Korean J Neurotrauma.
2018 Oct;14(2):169-172. 10.13004/kjnt.2018.14.2.169.
Rapid Healing and Remodeling Process of Pediatric Seat-Belt Fracture without Surgical Treatment
- Affiliations
-
- 1Department of Neurosurgery, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea. nscharisma@hanmail.net
- KMID: 2424334
- DOI: http://doi.org/10.13004/kjnt.2018.14.2.169
Abstract
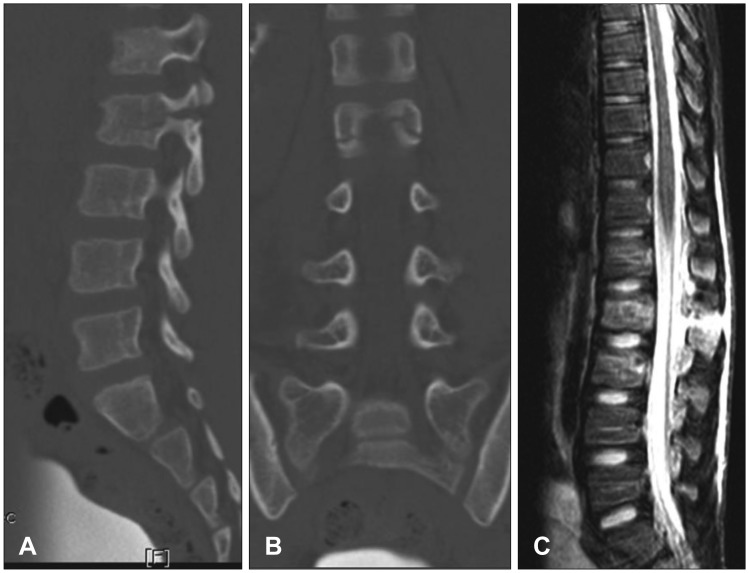
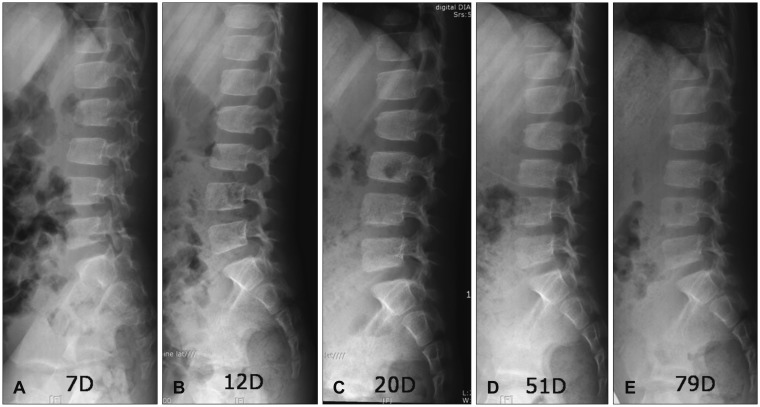
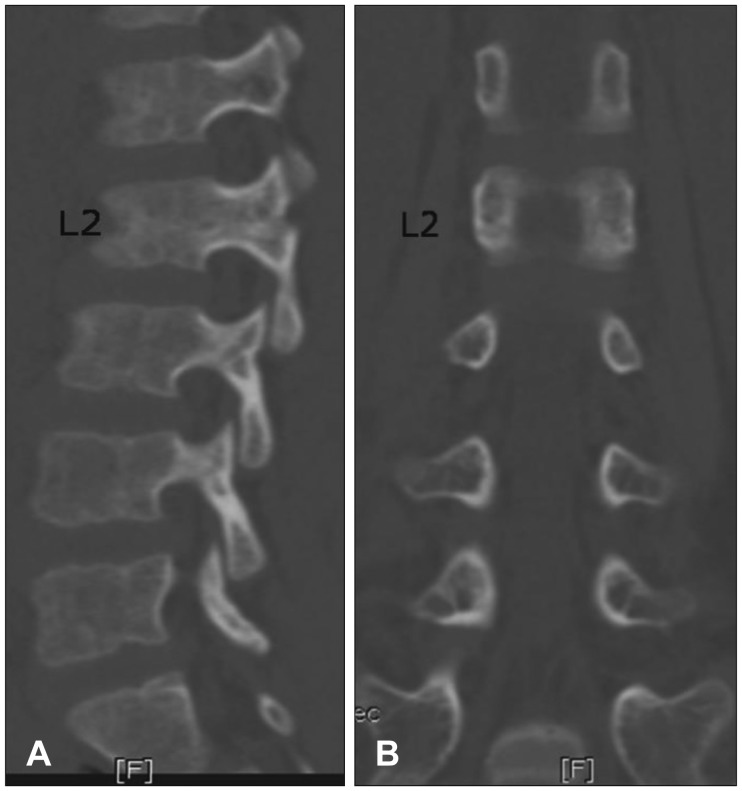
- Pediatric seat-belt fracture is a rare condition, and its management has not been well defined. The authors report a case of pediatric Chance fracture that was managed conservatively and that demonstrated rapid bone healing. A 7-year-old boy presented with back pain after a motor vehicle accident. Plain lumbar spine radiography, three-dimensional computed tomography (CT), and magnetic resonance imaging revealed a seat-belt fracture type C (classified by Rumball and Jarvis), and the patient's condition was managed conservatively. The patient started to ambulate with a brace 2 weeks after the injury. Spine CT performed 100 days after the injury revealed a remodeled fracture, and dynamic radiography did not show any evidence of instability or kyphotic deformity. We suggest that if there are no neurological deficits or severe deformities, then a pediatric seat-belt fracture should be managed conservatively, because the bone healing process is far more rapid in children than it is in adults and because of possible growth problems after surgery.
MeSH Terms
Figure
Reference
-
1. Abdelgawad AA, Kanlic EM. Orthopedic management of children with multiple injuries. J Trauma. 2011; 70:1568–1574. PMID: 21817996.
Article2. Andras LM, Skaggs KF, Badkoobehi H, Choi PD, Skaggs DL. Chance fractures in the pediatric population are often misdiagnosed. J Pediatr Orthop. 2016; epub ahead of print. DOI: 10.1097/bpo.0000000000000925.
Article3. Dawkins RL, Miller JH, Ramadan OI, Lysek MC, Kuhn EN, Rocque BG, et al. a reliability study. J Neurosurg Pediatr. 2018; 21:284–291. PMID: 29328004.4. Le TV, Baaj AA, Deukmedjian A, Uribe JS, Vale FL. Chance fractures in the pediatric population. J Neurosurg Pediatr. 2011; 8:189–197. PMID: 21806362.
Article5. Mikles MR, Stchur RP, Graziano GP. Posterior instrumentation for thoracolumbar fractures. J Am Acad Orthop Surg. 2004; 12:424–435. PMID: 15615508.
Article6. Mulpuri K, Jawadi A, Perdios A, Choit RL, Tredwell SJ, Reilly CW. Outcome analysis of chance fractures of the skeletally immature spine. Spine (Phila Pa 1976). 2007; 32:E702–E707. PMID: 18007230.
Article7. Rumball K, Jarvis J. Seat-belt injuries of the spine in young children. J Bone Joint Surg Br. 1992; 74:571–574. PMID: 1624518.
Article8. Santschi M, Lemoine C, Cyr C. The spectrum of seat belt syndrome among Canadian children: Results of a two-year population surveillance study. Paediatr Child Health. 2008; 13:279–283. PMID: 19337593.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Appendiceal transection associated with seat belt restraint
- Delayed presentation of an entrapped small bowel loop stricture in a case of seat belt injury with the seat belt sign: laparoscopic resection and anastomosis
- Seat belt injury
- Bipolar Clavicular Dislocation: A Case Report
- Neck fracture case at low speed in frontal collision