Neurointervention.
2018 Sep;13(2):129-132. 10.5469/neuroint.2018.01032.
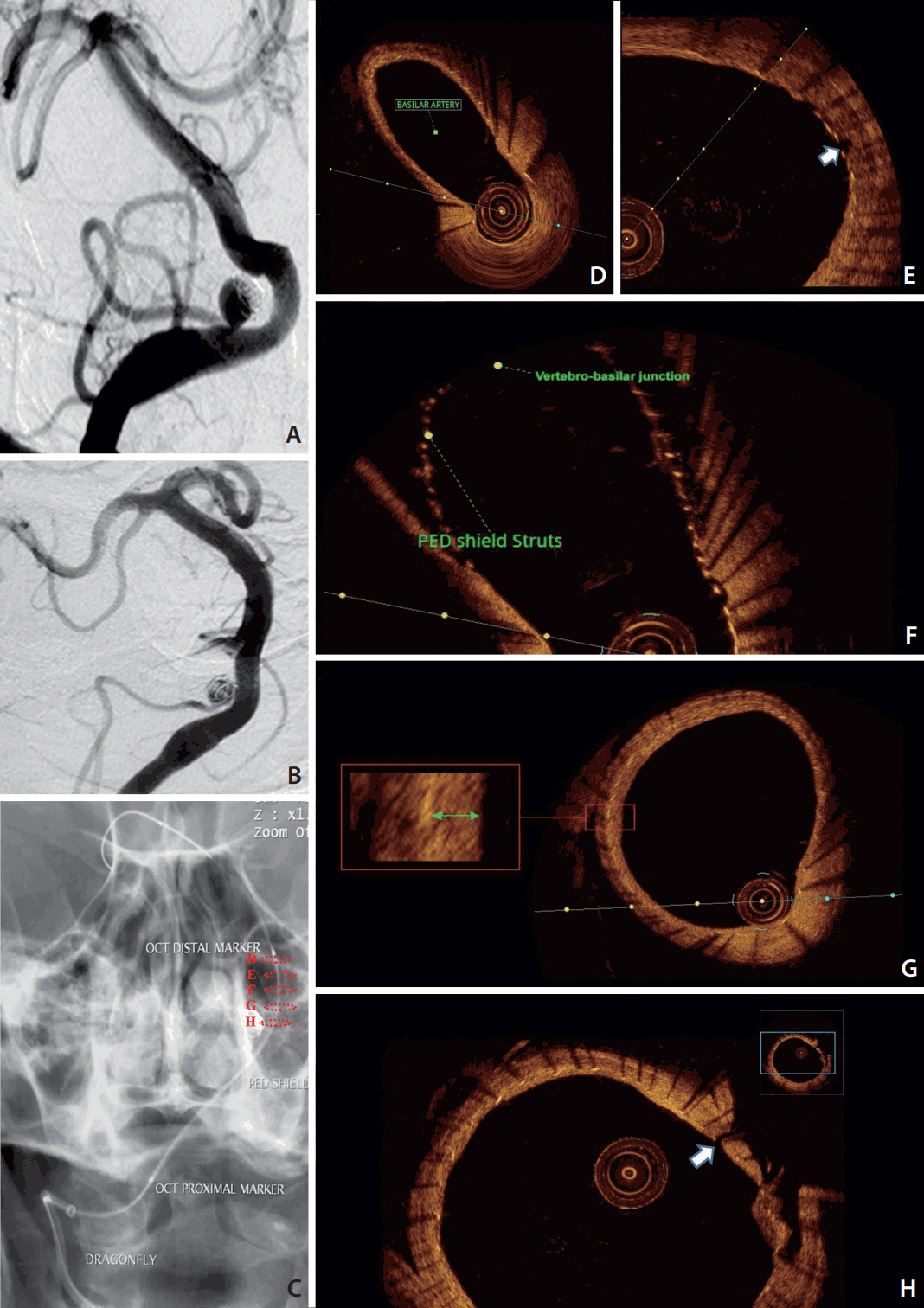
First Human Evaluation of Endothelial Healing after a Pipeline Flex Embolization Device with Shield Technology Implanted in Posterior Circulation Using Optical Coherence Tomography
- Affiliations
-
- 1Angioteam, Angiosur, MedellÃn, Colombia.
- 2Department of Radiology, Universidad de Antioquia, MedellÃn, Colombia.
- 3Department of Neurological Surgery, Rush University Medical Center, Chicago, IL, USA. Demetrius_Lopes@Rush.edu
- 4Department of Neurology, Mansoura University, Mansoura, Egypt.
- 5Interventional Neuroradiology Unit, Hospital Universitario Fundación Jiménez DÃaz, Madrid, Spain.
- KMID: 2424063
- DOI: http://doi.org/10.5469/neuroint.2018.01032
Abstract
- A 64-year-old female presented with an incidentally-discovered right posterior inferior cerebral artery (PICA) aneurysm, initially treated in 2015 by simple coiling. Follow-up demonstrated significant coil compaction that required retreatment. Retreatment was done uneventfully using a Pipeline embolization device (PED) shield deployed starting from the basilar artery and ending at the V4 segment of the vertebral artery. Eight-weeks post-deployment, a follow-up digital subtraction imaging (DSA) and intravascular imaging with optical coherence tomography were obtained. The intravascular imaging demonstrated that the flow diverter had good wall apposition and concentric neointimal growth over the braid with exception to the areas that the PED was not in contact with the endothelial wall, such as at the right PICA ostium and at the vertebrobasilar junction. The entire procedure was safe, and the patient had no complications. In this article, we describe for the first time the assessment of the status of endothelial "healing" of the PED shield at 8-weeks.
MeSH Terms
Figure
Reference
-
1. Brinjikji W, Lanzino G, Cloft HJ, Siddiqui AH, Boccardi E, Cekirge S, et al. Risk factors for ischemic complications following pipeline embolization device treatment of intracranial aneurysms: results from the IntrePED study. AJNR Am J Neuroradiol. 2016; 37:1673–1678.
Article2. Martínez-Galdámez M, Lamin SM, Lagios KG, Liebig T, Ciceri EF, Chapot R, et al. Periprocedural outcomes and early safety with the use of the Pipeline Flex Embolization Device with Shield Technology for unruptured intracranial aneurysms: preliminary results from a prospective clinical study. J Neurointerv Surg. 2017; 9:772–776.
Article3. Tearney G, Regar E, Akasaka T, Adriaenssens T, Barlis P, Bezerra HG, et al. Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation. J Am Coll Cardiol. 2012; 59:1058–1072.4. Girdhar G, Li J, Kostousov L, Wainwright J, Chandler WL. In-vitro thrombogenicity assessment of flow diversion and aneurysm bridging devices. J Thromb Thrombolysis. 2015; 40:437–443.
Article5. Hagen MW, Girdhar G, Wainwright J, Hinds MT. Thrombogenicity of flow diverters in an ex vivo shunt model: effect of phosphorylcholine surface modification. J Neurointerv Surg. 2016; 9:1006–1011.
Article6. Lopes DK, Johnson AK. Evaluation of cerebral artery perforators and the pipeline embolization device using optical coherence tomography. J Neurointerv Surg. 2012; 4:291–294.
Article7. Marosfoi M, Clarencon F, Langan ET, King RM, Brooks OW, Tamura T, et al. Acute thrombus formation on phosphorilcholine surface modified flow diverters. J Neurointerv Surg. 2018; 10:406–411.
Article8. Matsuda Y, Chung J, Lopes DK. Analysis of neointima development in flow diverters using optical coherence tomography imaging. J Neurointerv Surg. 2018; 10:162–167.
Article9. Given CA 2nd, Ramsey CN 3rd, Attizzani GF, Jones MR, Brooks WH, Bezerra HG, et al. Optical coherence tomography of the intracranial vasculature and Wingspan stent in a patient. BMJ Case Rep. 2014; 2014:bcr2014011114.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Microsurgical Strategies Following Failed Endovascular Treatment with the Pipeline Embolization Device: Case of a Giant Posterior Cerebral Artery Aneurysm
- Evaluation of the Cortical Vitreous Using Swept-Source Optical Coherence Tomography in Normal Eyes
- A Case of Ruptured Blood Blister-like Aneurysm Treated with Pipeline Embolization Device: Clinical Significance of Fetal-type Posterior Communicating Artery
- Photoacoustic imaging platforms for multimodal imaging
- Availability of Optical Coherence Tomography in Diagnosis and Classification of Choroidal Neovascularization