J Cerebrovasc Endovasc Neurosurg.
2018 Sep;20(3):191-197. 10.7461/jcen.2018.20.3.191.
STA-Distal ACA Bypass Using a Contralateral STA Interposition Graft for Symptomatic ACA Stenosis
- Affiliations
-
- 1Department of Neurosurgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Neurosurgery, National Health Insurance Service Ilsan Hospital, Goyang, Korea. yhlee@nhimc.or.kr
- KMID: 2422772
- DOI: http://doi.org/10.7461/jcen.2018.20.3.191
Abstract
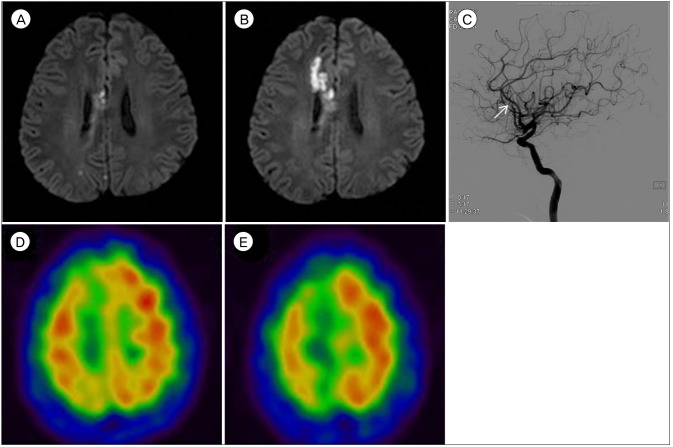
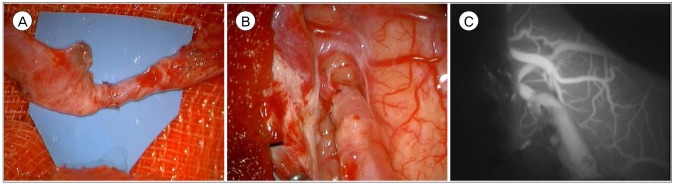
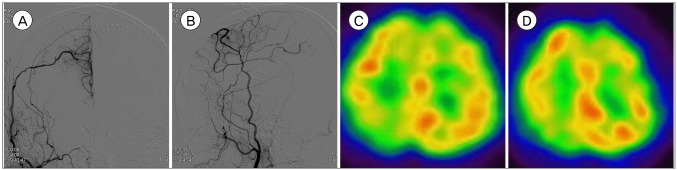
- Intracranial arterial stenosis usually occurs due to atherosclerosis and is considered the most common cause of stroke worldwide. Although the effectiveness of bypass surgery for ischemic stroke is controversial, the superficial temporal artery to the middle cerebral artery bypass for ischemic stroke is a common procedure. In our report, a 50-year-old man presented with sudden-onset left side weakness and dysarthria. An angiogram showed significant stenosis in the junction of the right cavernous-supraclinoid internal carotid artery and right pericallosal artery. Symptoms altered between improvement and deterioration. Magnetic resonance imaging showed a repeated progression of anterior cerebral artery (ACA) infarction despite maximal medical therapy. We performed a STA-ACA bypass with contralateral STA interposition. Postoperative course was uneventful with no further progression of symptoms. Thus, bypass surgery may be considered in patients with symptomatic stenosis or occlusion of the ACA, especially when patients present progressive symptoms despite maximal medical therapy.
MeSH Terms
Figure
Reference
-
1. Amin-Hanjani S, Barker FG 2nd, Charbel FT, Connolly ES Jr, Morcos JJ, Thompson BG, et al. Extracranial-intracranial bypass for stroke-is this the end of the line or a bump in the road? Neurosurgery. 2012; 9. 71(3):557–561. PMID: 22668888.2. Baron JC, Bousser MG, Rey A, Guillard A, Comar D, Castaigne P. Reversal of focal “misery-perfusion syndrome” by extra-intracranial arterial bypass in hemodynamic cerebral ischemia. A case study with 15O positron emission tomography. Stroke. 1981; Jul-Aug. 12(4):454–459. PMID: 6976022.
Article3. Carlson AP, Yonas H, Chang YF, Nemoto EM. Failure of cerebral hemodynamic selection in general or of specific positron emission tomography methodology?: Carotid Occlusion Surgery Study (COSS). Stroke. 2011; 12. 42(12):3637–3639. PMID: 21960571.4. Carvalho M, Oliveira A, Azevedo E, Bastos-Leite AJ. Intracranial arterial stenosis. J Stroke Cerebrovasc Dis. 2014; 4. 23(4):599–609. PMID: 23850084.
Article5. Group JS. Japanese EC-IC Bypass Trial (JET Study). Surg Cereb Stroke. 2002; 30(6):434–437.6. Grubb RL Jr, Derdeyn CP, Fritsch SM, Carpenter DA, Yundt KD, Videen TO, et al. Importance of hemodynamic factors in the prognosis of symptomatic carotid occlusion. JAMA. 1998; 9. 280(12):1055–1060. PMID: 9757852.
Article7. Horiuchi T, Ichinose S, Agata M, Ito K, Hongo K. STA-ACA bypass using the ipsilateral free STA graft as an interposition graft and A3–A3 anastomosis for treatment of bilateral ACA steno-occlusive ischemia. Acta Neurochir (Wien). 018; 4. 160(4):779–782. PMID: 29349672.
Article8. Ikeda A, Okada T, Shibuya M, Noda S, Sugiura M, Iguchi I, et al. Revascularization of the anterior cerebral artery. Report of two cases. J Neurosurg. 1985; 4. 62(4):603–606. PMID: 3973733.9. Ishii R, Koike T, Takeuchi S, Ohsugi S, Tanaka R, Konno K. Anastomosis of the superficial temporal artery to the distal anterior cerebral artery with interposed cephalic vein graft. Case report. J Neurosurg. 1983; 3. 58(3):425–429. PMID: 6827332.10. Ito Z. A new technique of intracranial interarterial anastomosis between distal anterior cerebral arteries (ACA) for ACA occlusion and its indication. Neurol Med Chir (Tokyo). 1981; 9. 21(9):931–939. PMID: 6171745.
Article11. Kang SY, Kim JS. Anterior cerebral artery infarction: Stroke mechanism and clinical-imaging study in 100 patients. Neurology. 2008; 6. 10. 70:2386. PMID: 18541871.
Article12. Kiyofuji S, Inoue T, Hasegawa H, Tamura A, Saito I. A3–A3 anastomosis and superficial temporal artery-radial artery graft-A3 bypass to treat bilateral ACA steno-occlusive hemodynamic ischemia with cognitive and executive dysfunction: a technical note. Acta Neurochir (Wien). 2014; 11. 156(11):2085–2093. discussion 2093. PMID: 25248326.
Article13. Lee SC, Ahn JH, Kang HS, Kim JE. Revascularization for symptomatic occlusion of the anterior cerebral artery using superficial temporal artery. J Korean Neurosurg Soc. 2013; 12. 54(6):511–514. PMID: 24527195.
Article14. Nagm A, Horiuchi T, Yanagawa T, Hongo K. Risky Cerebrovascular anatomic orientation: implications for brain revascularization. World Neurosurg. 2016; 12. 96:610.e15–610.e20.
Article15. Park ES, Ahn JS, Park JC, Kwon DH, Kwun BD, Kim CJ. STA-ACA bypass using the contralateral STA as an interposition graft for the treatment of complex ACA aneurysms: report of two cases and a review of the literature. Acta Neurochir (Wien). 2012; 8. 154(8):1447–1453. PMID: 22692589.
Article16. Powers WJ, Clarke WR, Grubb RL Jr, Videen TO, Adams HP Jr, Derdeyn CP, et al. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the Carotid Occlusion Surgery Study randomized trial. JAMA. 2011; 11. 306(18):1983–1992. PMID: 22068990.17. Sánchez-Sánchez C, Egido JA, González-Gutiérrez JL, Mera-Campillo J, Carneado-Ruiz J, Díaz-Otero F. Stroke and intracranial stenosis: clinical profile in a series of 134 patients in Spain. Rev Neurol. 2004; 8. 39(4):305–311. PMID: 15340886.18. Terasaka S, Satoh M, Echizenya K, Murai H, Fujimoto S, Asaoka K. Revascularization of the anterior cerebral artery using a free superficial temporal artery graft: a case report. Surg Neurol. 1997; 8. 48(2):164–169. discussion 169-70. PMID: 9242243.
Article19. Vemmos KN, Takis CE, Georgilis K, Zakopoulos NA, Lekakis JP, Papamichael CM, et al. The Athens stroke registry: results of a five-year hospital-based study. Cerebrovasc Dis. 2000; Mar-Apr. 10(2):133–141. PMID: 10686452.
Article20. Wityk RJ, Lehman D, Klag M, Coresh J, Ahn H, Litt B. Race and sex differences in the distribution of cerebral atherosclerosis. Stroke. 1996; 11. 27(11):1974–1980. PMID: 8898801.
Article21. Yasargil MG. Experimental small vessel surgery in the dog including patching and grafting of cerebral vessels and the formation of functional extra-intracranial shunts. In : Donaghy RMP, Yasargil MG, editors. Micro-vascular Surgery. Stuttgart: Georg Thieme Verlag;1967. p. 87–126.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Revascularization for Symptomatic Occlusion of the Anterior Cerebral Artery Using Superficial Temporal Artery
- Emergency In Situ Bypass during Middle Cerebral Artery Aneurysm Surgery: Middle Cerebral Artery-Superficial Temporal Artery Interposition Graft-Middle Cerebral Artery Anastomosis
- Assessing the Adequacy of Superficial Temporal Artery Blood Flow in Korean Patients Undergoing STA-MCA Anastomosis
- Changes in Bypass Flow during Temporary Occlusion of Unused Branch of Superficial Temporal Artery
- Augmentation of the Patency of an Extracranial-Intracranial Bypass Accompanied by the Occlusion of an Intracranial Stenotic Lesion