J Clin Neurol.
2012 Jun;8(2):116-122.
Mechanism of Medullary Infarction Based on Arterial Territory Involvement
- Affiliations
-
- 1Department of Neurology, Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea. jhheo@yuhs.ac
- 2Department of Preventive Medicine and Public Health, Yonsei University College of Medicine, Seoul, Korea.
Abstract
- BACKGROUND AND PURPOSE
The blood supply to the medulla oblongata is distinct from that of other areas of the brainstem, and thus the mechanism underlying medullary infarctions may be distinct. However, few studies have investigated this.
METHODS
Of 3833 stroke patients who were on the stroke registry between February 1999 and April 2008, those with medullary infarctions demonstrated on diffusion-weighted magnetic resonance imaging were enrolled. We analyzed the topography, the involved arterial territories, and the etiologic mechanisms of the lesions.
RESULTS
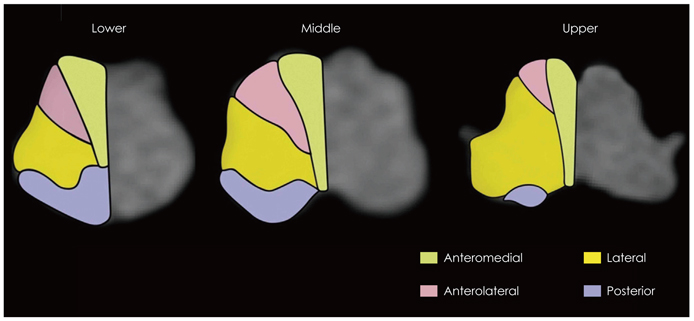
In total, 142 patients were enrolled in the study. Bilateral medullary infarctions were rare (2.2%). Lesions involving the anteromedial or lateral territories were common in the upper medulla oblongata, whereas lateral territorial involvements were common in the middle and lower regions of the medulla oblongata. Significant stenosis (>50%) or occlusion of the vertebral artery was common (52.2%). Among stroke subtypes, large-artery atherosclerosis was most common (34.5%), while lacunae and cardioembolism were rare (3.5% and 4.2%, respectively). Vertebral artery dissection was frequent. The stroke mechanisms differed with the involved vascular territories. Large-artery atherosclerosis produced lesions in the lateral, anteromedial, and posterior territories. None of the cardioembolisms or other etiologies involved anteromedial or anterolateral territories, but all involved the lateral and/or posterior territories. Lacunar infarction was found only in the anteromedial and anterolateral territories.
CONCLUSIONS
The topography and mechanisms of infarctions involving the medulla oblongata are different with the involved arterial territories. These findings may be associated with the distinct pattern of arterial supply to the medulla oblongata.
Keyword
MeSH Terms
Figure
Reference
-
1. Sacco RL, Freddo L, Bello JA, Odel JG, Onesti ST, Mohr JP. Wallenberg's lateral medullary syndrome. Clinical-magnetic resonance imaging correlations. Arch Neurol. 1993. 50:609–614.2. Kim JS, Lee JH, Choi CG. Patterns of lateral medullary infarction: vascular lesion-magnetic resonance imaging correlation of 34 cases. Stroke. 1998. 29:645–652.3. Kim JS, Choi-Kwon S. Sensory sequelae of medullary infarction: differences between lateral and medial medullary syndrome. Stroke. 1999. 30:2697–2703.4. Kwon M, Lee JH, Kim JS. Dysphagia in unilateral medullary infarction: lateral vs medial lesions. Neurology. 2005. 65:714–718.
Article5. Kim JS. Pure lateral medullary infarction: clinical-radiological correlation of 130 acute, consecutive patients. Brain. 2003. 126:1864–1872.
Article6. Duvernoy HM. Human Brain Stem Vessels. 1999. 2nd ed. New York: Springer.7. Tatu L, Moulin T, Bogousslavsky J, Duvernoy H. Arterial territories of human brain: brainstem and cerebellum. Neurology. 1996. 47:1125–1135.8. Kim JS, Han YS. Medial medullary infarction: clinical, imaging, and outcome study in 86 consecutive patients. Stroke. 2009. 40:3221–3225.9. Lee BI, Nam HS, Heo JH, Kim DI. Yonsei Stroke Team. Analysis of 1,000 patients with acute cerebral infarctions. Cerebrovasc Dis. 2001. 12:145–151.10. Kim YD, Choi HY, Jung YH, Nam CM, Yang JH, Cho HJ, et al. Classic risk factors for atherosclerosis are not major determinants for location of extracranial or intracranial cerebral atherosclerosis. Neuroepidemiology. 2009. 32:201–207.
Article11. Cho HJ, Choi HY, Kim YD, Nam HS, Han SW, Ha JW, et al. Transoesophageal echocardiography in patients with acute stroke with sinus rhythm and no cardiac disease history. J Neurol Neurosurg Psychiatry. 2010. 81:412–415.
Article12. North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991. 325:445–453.13. Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) Trial Investigators. Design, progress and challenges of a double-blind trial of warfarin versus aspirin for symptomatic intracranial arterial stenosis. Neuroepidemiology. 2003. 22:106–117.14. Kim JS, Lee JH, Suh DC, Lee MC. Spectrum of lateral medullary syndrome. Correlation between clinical findings and magnetic resonance imaging in 33 subjects. Stroke. 1994. 25:1405–1410.
Article15. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993. 24:35–41.
Article16. Yonas H, Agamanolis D, Takaoka Y, White RJ. Dissecting intracranial aneurysms. Surg Neurol. 1977. 8:407–415.17. Yamaura A, Watanabe Y, Saeki N. Dissecting aneurysms of the intracranial vertebral artery. J Neurosurg. 1990. 72:183–188.
Article18. Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003. 157:364–375.
Article19. Seçkin H, Ateş O, Bauer AM, Başkaya MK. Microsurgical anatomy of the posterior spinal artery via a far-lateral transcondylar approach. J Neurosurg Spine. 2009. 10:228–233.
Article20. Shono Y, Koga M, Toyoda K, Matsuoka H, Yokota C, Uehara T, et al. Medial medullary infarction identified by diffusion-weighted magnetic resonance imaging. Cerebrovasc Dis. 2010. 30:519–524.
Article21. Kolominsky-Rabas PL, Weber M, Gefeller O, Neundoerfer B, Heuschmann PU. Epidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke. 2001. 32:2735–2740.
Article22. Han SW, Kim SH, Lee JY, Chu CK, Yang JH, Shin HY, et al. A new subtype classification of ischemic stroke based on treatment and etiologic mechanism. Eur Neurol. 2007. 57:96–102.
Article23. Bejot Y, Caillier M, Ben Salem D, Couvreur G, Rouaud O, Osseby GV, et al. Ischaemic stroke subtypes and associated risk factors: a French population based study. J Neurol Neurosurg Psychiatry. 2008. 79:1344–1348.
Article24. Urban PP, Hopf HC, Connemann B, Hundemer HP, Koehler J. The course of cortico-hypoglossal projections in the human brainstem. Functional testing using transcranial magnetic stimulation. Brain. 1996. 119:1031–1038.
Article25. Kameda W, Kawanami T, Kurita K, Daimon M, Kayama T, Hosoya T, et al. Lateral and medial medullary infarction: a comparative analysis of 214 patients. Stroke. 2004. 35:694–699.26. Kumral E, Afsar N, Kirbas D, Balkir K, Ozdemirkiran T. Spectrum of medial medullary infarction: clinical and magnetic resonance imaging findings. J Neurol. 2002. 249:85–93.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Opalski Syndrome Presenting as Sensorimotor Deficits Ipsilateral to Cerebral Infarction
- Isolated Axial Lateropulsion in Lateral Medullary Infarction
- Lenticulostriate Artery Involvement is Predictive of Poor Outcomes in Superficial Middle Cerebral Artery Territory Infarction
- Medullary Infarction Presenting as Sudden Cardiac Arrest: Report of Two Cases and Review of the Literature
- High-Resolution Contrast-Enhanced 3D-Spoiled Gradient-Recalled Imaging for Evaluation of Intracranial Vertebral Artery and Posterior Inferior Cerebellar Artery in Lateral Medullary Infarction