J Korean Acad Nurs.
2016 Aug;46(4):514-522. 10.4040/jkan.2016.46.4.514.
Comparison of Effects of Exhalation and Inhalation Breathing Exercises on Pulmonary Function and Complications in Elderly Patients with Upper-abdominal Surgery
- Affiliations
-
- 1SICU, Pusan National University Yangsan Hospital, Yangsan, Korea. worldofmiji@hanmail.net
- 2College of Nursing, Pusan National University, Yangsan, Korea.
- KMID: 2424548
- DOI: http://doi.org/10.4040/jkan.2016.46.4.514
Abstract
- PURPOSE
The purpose of this study was to identify the effects of exhalation breathing exercises using expirometer and that of inhalation breathing exercises using incentive spirometry on pulmonary function and complications in elderly patients with upper-abdominal surgery.
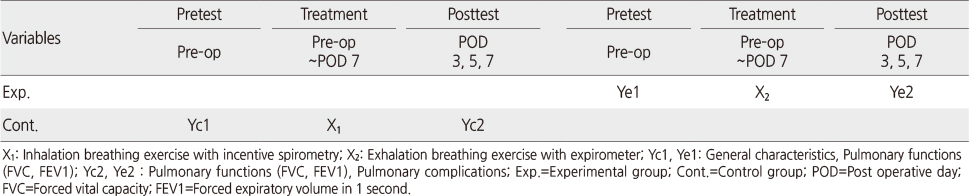
METHODS
The research design was a nonequivalent control group non-synchronized design. Participants were 63 patients who underwent upper-abdominal surgery under general anesthesia (32 in experiment group, 31 in control group). They were recruited at P university hospital from August 1 to November 30, 2015. Effects were evaluated by measuring pulmonary functions (Forced Vital Capacity [FVC], Forced Expiratory Volume in 1 second [FEV1]) and pulmonary complications. Data were analyzed using SPSS/WIN 18.0 program.
RESULTS
There was no difference in FVC between the experimental group and the control group, but FEV1 in the experimental group increased significantly compared to the control group by time change (p=.001). Also, there were no pulmonary complications in the experimental group but there were 5 cases (16.1%)(p=.018) in the control group.
CONCLUSION
Findings indicate that exhalation breathing exercises by elderly patients following upper-abdominal surgery is an effective nursing intervention in enhancing pulmonary function and preventing pulmonary complications.
Keyword
MeSH Terms
Figure
Reference
-
1. García-Miguel FJ, Serrano-Aguilar PG, López-Bastida J. Preoperative assessment. Lancet. 2003; 362(9397):1749–1757.2. Kim WS, Kim BG, Kim JY. Study on the normal predictive values of pulmonary function and related factors in Korean adults using portable spirometer. Res Works Grad Sch. 2002; 27:405–417.3. Ryu KH. Critical point of anesthetic management in the elderly. Korean J Anesthesiol. 2004; 46(5):501–516. DOI: 10.4097/kjae.2004.46.5.501.4. Ryu YJ, Park JY, Baik SJ, Lee JH, Cheon EM, Chang JH. Incidence and predictors of postoperative pulmonary complications after nonthoracic surgery in patients of 65 years old or more. Korean J Med. 2004; 67(1):65–72.5. Hedenstierna G. Alveolar collapse and closure of airways: Regular effects of anaesthesia. Clin Physiol Funct Imaging. 2003; 23(3):123–129.6. Rock P. Preoperative evaluation of the patient with pulmonary disease. In : 6th Critical Care Refresher Course at the 31st Annual Meeting of the Society of Critical Care Medicine; 2002 January 25-26; San Diego, CA.7. Doh YJ, Hur IK, Lee JY, Park JB, Sung NI, Lee YG, et al. Reappraisal of the predictive factors for postoperative pulmonary complications after general anesthesia. Korean J Med. 2007; 72(5):501–510.8. Lee BY, Shon KH. The effect of chest meridian massage on postanesthetic recovery of general anesthesia patients. J Korean Acad Adult Nurs. 2005; 17(4):612–621.9. Kim HT, Lee SM, Uh ST, Chung YT, Kim YH, Park CS. Recovery of pulmonary function according to the operative sites after general anesthesia. Tuberc Respir Dis. 1993; 40(3):250–258.10. Arozullah AM, Conde MV, Lawrence VA. Preoperative evaluation for postoperative pulmonary complications. Med Clin North Am. 2003; 87(1):153–173.11. Reimer-Kent J. Creating a postoperative wellness model to optimize and enhance rapid surgical recovery. Can J Cardiovasc Nurs. 2012; 22(2):7–23.12. Canet J, Gallart L. Postoperative respiratory failure: Pathogenesis, prediction, and prevention. Curr Opin Crit Care. 2014; 20(1):56–62. DOI: 10.1097/mcc.0000000000000045.13. Kim YH, Park SN, Hwang KH. Pulmonology. Seoul: Korea Medical Book Publisher;2011. p. 1–206.14. Brown R, DiMarco AF, Hoit JD, Garshick E. Respiratory dysfunction and management in spinal cord injury. Respir Care. 2006; 51(8):853–868.15. Kang SW, Shin JC, Park CI, Moon JH, Rha DW, Cho DH. Relationship between inspiratory muscle strength and cough capacity in cervical spinal cord injured patients. Spinal Cord. 2006; 44(4):242–248. DOI: 10.1038/sj.sc.3101835.16. Sutbeyaz ST, Koseoglu F, Inan L, Coskun O. Respiratory muscle training improves cardiopulmonary function and exercise tolerance in subjects with subacute stroke: A randomized controlled trial. Clin Rehabil. 2010; 24(3):240–250. DOI: 10.1177/0269215509358932.17. Min YM. The effect of regular practice for deep breathing on function of postoperative pulmonary ventilation in geriatric patients [master's thesis]. Suwon: Ajou University;2007. 1–42.18. Kim KN. The effect of regular practice for deep breathing on postoperative pulmonary ventilation of the aged who underwent lobectomy[master's thesis]. Busan: Catholic University of Pusan;2009. 1–44.19. Lunardi AC, Paisani DM, Marques da Silva CC, Cano DP, Tanaka C, Carvalho CR. Comparison of lung expansion techniques on thoracoabdominal mechanics and incidence of pulmonary complications after upper abdominal surgery: A randomized and controlled trial. Chest. 2015; 148(4):1003–1010. DOI: 10.1378/chest.14-2696.20. do Nascimento Junior P, Módolo NS, Andrade S, Guimarães MM, Braz LG, El Dib R. Incentive spirometry for prevention of postoperative pulmonary complications in upper abdominal surgery. Cochrane Database Syst Rev. 2014; (2):CD006058. DOI: 10.1002/14651858.CD006058.pub3.21. Jeon YJ, Oh DW, Kim KM, Lee YJ. Comparison of the effect of inhalation and exhalation breathing exercises on pulmonary function of patients with cervical cord injury. Phys Ther Korea. 2010; 17(1):9–16.22. Kwun KB. Perioperative pulmonary management. Korean J Crit Care Med. 2003; 18(1):7–19.23. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: L. Erlbaum Associates;1988.24. Mazo V, Sabaté S, Canet J, Gallart L, de Abreu MG, Belda J, et al. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology. 2014; 121(2):219–231. DOI: 10.1097/aln.0000000000000334.25. Lee HR, Choe CJ, Park OJ, Kim YS, Choi KO, Kim KS, et al. Adult nursing I. 6th ed. Paju: Soomoonsa;2007.26. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005; 26(2):319–338. DOI: 10.1183/09031936.05.00034805.27. Seo YH, Kang HS. The effects of the respiration strengthening exercise program on pulmonary function, anxiety, and sleep of patients underwent lung surgery. Clin Nurs Res. 2007; 13(3):157–167.28. Nunn AJ, Gregg I. New regression equations for predicting peak expiratory flow in adults. BMJ. 1989; 298(6680):1068–1070.29. Lee W, Yang YL, Oh EG. Effectiveness of deep breathing exercise for postoperative pulmonary complications prevention: A systematic review. J Korean Acad Fundam Nurs. 2014; 21(4):423–432. DOI: 10.7739/jkafn.2014.21.4.423.30. The Korean Academy of Tuberculosis and Respiratory Diseases. Respiratory diseases. Paju: Koonja;2004.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Deep Breathing Exercise and Incentive Spirometry to Prevent Postoperative Pulmonary Complications after Abdominal Surgery in Geriatric Patients
- Effect of Breathing Exercise Using Panflutes on the Postoperative Compliance, Pulmonary Infections and Life Satisfaction in Elderly Patients Undergoing Spinal Surgery
- The Study on the Effects of a Respiratory Rehabilitation Program for COPD Patients
- The Effects of Deep Breathing Methods on Pulmonary Ventilatory Function of Pneumothorax Patients undergoing a Thoracotomy
- The Effects of Abdominal Relaxed Breathing Exercises using Biofeedback on Stress Response and Blood Pressure in Elderly People with Hypertension