Ann Surg Treat Res.
2018 Dec;95(6):333-339. 10.4174/astr.2018.95.6.333.
Long-term outcomes after stent insertion in patients with early and late hepatic vein outflow obstruction after living donor liver transplantation
- Affiliations
-
- 1Department of Surgery-Transplantation, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jongman94.kim@samsung.com
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2426765
- DOI: http://doi.org/10.4174/astr.2018.95.6.333
Abstract
- PURPOSE
The purpose of this study was to describe the long-term effects of stenting in patients with hepatic venous outflow obstruction (HVOO), who underwent living donor liver transplantation (LDLT).
METHODS
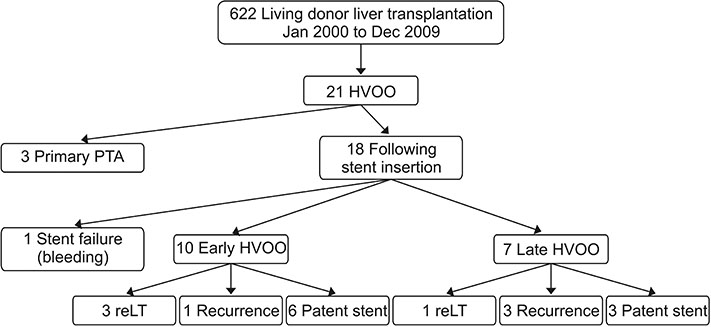
Between January 2000 and December 2009, 622 adult patients underwent LDLT at our hospital, and of these patients, 21 (3.3%) were diagnosed with HVOO; among these patients, 17 underwent stenting. The patients were divided into early or late groups according to the time of their HVOO diagnoses (cutoff: 60 days after liver transplantation).
RESULTS
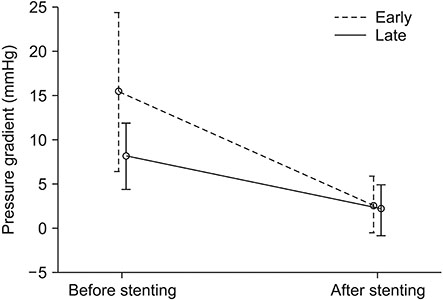
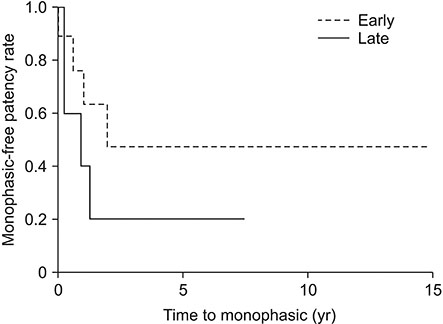
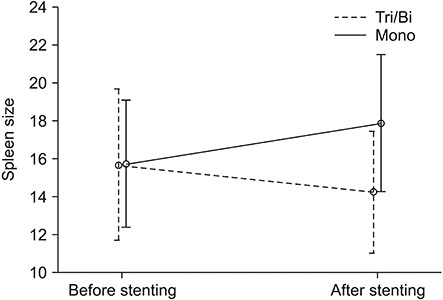
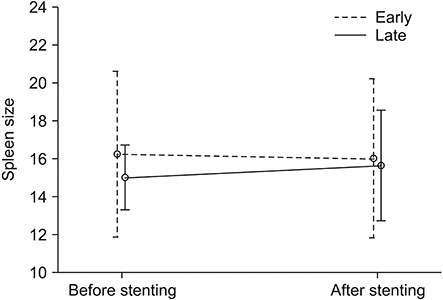
The median follow-up period was 54.2 months (range, 0.5-192.4 months). Stent insertion was successful in 8 of 10 patients in the early group and 6 of 7 in the late group. The 5-year primary patency rates were 46% and 20%, respectively. In both groups, patients with recurrent HVOO at the beginning showed kinking confirmed by venography. Patients who carried their stents for more than 3 years maintained long-term patency. There was no significant difference in spleen size between groups; however, when the groups were compared according to whether they maintained patency, spleens tended to be smaller in the patency-maintained group.
CONCLUSION
Unlike stenosis, if kinking is confirmed on venography, stenting is not feasible in the long term for patients with LDLT.
Keyword
MeSH Terms
Figure
Reference
-
1. Duffy JP, Kao K, Ko CY, Farmer DG, McDiarmid SV, Hong JC, et al. Long-term patient outcome and quality of life after liver transplantation: analysis of 20-year survivors. Ann Surg. 2010; 252:652–661.2. Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018; 68:723–750.
Article3. Kim JM, Lee KW, Song GW, Jung BH, Lee HW, Yi NJ, et al. Outcomes for patients with HCV after liver transplantation in Korea: a multicenter study. Ann Surg Treat Res. 2016; 90:36–42.
Article4. Jain A, Reyes J, Kashyap R, Dodson SF, Demetris AJ, Ruppert K, et al. Long-term survival after liver transplantation in 4,000 consecutive patients at a single center. Ann Surg. 2000; 232:490–500.
Article5. Adam R, Karam V, Delvart V, O'Grady J, Mirza D, Klempnauer J, et al. Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). J Hepatol. 2012; 57:675–688.
Article6. Hampe T, Dogan A, Encke J, Mehrabi A, Schemmer P, Schmidt J, et al. Biliary complications after liver transplantation. Clin Transplant. 2006; 20:Suppl 17. 93–96.
Article7. Taner T. Liver transplantation: rejection and tolerance. Liver Transpl. 2017; 23(S1):S85–S88.
Article8. Piardi T, Lhuaire M, Bruno O, Memeo R, Pessaux P, Kianmanesh R, et al. Vascular complications following liver transplantation: a literature review of advances in 2015. World J Hepatol. 2016; 8:36–57.
Article9. Ko GY, Sung KB, Yoon HK, Kim KR, Kim JH, Gwon DI, et al. Early posttransplant hepatic venous outflow obstruction: long-term efficacy of primary stent placement. Liver Transpl. 2008; 14:1505–1511.
Article10. Umehara M, Narumi S, Sugai M, Toyoki Y, Ishido K, Kudo D, et al. Hepatic venous outflow obstruction in living donor liver transplantation: balloon angioplasty or stent placement? Transplant Proc. 2012; 44:769–771.
Article11. Chu HH, Yi NJ, Kim HC, Lee KW, Suh KS, Jae HJ, et al. Longterm outcomes of stent placement for hepatic venous outflow obstruction in adult liver transplantation recipients. Liver Transpl. 2016; 22:1554–1561.
Article12. Chen YS, Chen CL, Liu PP, Wang CC, Chiang YC, Huang TL, et al. Successful treatment of hepatic vein thrombosis following reduced-size liver transplantation. Transplant Proc. 1998; 30:3203–3204.
Article13. Someda H, Moriyasu F, Fujimoto M, Hamato N, Nabeshima M, Nishikawa K, et al. Vascular complications in living related liver transplantation detected with intraoperative and postoperative Doppler US. J Hepatol. 1995; 22:623–632.
Article14. Haga J, Shimazu M, Wakabayashi G, Tanabe M, Kawachi S, Fuchimoto Y, et al. Liver regeneration in donors and adult recipients after living donor liver transplantation. Liver Transpl. 2008; 14:1718–1724.
Article15. Darcy MD. Mnagement of venous outflow complications after liver transplantation. Tech Vasc Interv Radiol. 2007; 10:240–245.16. Cirera I, Navasa M, Rimola A, García-Pagán JC, Grande L, Garcia-Valdecasas JC, et al. Ascites after liver transplantation. Liver Transpl. 2000; 6:157–162.
Article17. Chezmar JL, Redvanly RD, Nelson RC, Henderson JM. Persistence of portosystemic collaterals and splenomegaly on CT after orthotopic liver transplantation. AJR Am J Roentgenol. 1992; 159:317–320.
Article18. Chikamori F, Nishida S, Selvaggi G, Tryphonopoulos P, Moon JI, Levi DM, et al. Effect of liver transplantation on spleen size, collateral veins, and platelet counts. World J Surg. 2010; 34:320–326.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Late Hepatic Venous Outflow Obstruction Following Inferior Vena Cava Stenting in Patient with Deceased Donor Liver Transplantation Using Modified Piggyback Technique
- Graft outflow vein unification venoplasty with superficial left hepatic vein branch in pediatric living donor liver transplantation using a left lateral section graft
- Liver retransplantation for adult recipients
- Third retransplantation using a whole liver graft for late graft failure from hepatic vein stent stenosis in a pediatric patient who underwent split liver retransplantation
- Hepatic Vein Reconstruction for Living Donor Liver Transplantation using a Modified Right lobe Graft: Experience at Asan Medical Center and focused on Middle Hepatic Vein Reconstruction