Douladiris N, Makris M, Papadopoulos NG. Pediatric allergic rhinitis and asthma: can the march be halted? Paediatr Drugs. 2013; 15:431–440.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Antigen Sensitization and Development of Respiratory Allergy Disease on Severity of Atopic Dermatitis
- Advances In the Pathophysiology of Atopic Dermatitis
- A Case of Persistent Cow's Milk Allergy Accompanying Atopic Dermatitis
- A Case of Atopic Dermatitis due to Peanut Allergy
- Update on management of pediatric atopic dermatitis