Cancer Res Treat.
2018 Oct;50(4):1270-1280. 10.4143/crt.2017.371.
Factors Associated with Prolonged Patient-Attributable Delay in the Diagnosis of Colorectal Cancer
- Affiliations
-
- 1Research Network on Health Services in Chronic Diseases (REDISSEC), Carlos III Health Institute, Madrid, Spain. mredondo@hcs.es
- 2Research Unit, Costa del Sol Hospital, University of Málaga, Marbella, Spain.
- 3Department of Oncohemathology, Costa del Sol Hospital, Marbella, Spain.
- 4Clinical Epidemiology and Cancer Screening, Corporació Sanitaria ParcTaulÃ, Sabadell, Spain.
- 5Department of Preventive Medicine and Public Health, University of Valencia, Valencia, Spain.
- 6Consortium for Biomedical Research in Epidemiology and Public Health (CIBERESP), Madrid, Spain.
- 7Epidemiology Unit, Sevilla District, Andalusian Regional Health Service, Sevilla, Spain.
- 8Research Unit, Donostia University Hospital, Biodonostia Health Research Institute, Donostia, Spain.
- 9Area of Environmental Epidemiology and Cancer, National Epidemiology Centre, Carlos III Health Institute, Madrid, Spain.
- 10Research Unit, Basurto University Hospital, Bilbao, Spain.
- 11Research Unit, Galdakao-Usansolo Hospital, Galdakao-Usansolo Hospital, Galdakao, Spain.
- KMID: 2424799
- DOI: http://doi.org/10.4143/crt.2017.371
Abstract
- PURPOSE
The delayed diagnosis of colorectal cancer (CRC) may be attributable to sociodemographic characteristics, to aspects of tumour histopathology or to the functioning of the health system. We seek to determine which of these factors most influences prolonged patient-attributable delay (PPAD) in the diagnosis and treatment of CRC.
MATERIALS AND METHODS
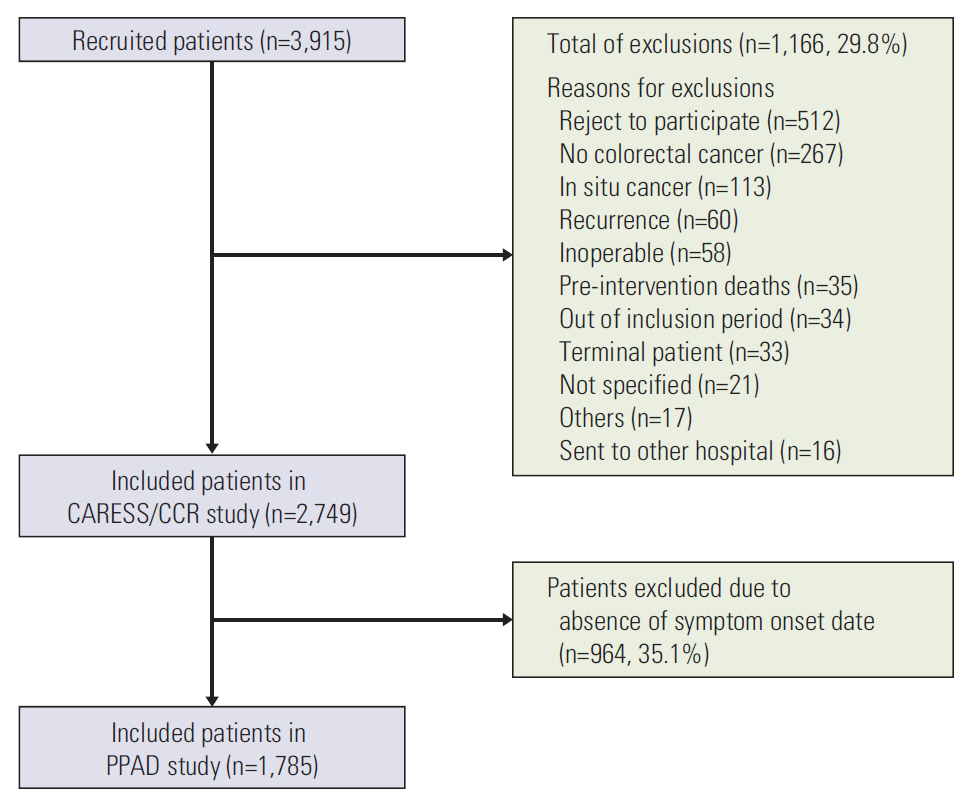
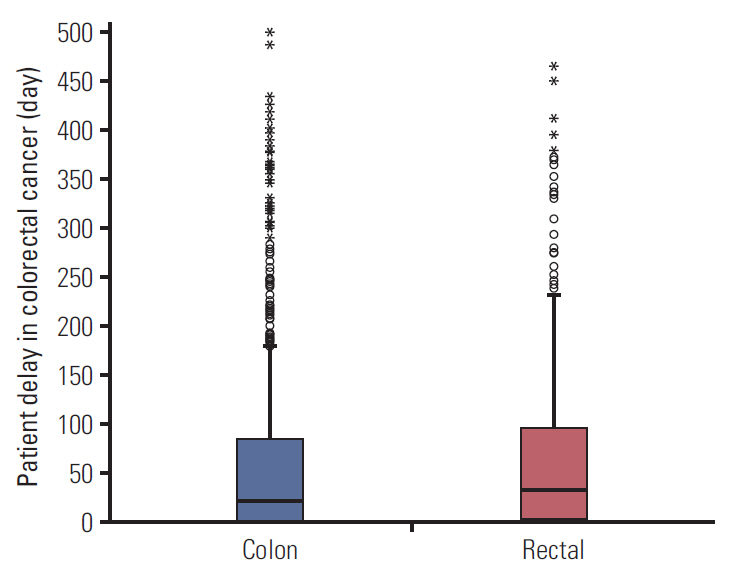
A prospective, multicentre observational study was conducted in 22 Spanish hospitals. In total, 1,785 patients were recruited to the study between 2010 and 2012 and underwent elective or urgent surgery. PPAD is considered to occur when the time elapsed between a patient presenting the symptom and him/her seeking attention from the primary care physician or hospital emergency department exceeds 180 days. A bivariate analysis was performed to assess differences in variables segmented by tumour location and patient delay. Multivariate logistic regression analysis was performed on the outcome variable, PPAD.
RESULTS
The rate of PPAD among this population was 12.1%. PPAD was significantly associated with altered bowel rhythm (odds ratio [OR], 1.36; 95% confidence interval [CI], 1.02 to 1.83) and with adenocarcinoma histology, in comparison with mucinous adenocarcinoma (OR, 2.03; 95% CI, 1.11 to 3.71). Other sociocultural factors and clinicopathological features were not independent predictors of PPAD.
CONCLUSION
Many patients do not consider altered bowel rhythm an alarming symptom, warranting a visit to the doctor. PPAD could be reduced by improving health education, raising awareness of CRC-related symptoms.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015; 65:87–108.
Article2. Edwards BK, Ward E, Kohler BA, Eheman C, Zauber AG, Anderson RN, et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010; 116:544–73.
Article3. Roncoroni L, Pietra N, Violi V, Sarli L, Choua O, Peracchia A. Delay in the diagnosis and outcome of colorectal cancer: a prospective study. Eur J Surg Oncol. 1999; 25:173–8.4. Khubchandani M. Relationship of symptom duration and survival in patients with carcinoma of the colon and rectum. Dis Colon Rectum. 1985; 28:585–7.
Article5. Pita-Fernandez S, Gonzalez-Saez L, Lopez-Calvino B, Seoane-Pillado T, Rodriguez-Camacho E, Pazos-Sierra A, et al. Effect of diagnostic delay on survival in patients with colorectal cancer: a retrospective cohort study. BMC Cancer. 2016; 16:664.
Article6. Ramos M, Esteva M, Cabeza E, Llobera J, Ruiz A. Lack of association between diagnostic and therapeutic delay and stage of colorectal cancer. Eur J Cancer. 2008; 44:510–21.
Article7. Andersen BL, Cacioppo JT. Delay in seeking a cancer diagnosis: delay stages and psychophysiological comparison processes. Br J Soc Psychol. 1995; 34(Pt 1):33–52.
Article8. Hansen RP, Vedsted P, Sokolowski I, Sondergaard J, Olesen F. Time intervals from first symptom to treatment of cancer: a cohort study of 2,212 newly diagnosed cancer patients. BMC Health Serv Res. 2011; 11:284.
Article9. Pedersen AF, Hansen RP, Vedsted P. Patient delay in colorectal cancer patients: associations with rectal bleeding and thoughts about cancer. PLoS One. 2013; 8:e69700.
Article10. Macleod U, Mitchell ED, Burgess C, Macdonald S, Ramirez AJ. Risk factors for delayed presentation and referral of symptomatic cancer: evidence for common cancers. Br J Cancer. 2009; 101 Suppl 2:S92–S101.
Article11. Quintana JM, Gonzalez N, Anton-Ladislao A, Redondo M, Bare M, Fernandez de Larrea N, et al. Colorectal cancer health services research study protocol: the CCR-CARESS observational prospective cohort project. BMC Cancer. 2016; 16:435.
Article12. Bernal Perez M, Gomez Bernal FJ, Gomez Bernal GJ. Delay in the diagnosis of cancer. Aten Primaria. 2001; 27:79–85.13. Esteva M, Leiva A, Ramos M, Pita-Fernandez S, Gonzalez-Lujan L, Casamitjana M, et al. Factors related with symptom duration until diagnosis and treatment of symptomatic colorectal cancer. BMC Cancer. 2013; 13:87.
Article14. Hallissey MT, Allum WH, Jewkes AJ, Ellis DJ, Fielding JW. Early detection of gastric cancer. BMJ. 1990; 301:513–5.
Article15. Irving MJ, Lamb PJ, Irving RJ, Raimes SA. Speeding up the diagnosis of oesophago-gastric cancer. Nurs Times. 2002; 98:35–7.16. Redondo M, Rodrigo I, Pereda T, Funez R, Acebal M, Perea-Milla E, et al. Prognostic implications of emergency admission and delays in patients with breast cancer. Support Care Cancer. 2009; 17:595–9.
Article17. Allgar VL, Neal RD. Delays in the diagnosis of six cancers: analysis of data from the National Survey of NHS Patients: Cancer. Br J Cancer. 2005; 92:1959–70.
Article18. Del Giudice ME, Vella ET, Hey A, Simunovic M, Harris W, Levitt C. Systematic review of clinical features of suspected colorectal cancer in primary care. Can Fam Physician. 2014; 60:e405–15.19. Zarcos-Pedrinaci I, Fernandez-Lopez A, Tellez T, Rivas-Ruiz F, Rueda A, Morales Suarez-Varela MM, et al. Factors that influence treatment delay in patients with colorectal cancer. Oncotarget. 2017; 8:36728–42.
Article20. Macdonald S, Macleod U, Campbell NC, Weller D, Mitchell E. Systematic review of factors influencing patient and practitioner delay in diagnosis of upper gastrointestinal cancer. Br J Cancer. 2006; 94:1272–80.
Article21. Gullo L, Tomassetti P, Migliori M, Casadei R, Marrano D. Do early symptoms of pancreatic cancer exist that can allow an earlier diagnosis? Pancreas. 2001; 22:210–3.
Article22. Hackett TP, Cassem NH, Raker JW. Patient delay in cancer. N Engl J Med. 1973; 289:14–20.
Article23. Van Hout AM, de Wit NJ, Rutten FH, Peeters PH. Determinants of patient's and doctor's delay in diagnosis and treatment of colorectal cancer. Eur J Gastroenterol Hepatol. 2011; 23:1056–63.
Article24. Thornton L, Reader H, Stojkovic S, Allgar V, Woodcock N. Has the 'Fast-Track' referral system affected the route of presentation and/or clinical outcomes in patients with colorectal cancer? World J Surg Oncol. 2016; 14:158.
Article25. Brown S, Castelli M, Hunter DJ, Erskine J, Vedsted P, Foot C, et al. How might healthcare systems influence speed of cancer diagnosis: a narrative review. Soc Sci Med. 2014; 116:56–63.
Article26. Kim SH, Shin SJ, Lee KY, Kim H, Kim TI, Kang DR, et al. Prognostic value of mucinous histology depends on microsatellite instability status in patients with stage III colon cancer treated with adjuvant FOLFOX chemotherapy: a retrospective cohort study. Ann Surg Oncol. 2013; 20:3407–13.
Article27. Park JS, Huh JW, Park YA, Cho YB, Yun SH, Kim HC, et al. Prognostic comparison between mucinous and nonmucinous adenocarcinoma in colorectal cancer. Medicine (Baltimore). 2015; 94:e658.
Article28. Shin US, Yu CS, Kim JH, Kim TW, Lim SB, Yoon SN, et al. Mucinous rectal cancer: effectiveness of preoperative chemoradiotherapy and prognosis. Ann Surg Oncol. 2011; 18:2232–9.
Article29. Glimelius B, Tiret E, Cervantes A, Arnold D; ESMO Guidelines Working Group. Rectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013; 24 Suppl 6:vi81–8.
Article30. Langenbach MR, Schmidt J, Neumann J, Zirngibl H. Delay in treatment of colorectal cancer: multifactorial problem. World J Surg. 2003; 27:304–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Population Attributable Fraction of Established Modifiable Risk Factors on Colorectal Cancer in Korea
- Improving survival after endometrial cancer: the big picture
- Endoscopic diagnosis and treatment of early colorectal cancer
- A case of Colorectal carcinoma During Pregnancy
- Screening strategy for colorectal cancer according to risk