J Korean Med Assoc.
2018 Nov;61(11):687-698. 10.5124/jkma.2018.61.11.687.
Analysis of factors affecting antibiotic use at hospitals and clinics based on the defined daily dose
- Affiliations
-
- 1Pharmaceutical & Medical Technology Research Team, Department of Research, Health Insurance Review & Assessment Service, Wonju, Korea. sttone@hira.or.kr
- 2Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea. ahnhann@gmail.com
- KMID: 2426479
- DOI: http://doi.org/10.5124/jkma.2018.61.11.687
Abstract
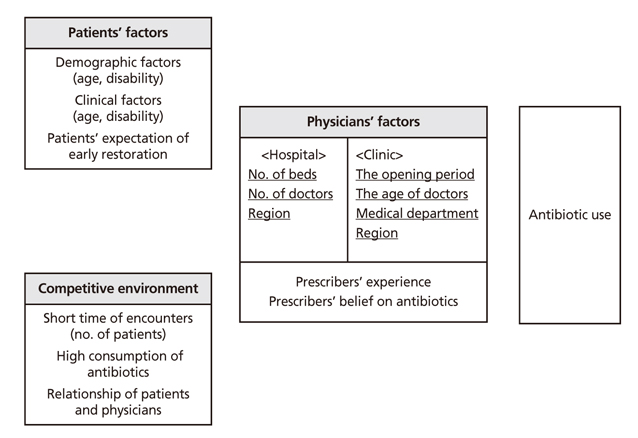
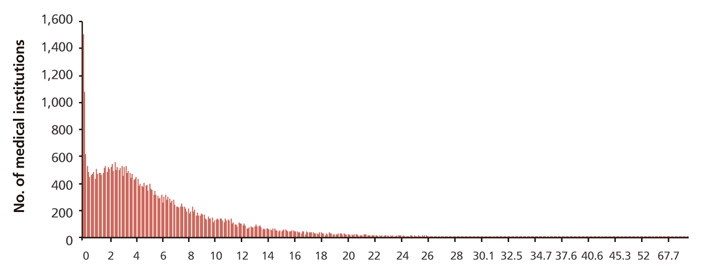
- Inappropriate antibiotic use significantly contributes to antibiotic resistance, resulting in reduced antibiotic efficacy and an increased burden of disease. The objective of this study was to investigate the characteristics of prescribers whose antibiotics use was high and to explore factors affecting the use of antibiotics by medical institutions. This study analyzed the National Health Insurance claims data from 2015. Antibiotic prescription data were analyzed in terms of the number of defined daily doses per 1,000 patients per day, according to the World Health Organization anatomical-therapeutic-chemical classification and methodologies for measuring the defined daily dose. We investigated the characteristics of prescribers and medical institutions with high antibiotic use. Multivariate regression analyses were performed on the basis of characteristics of the medical institution (number of patients, type of medical institution [hospital or clinic], age of the physician, etc.). The number of patients and number of beds were found to be significant factors affecting antibiotic use in hospitals, and the number of patients, region, and medical department were significant factors affecting antibiotic use at the level of medical institutions. These findings are expected to help policy-makers to better target future interventions to promote prudent antibiotic prescription.
Keyword
MeSH Terms
Figure
Reference
-
1. Shin E. Antimicrobials and antimicrobial resistant superbac-teria. Ewha Med J. 2017; 40:99–103.
Article2. Torjesen I. UK spearheads efforts to combat rising threat of antibiotic resistance. BMJ. 2014; 349:g4418.
Article3. O'Neill J. Tackling drug-resistant infections globally: final report and recommendation. London: HM Government and Wellcome Trust;2016.4. The White House. National action plan for combating antibio-tic-resistance bacteria. Washington, DC: The White House;2014.5. Centers for Disease Control and Prevention. Antibiotic resis-tance threats in the United States. Atlanta: Centers for Disease Control and Prevention;2013.6. Organization for Economic Cooperation and Development. Antimicrobial resistance in G7 countries and beyond: econo-mic issues, policies and options for action. Paris: Organization for Economic Cooperation and Development;2015.7. Ministry of Health and Welfare. National plan on prevention of infection disease [Internet]. Sejong: Ministry of Health and Welfare;2018. cited 2018 Jul 7. Available from: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=345237.8. Hooper DC, DeMaria A, Limbago BM, O'Brien TF, McCau-ghey B. Antibiotic resistance: how serious is the problem, and what can be done? Clin Chem. 2012; 58:1182–1186.
Article9. Word Health Organization. Country progress in the imple-mentation of the global action plan on antimicrobial resis-tance: WHO, FAO and OIE global tripartite database [Internet]. Geneva: Word Health Organization;cited 2018 Oct 30. Available from: http://www.who.int/antimicrobial-resistance/global-action-plan/database/en/.10. Kim DS, Bae G, Yoo SY, Kang M. Between government policy, clinical autonomy, and market demands: a qualitative study of the impact of the Prescribing Analysis System on behavior of physicians in South Korea. BMC Health Serv Res. 2015; 15:397.
Article11. Kim SK, Kim HE, Back MS, Lee SH. The effect of public report on antibiotics prescribing rate. Korean J Clin Pharm. 2010; 20:242–247.12. Park J, Han E, Lee SO, Kim DS. Antibiotic use in South Korea from 2007 to 2014: a health insurance database-generated time series analysis. PLoS One. 2017; 12:e0177435.
Article13. Cars O, Molstad S, Melander A. Variation in antibiotic use in the European Union. Lancet. 2001; 357:1851–1853.
Article14. Wood F, Phillips C, Brookes-Howell L, Hood K, Verheij T, Coenen S, Little P, Melbye H, Godycki-Cwirko M, Jakobsen K, Worby P, Goossens H, Butler CC. Primary care clinicians' perceptions of antibiotic resistance: a multi-country qualitative interview study. J Antimicrob Chemother. 2013; 68:237–243.
Article15. Brookes-Howell L, Hood K, Cooper L, Little P, Verheij T, Coenen S, Godycki-Cwirko M, Melbye H, Borras-Santos A, Worby P, Jakobsen K, Goossens H, Butler CC. Understanding variation in primary medical care: a nine-country qualitative study of cliniciansXMLLink_XYZ accounts of the non-clinical factors that shape antibiotic prescribing decisions for lower respiratory tract infection. BMJ Open. 2012; 08. 22. [Epub]. DOI: 10.1136/bmjopen-2011-000796.16. Trepka MJ, Belongia EA, Chyou PH, Davis JP, Schwartz B. The effect of a community intervention trial on parental know-ledge and awareness of antibiotic resistance and appropriate antibiotic use in children. Pediatrics. 2001; 107:E6.
Article17. Mangione-Smith R, McGlynn EA, Elliott MN, McDonald L, Franz CE, Kravitz RL. Parent expectations for antibiotics, physician-parent communication, and satisfaction. Arch Pediatr Adolesc Med. 2001; 155:800–806.
Article18. Cho H, Park J, Kim DS. A Qualitative study of antibiotic prescribing decision of physicians and strategy of antibiotics prescription. Korean J Health Promot. 2016; 16:203–213.
Article19. Choi WJ, Yim E, Kim TH, Suh HS, Choi KC, Chung W. Analysis of factors related to the prescription of antibiotics for the acute upper respiratory infection. Health Policy Manag. 2015; 25:256–263.
Article20. Kim Y, Lee S, Park S, Na HO. Tchoe B. Outpatient antibiotic prescription patterns for respiratory tract infections of infants. Health Policy Manag. 2015; 25:323–332.
Article21. Joo YS, Cho GY. Outlier detection and treatment in industrial sampling survey. J Korean Data Inf Sci Soc. 2016; 27:131–142.
Article22. Tukey JW. Exploratory data analysis. London: Adiison-Wesley;1977.23. WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment 2014. Oslo: WHO Collaborating Centre for Drug Statistics Methodology;2014.24. Lusini G, Lapi F, Sara B, Vannacci A, Mugelli A, Kragstrup J, Bjerrum L. Antibiotic prescribing in paediatric populations: a comparison between Viareggio, Italy and Funen, Denmark. Eur J Public Health. 2009; 19:434–438.
Article25. World Health Organization. Republic of Korea, National action plan on antimicrobial resistance (2016-2020) [Internet]. Geneva: World Health Organization;2016. cited 2018 Jul 7. Available from: http://www.who.int/antimicrobial-resistance/global-action-plan/library/en.26. Kim DS, Park J, Lee GW, Choi JW, Lee EJ, Jeon SY. Analysis of antibiotic use and consideration of the association between antibiotic use and resistance. Wonju: Health Insurance Review and Assessment Service;2017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Affecting the Preference for Hospitals Over Clinics in Primary Care in Korea
- Factors affecting the rate of antibiotic prescription in dental practices
- Current Status of Subspecialists Training Programs and Factors Affecting Subspecialists' Job Selection after Training
- Nurse Staffing Levels and Proportion of Hospitals and Clinics Meeting the Legal Standard for Nurse Staffing for 1996~2013
- Factors Affecting Productivity of Medical Personnel in Training Hospital