Brain Tumor Res Treat.
2018 Oct;6(2):78-81. 10.14791/btrt.2018.6.e11.
Gliosarcoma of Cerebello-Pontine Angle: A Case Report and Review of the Literature
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Cheonan Hospital, Cheonan, Korea. schnsohj@gmail.com
- KMID: 2423978
- DOI: http://doi.org/10.14791/btrt.2018.6.e11
Abstract
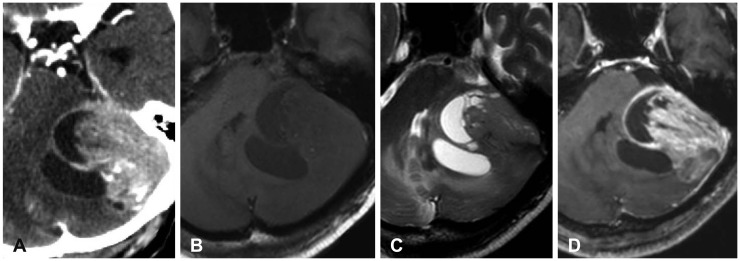
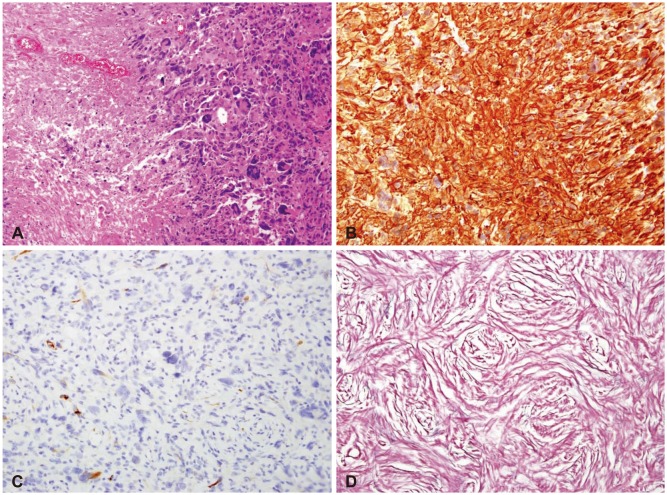
- Gliosarcoma (GS), known as variant of glioblastoma multiforme, is aggressive and very rare primary central nervous system malignant neoplasm. They are usually located in the supratentorial area with possible direct dural invasion or only reactive dural thickening. However, in this case, GS was located in lateral side of left posterior cranial fossa. A 78-year-old man was admitted to our hospital with 3 month history of continuous dizziness and gait disturbance without past medical history. A gadolinium-enhanced MRI demonstrated 5.6×4.8×3.2 cm sized mass lesion in left posterior cranial fossa, heterogeneously enhanced. The patient underwent left retrosigmoid craniotomy with navigation system. The tumor was combined with 2 components, whitish firm mass and gray colored soft & suckable mass. On pathologic report, the final diagnosis was GS of WHO grade IV. In spite of successful gross total resection of tumor, we were no longer able to treat because of the patient's rejection of adjuvant treatment. The patient survived for nine months without receiving any special treatment from the hospital.
Keyword
MeSH Terms
Figure
Reference
-
1. Kozak KR, Mahadevan A, Moody JS. Adult gliosarcoma: epidemiology, natural history, and factors associated with outcome. Neuro Oncol. 2009; 11:183–191. PMID: 18780813.
Article2. Galanis E, Buckner JC, Dinapoli RP, et al. Clinical outcome of gliosarcoma compared with glioblastoma multiforme: North Central Cancer Treatment Group results. J Neurosurg. 1998; 89:425–430. PMID: 9724117.
Article3. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016; 131:803–820. PMID: 27157931.
Article4. Zhang G, Huang S, Zhang J, Wu Z, Lin S, Wang Y. Clinical outcome of gliosarcoma compared with glioblastoma multiforme: a clinical study in Chinese patients. J Neurooncol. 2016; 127:355–362. PMID: 26725096.
Article5. Han SJ, Yang I, Tihan T, Prados MD, Parsa AT. Primary gliosarcoma: key clinical and pathologic distinctions from glioblastoma with implications as a unique oncologic entity. J Neurooncol. 2010; 96:313–320. PMID: 19618114.
Article6. Boerman RH, Anderl K, Herath J, et al. The glial and mesenchymal elements of gliosarcomas share similar genetic alterations. J Neuropathol Exp Neurol. 1996; 55:973–981. PMID: 8800093.
Article7. Reis RM, Könü-Lebleblicioglu D, Lopes JM, Kleihues P, Ohgaki H. Genetic profile of gliosarcomas. Am J Pathol. 2000; 156:425–432. PMID: 10666371.
Article8. Actor B, Cobbers JM, Büschges R, et al. Comprehensive analysis of genomic alterations in gliosarcoma and its two tissue components. Genes Chromosomes Cancer. 2002; 34:416–427. PMID: 12112531.
Article9. Ben Nsir A, Thai QA, Kassar AZ, Ben Said I, Jemel H. Primary cerebellar gliosarcoma with extracranial metastases: an orphan differential diagnosis. World Neurosurg. 2015; 84:2076.e13–2076.e17.
Article10. Ng HK, Poon WS. Gliosarcoma of the posterior fossa with features of a malignant fibrous histiocytoma. Cancer. 1990; 65:1161–1166. PMID: 2154322.
Article11. Nitta H, Hayase H, Moriyama Y, Yamashima T, Yamashita J. Gliosarcoma of the posterior cranial fossa: MRI findings. Neuroradiology. 1993; 35:279–280. PMID: 8492894.
Article12. Moon SK, Kim EJ, Choi WS, Ryu CW, Park BJ, Lee J. Gliosarcoma of the cerebellar hemisphere: a case report and review of the literature. Korean J Radiol. 2010; 11:566–570. PMID: 20808702.
Article13. Chikkannaiah P, Bharath RD, Sampath S, Santosh V. De novo gliosarcoma occurring in the posterior fossa of a 11-year-old girl. Clin Neuropathol. 2012; 31:389–391. PMID: 22939178.
Article14. Duan H, Kitazawa K, Yako T, Ichinose S, Kobayashi S, Sudo M. Gliosarcoma in the cerebellopontine angle with rapid tumor growth and intratumoral hemorrhage. World Neurosurg. 2016; 92:580.e17–580.e21.
Article15. Frandsen J, Orton A, Jensen R, et al. Patterns of care and outcomes in gliosarcoma: an analysis of the National Cancer Database. J Neurosurg. 2018; 128:1133–1138. PMID: 28621623.
Article16. Jain A, Correia J, Schweder P, McMahon A, Merola J, Aspoas R. Analysis of outcomes of multidisciplinary management of gliosarcoma: a single-center study, 2000-a2013. World Neurosurg. 2017; 106:30–36. PMID: 28642179.17. Han L, Zhang X, Qiu S, et al. Magnetic resonance imaging of primary cerebral gliosarcoma: a report of 15 cases. Acta Radiol. 2008; 49:1058–1067. PMID: 18766496.
Article18. Zhang BY, Chen H, Geng DY, et al. Computed tomography and magnetic resonance features of gliosarcoma: a study of 54 cases. J Comput Assist Tomogr. 2011; 35:667–673. PMID: 22082533.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Glioblastoma Occurred at Cerebello-pontine Angle: Case Report
- Trigeminal neuralgia Caused by Cerebello-pontine Angle Epidermoid Tumor
- MR Imaging of a Cerebello-Pontine Angle Epidermoid Cyst with a Malignant Transformation: Case Report
- Epidermoid Cyst in the Cerebello-Pontine Angle Associated with Trigeminal Neuralgia
- The radiographic findings of cerebello-pontine angle lesions