Korean J Gastroenterol.
2018 Oct;72(4):188-196. 10.4166/kjg.2018.72.4.188.
Risk Factors and On-site Rescue Treatments for Endoscopic Variceal Ligation Failure
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea. estevanj@naver.com
- KMID: 2424110
- DOI: http://doi.org/10.4166/kjg.2018.72.4.188
Abstract
- BACKGROUND/AIMS
The success rate of endoscopic variceal ligation (EVL) is about 85-94%. There is only a few studies attempting to determine the cause of EVL failure, and to date, on-site rescue treatments remains unestablished. This study aimed to elucidate the risk factors for EVL failure and the effectiveness of on-site rescue treatment.
METHODS
Data of 454 patients who underwent emergency EVL at Chonnam National University Hospital were retrospectively analyzed. Enrolled patients were divided into two groups: the EVL success and EVL failure groups. EVL failures were defined as inability to ligate the varices due to poor endoscopic visual field, or failure of hemostasis after band ligation for the culprit lesion.
RESULTS
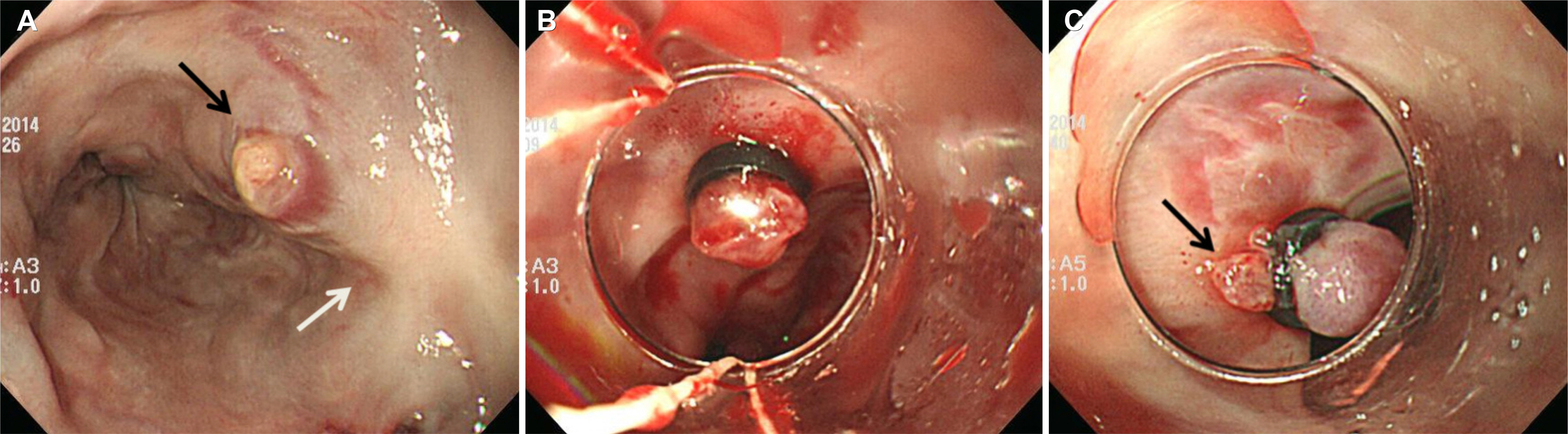
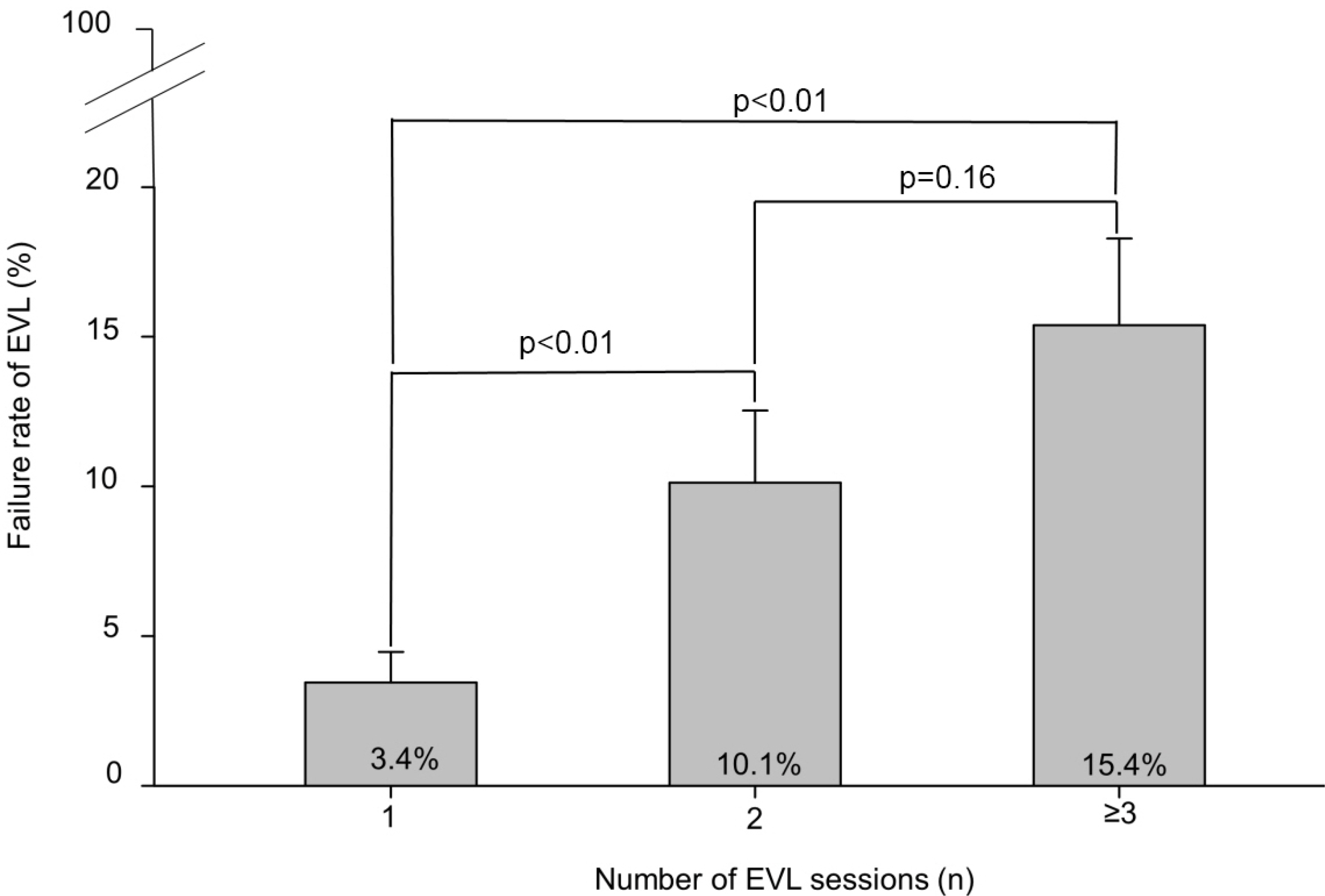
Forty-seven patients experienced EVL failure. In the multivariate analysis, male patients, initial hypovolemic shock, active bleeding on endoscopy, and history of previous EVL were independent risk factors for EVL failure. During endoscopic procedure, we came across the common causes of EVL failure, including unsuctioned varix due to previous EVL-induced scars followed by insufficient ligation of the stigmata and inability to ligate the varix due to poor endoscopic visual field. Endoscopic variceal obturation using N-butyl-2-cyanoacrylate (48.9%) was the most commonly used on-site rescue treatment method, followed by insertion of Sangstaken Blakemore tube (14.9%), and EVL retrial (12.8%). The rescue treatments successfully achieved hemostasis in 91.7% of those in the EVL failure group.
CONCLUSIONS
The risk factors of EVL failure should be considered before performing EVL, and in case of such scenario, on-site rescue treatment is needed.
MeSH Terms
Figure
Reference
-
References
1. Sanyal AJ, Fontana RJ, Di Bisceglie AM, et al. The prevalence and risk factors associated with esophageal varices in subjects with hepatitis C and advanced fibrosis. Gastrointest Endosc. 2006; 64:855–864.
Article2. Garcia‐ Tsao G, Sanyal AJ, Grace ND, Carey W. Practice Guidelines Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007; 46:922–938.
Article3. Bosch J, García-Pagán JC. Prevention of variceal rebleeding. Lancet. 2003; 361:952–954.
Article4. Saad WE, Darcy MD. Transjugular intrahepatic portosystemic shunt (TIPS) versus balloon-occluded retrograde transvenous obliteration (BRTO) for the management of gastric varices. Semin Intervent Radiol. 2011; 28:339–349.
Article5. Iwatsuki S, Starzl TE, Todo S, et al. Liver transplantation in the treatment of bleeding esophageal varices. Surgery. 1988; 104:697–705.6. Maluf-Filho F, Sakai P, Ishioka S, Matuguma SE. Endoscopic sclerosis versus cyanoacrylate endoscopic injection for the first episode of variceal bleeding: a prospective, controlled, and randomized study in Child-Pugh class C patients. Endoscopy. 2001; 33:421–427.
Article7. Sung JJ, Yeo W, Suen R, et al. Injection sclerotherapy for variceal bleeding in patients with hepatocellular carcinoma: cyanoacrylate versus sodium tetradecyl sulphate. Gastrointest Endosc. 1998; 47:235–239.
Article8. de Franchis R, Baveno Faculty VI. Expanding consensus in portal hypertension: report of the Baveno VI consensus workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015; 63:743–752.9. Stiegmann GV, Goff JS, Michaletz-Onody PA, et al. Endoscopic sclerotherapy as compared with endoscopic ligation for bleeding esophageal varices. N Engl J Med. 1992; 326:1527–1532.
Article10. Garcia-Pagán JC, Bosch J. Endoscopic band ligation in the treatment of portal hypertension. Nat Clin Pract Gastroenterol Hepatol. 2005; 2:526–535.
Article11. Laine L, Cook D. Endoscopic ligation compared with sclerotherapy for treatment of esophageal variceal bleeding. A metaanalysis. Ann Intern Med. 1995; 123:280–287.12. Gimson AE, Ramage JK, Panos MZ, et al. Randomised trial of variceal banding ligation versus injection sclerotherapy for bleeding oesophageal varices. Lancet. 1993; 342:391–394.
Article13. Lo GH, Lai KH, Cheng JS, et al. A prospective, randomized trial of sclerotherapy versus ligation in the management of bleeding esophageal varices. Hepatology. 1995; 22:466–471.
Article14. Kim HY, Park JK, Shim JH, et al. Clinical course of esophageal varices treated with endoscopic variceal ligation. Korean J Med. 2005; 68:498–503.15. Chen WC, Lo GH, Tsai WL, Hsu PI, Lin CK, Lai KH. Emergency endoscopic variceal ligation versus somatostatin for acute esophageal variceal bleeding. J Chin Med Assoc. 2006; 69:60–67.
Article16. Idezuki Y. General rules for recording endoscopic findings of esophagogastric varices (1991). Japanese Society for Portal Hypertension. World J Surg. 1995; 19:420–422. discussion 423.17. de Franchis R, Primignani M. Natural history of portal hypertension in patients with cirrhosis. Clin Liver Dis. 2001; 5:645–663.
Article18. Habib A, Sanyal AJ. Acute variceal hemorrhage. Gastrointest Endosc Clin N Am. 2007; 17:223–252. v.
Article19. Saeed ZA, Michaletz PA, Winchester CB, et al. Endoscopic variceal ligation in patients who have failed endoscopic sclerotherapy. Gastrointest Endosc. 1990; 36:572–574.
Article20. Cipolletta L, Zambelli A, Bianco MA, et al. Acrylate glue injection for acutely bleeding oesophageal varices: a prospective cohort study. Dig Liver Dis. 2009; 41:729–734.
Article21. Avgerinos A, Armonis A. Balloon tamponade technique and efficacy in variceal haemorrhage. Scand J Gastroenterol Suppl. 1994; 207:11–16.
Article22. Escorsell À, Pavel O, Cárdenas A, et al. Esophageal balloon tamponade versus esophageal stent in controlling acute refractory variceal bleeding: a multicenter randomized, controlled trial. Hepatology. 2016; 63:1957–1967.
Article23. Vangeli M, Patch D, Burroughs AK. Salvage tips for uncontrolled variceal bleeding. J Hepatol. 2002; 37:703–704.
Article24. Holster IL, Tjwa ET, Moelker A, et al. Covered transjugular intrahepatic portosystemic shunt versus endoscopic therapy + β-blocker for prevention of variceal rebleeding. Hepatology. 2016; 63:581–589.25. Qi X, He C, Guo W, et al. Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with variceal bleeding in liver cirrhosis: outcomes and predictors in a prospective cohort study. Liver Int. 2016; 36:667–676.
Article26. D'Amico G, De Franchis R. Cooperative Study Group. Upper digestive bleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators. Hepatology. 2003; 38:599–612.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Endoscopic Variceal Ligation versus Combined Ligation and Sclerotherapy for Bleeding Esophageal Varices
- The Use of Vasoconstrictors in Acute Variceal Bleeding: How Long Is Enough?
- Endoscopic Therapy and Radiologic Intervention of Acute Gastroesophageal Variceal Bleeding
- Endoscopic Treatment and Prevention of Acute Variceal Hemorrhage
- A Case of Esophageal Perforation during Endoscopic Variceal Ligation