Anat Cell Biol.
2015 Sep;48(3):218-221. 10.5115/acb.2015.48.3.218.
An anomalous portal vein crossing the lesser sac and ending at the upper part of ductus venosus
- Affiliations
-
- 1Department of Surgery and Biomedical Research Institute, Chonbuk National University Hospital, Jeonju, Korea.
- 2Department of Anatomy, Chonbuk National University Medical School, Jeonju, Korea. 407kk@hanmail.net
- 3Division of Internal Medicine, Iwamizawa Asuka Hospital, Iwamizawa, Japan.
- 4Institute of Embryology, Universidad Complutense, Madrid, Spain.
- KMID: 2424826
- DOI: http://doi.org/10.5115/acb.2015.48.3.218
Abstract
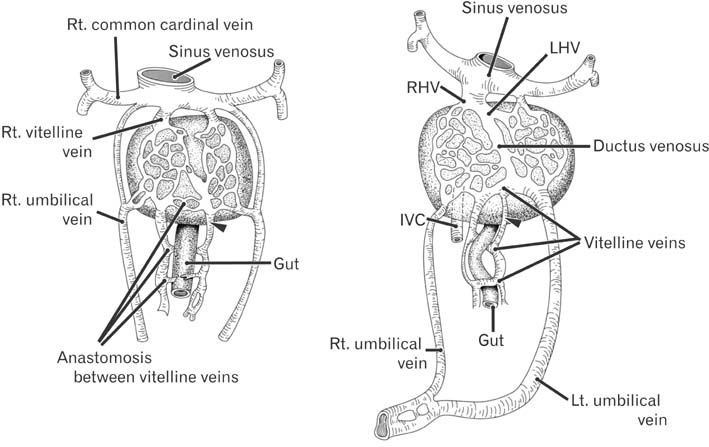
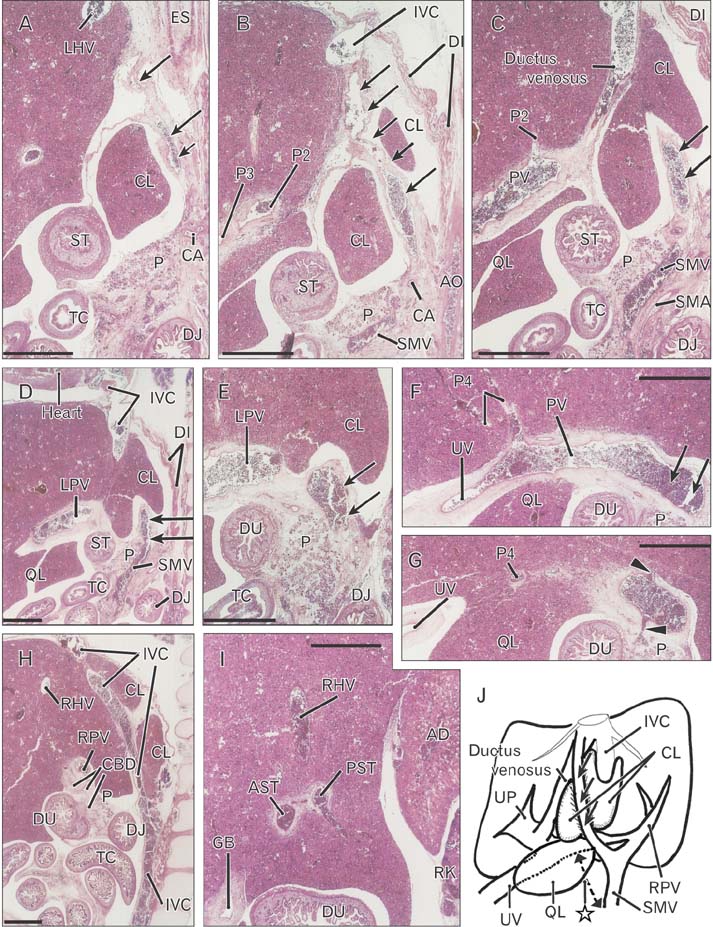
- In serial sagittal sections of a fetus on week 9 (crown-rump length, 36 mm), we incidentally found absence of the usual portal vein through the hepatoduodenal ligament. Instead, an anomalous portal vein originated behind the pancreatic body, crossed the lesser sac and merged with the upper part of the ductus venosus. During the course across the lesser sac, the vein provided a deep notch of the liver caudate lobe (Spiegel's lobe). The hepatoduodenal ligament contained the hepatic artery, the common bile duct and, at the right posterior margin of the ligament, and a branch of the anomalous portal vein which communicated with the usual right branch of the portal vein at the hepatic hilum. The umbilical portion of the portal vein took a usual morphology and received the umbilical vein and gave off the ductus venosus. Although it seemed not to be described yet, the present anomalous portal vein was likely to be a persistent left vitelline vein. The hepatoduodenal ligament was unlikely to include the left vitelline vein in contrast to the usual concept.
MeSH Terms
Figure
Reference
-
1. Collardeau-Frachon S, Scoazec JY. Vascular development and differentiation during human liver organogenesis. Anat Rec (Hoboken). 2008; 291:614–627.2. Inoue M, Taenaka N, Nishimura S, Kawamura T, Aki T, Yamaki K, Enomoto H, Kosaka K, Yoshikawa K. Prepancreatic postduodenal portal vein: report of a case. Surg Today. 2003; 33:956–959.3. Tomizawa N, Akai H, Akahane M, Ino K, Kiryu S, Ohtomo K. Prepancreatic postduodenal portal vein: a new hypothesis for the development of the portal venous system. Jpn J Radiol. 2010; 28:157–161.4. Jin ZW, Cho BH, Murakami G, Fujimiya M, Kimura W, Yu HC. Fetal development of the retrohepatic inferior vena cava and accessory hepatic veins: Re-evaluation of the Alexander Barry's hypothesis. Clin Anat. 2010; 23:297–303.5. Yi SQ, Tanaka S, Tanaka A, Shimokawa T, Ru F, Nakatani T. An extremely rare inversion of the preduodenal portal vein and common bile duct associated with multiple malformations. Report of an adult cadaver case with a brief review of the literature. Anat Embryol (Berl). 2004; 208:87–96.6. Dighe M, Vaidya S. Case report. Duplication of the portal vein: a rare congenital anomaly. Br J Radiol. 2009; 82:e32–e34.7. Hwang SE, Cho BH, Hirai I, Kim HT, Kim JH, Fujimiya M, Murakami G, Kimura W. Topographical anatomy of Spiegel's lobe and its adjacent organs in mid-term fetuses: its implication on the development of the lesser sac and adult morphology of the upper abdomen. Clin Anat. 2010; 23:712–719.8. Murakami G, Hata F. Human liver caudate lobe and liver segment. Anat Sci Int. 2002; 77:211–224.9. Kanamura T, Murakami G, Ko S, Hirai I, Hata F, Nakajima Y. Evaluating the hilar bifurcation territory in the human liver caudate lobe to obtain critical information for delimiting reliable margins during caudate lobe surgery: anatomic study of livers with and without the external caudate notch. World J Surg. 2003; 27:284–288.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fetal Intra-abdominal Umbilical Vein Varix Complicated with Patent Ductus Venosus and Atrial Septal Defect
- A Case of Non-Immune Hydrops Fetalis due to Umbilical Venous Malformation and Noonan Syndrome
- Multiple absences of the branches of abdominal aorta with congenital absence of the portal vein, unilateral adrenal agenesis and persistent ductus arteriosus in a female cadaver
- Blood flow volume difference (P-SS) between the portal vein and thesum of splenic vein and superior mesenteric vein in portal hypertension
- Computed Tomography Findings of Thrombosis and Aneurysm of the Portal Venous System