Ann Surg Treat Res.
2018 Dec;95(6):312-318. 10.4174/astr.2018.95.6.312.
Effects of acute normovolemic hemodilution on healing of gastric anastomosis in rats
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Hanyang University College of Medicine, Seoul, Korea.
- 2Department of Pathology, Hanyang University College of Medicine, Seoul, Korea.
- 3Department of Surgery, Hanyang University College of Medicine, Seoul, Korea. crane87@hanyang.ac.kr
- KMID: 2426762
- DOI: http://doi.org/10.4174/astr.2018.95.6.312
Abstract
- PURPOSE
Acute normovolemic hemodilution (ANH) is an autologous transfusion method, using blood collected during surgery, to reduce the need for allogeneic blood transfusion. ANH is controversial because it may lead to various complications. Among the possible complications, anastomotic leakage is one that would have a significant effect on the operation outcome. However, the relationship between ANH and anastomotic site healing requires additional research. Therefore, we conducted this prospective study of ANH, comparing it with standard intraoperative management, undergoing gastric anastomosis in rats.
METHODS
Sixteen Sprague-Dawley rats were randomly assigned to three groups: group A, surgery with ANH; group N, surgery with standard intraoperative management; and group C, sham surgery with standard intraoperative management. ANH was performed in group A animals by, removing 5.8-6.6 mL of blood and replacing it with 3 times as much crystalloid. All rats were enthanized on postoperative day 6, and histopathologic analyses were performed.
RESULTS
The mean hematocrit values, after hemodilution were 22.0% (range, 18.0%-29.0%), group A; 33.0% (29.0%-35.0%), group N; and 32.5% (29.0%-34.0%), group C. There were significant differences between groups A and N (P = 0.019, P = 0.009, P = 0.004, P = 0.039, and P = 0.027), and between groups N and C (P = 0.006, P = 0.027, P = 0.04, P = 0.008, and P = 0.009) with respect to inflammatory cell numbers, neovascularization, fibroblast numbers, edema and necrosis, respectively; there were no differences between groups A and N.
CONCLUSION
In rat model, anastomotic complications did not increase in the ANH group, compared with the standard intraoperative management group.
MeSH Terms
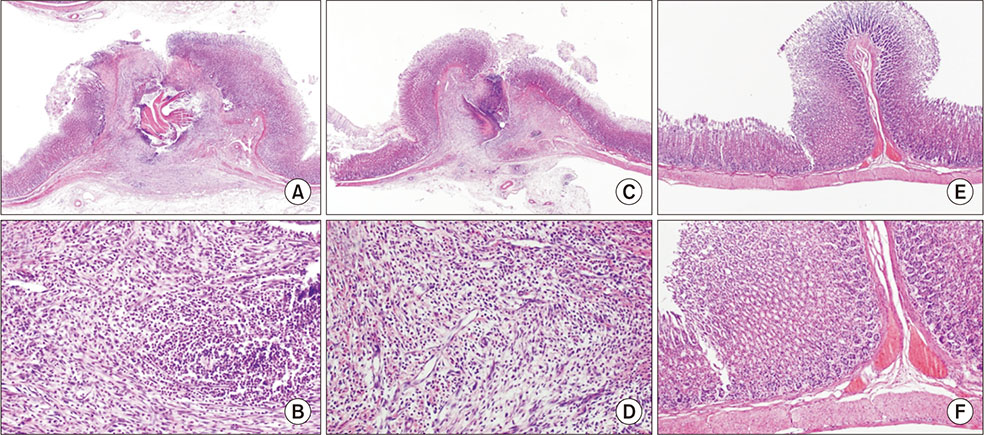
Figure
Reference
-
1. Frank SM, Savage WJ, Rothschild JA, Rivers RJ, Ness PM, Paul SL, et al. Variability in blood and blood component utilization as assessed by an anesthesia information management system. Anesthesiology. 2012; 117:99–106.
Article2. Spinella PC, Reddy HL, Jaffe JS, Cap AP, Goodrich RP. Fresh whole blood use for hemorrhagic shock: preserving benefit while avoiding complications. Anesth Analg. 2012; 115:751–758.3. Vincent JL, Lelubre C. Preoperative transfusions to limit the deleterious effects of blood transfusions. Anesthesiology. 2012; 116:513–514.
Article4. Inaba K, Branco BC, Rhee P, Blackbourne LH, Holcomb JB, Teixeira PG, et al. Impact of plasma transfusion in trauma patients who do not require massive transfusion. J Am Coll Surg. 2010; 210:957–965.
Article5. Hendrickson JE, Hillyer CD. Noninfectious serious hazards of transfusion. Anesth Analg. 2009; 108:759–769.
Article6. Glance LG, Dick AW, Mukamel DB, Fleming FJ, Zollo RA, Wissler R, et al. Association between intraoperative blood transfusion and mortality and morbidity in patients undergoing noncardiac surgery. Anesthesiology. 2011; 114:283–292.
Article7. Goodnough LT, Brecher ME, Kanter MH, AuBuchon JP. Transfusion medicine. First of two parts--blood transfusion. N Engl J Med. 1999; 340:438–447.8. Jarnagin WR, Gonen M, Maithel SK, Fong Y, D'Angelica MI, Dematteo RP, et al. A prospective randomized trial of acute normovolemic hemodilution compared to standard intraoperative management in patients undergoing major hepatic resection. Ann Surg. 2008; 248:360–369.
Article9. Sanders G, Mellor N, Rickards K, Rushton A, Christie I, Nicholl J, et al. Prospective randomized controlled trial of acute normovolaemic haemodilution in major gastrointestinal surgery. Br J Anaesth. 2004; 93:775–781.
Article10. Mandai R, Eguchi Y, Tanaka M, Sai Y, Nosaka S. Effects of profound hemodilution on small-intestinal wound healing in rabbits. J Surg Res. 2001; 99:107–113.
Article11. Fischer M, Matsuo K, Gonen M, Grant F, Dematteo RP, D'Angelica MI, et al. Relationship between intraoperative fluid administration and perioperative outcome after pancreaticoduodenectomy: results of a prospective randomized trial of acute normovolemic hemodilution compared with standard intraoperative management. Ann Surg. 2010; 252:952–958.12. Alves A, Panis Y, Pocard M, Regimbeau JM, Valleur P. Management of anastomotic leakage after nondiverted large bowel resection. J Am Coll Surg. 1999; 189:554–559.
Article13. Goodnough LT, Brecher ME, Kanter MH, AuBuchon JP. Transfusion medicine. Second of two parts--blood conservation. N Engl J Med. 1999; 340:525–533.14. Wolowczyk L, Lewis DR, Nevin M, Smith FC, Baird RN, Lamont PM. The effect of acute normovolaemic haemodilution on blood transfusion requirements in abdominal aortic aneurysm repair. Eur J Vasc Endovasc Surg. 2001; 22:361–364.
Article15. Jeon YB, Yun S, Choi D. Transfusion free radical antegrade modular pancreaticosplenectomy of metastatic neuroendocrine tumor of the pancreas in Jehovah's Witness patient. Ann Surg Treat Res. 2015; 88:106–110.
Article16. Segal JB, Blasco-Colmenares E, Norris EJ, Guallar E. Preoperative acute normovolemic hemodilution: a meta-analysis. Transfusion. 2004; 44:632–644.
Article17. Lipska MA, Bissett IP, Parry BR, Merrie AE. Anastomotic leakage after lower gastrointestinal anastomosis: men are at a higher risk. ANZ J Surg. 2006; 76:579–585.
Article18. Konishi T, Watanabe T, Kishimoto J, Nagawa H. Risk factors for anastomotic leakage after surgery for colorectal cancer: results of prospective surveillance. J Am Coll Surg. 2006; 202:439–444.
Article19. Gorissen KJ, Benning D, Berghmans T, Snoeijs MG, Sosef MN, Hulsewe KW, et al. Risk of anastomotic leakage with non-steroidal anti-inflammatory drugs in colorectal surgery. Br J Surg. 2012; 99:721–727.
Article20. Platell C, Barwood N, Dorfmann G, Makin G. The incidence of anastomotic leaks in patients undergoing colorectal surgery. Colorectal Dis. 2007; 9:71–79.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraoperative Normovolemic Hemodilution in Patients Undergonig Posterolateral Spinal Fusion: Safety and Efficacy
- Acute normovolemic hemodilution for a patient with secondary polycythemia undergoing aortic valve replacement due to severe aortic stenosis - A case report -
- The Effects of Acute Normovolemic Anemia Induced by Hemodilution on Tissue Oxygenation in Dogs: A Comparison of Systemic Oxygen Consumption, Arterial Lactate, Arterial Ketone Body Ratio and Gastric Intramucosal pH
- An Experiment on Intraoperative Autotransgusion and Normovolemic Hemodilution with hartmann`s Solution and Rheomacrodex
- Acute Normovolemic Hemodilution Decreases Transfusion Requirement in Spinal Surgery