Ann Pediatr Endocrinol Metab.
2018 Sep;23(3):113-118. 10.6065/apem.2018.23.3.113.
Clinical characteristics in Japanese children with nonobese type 2 diabetes
- Affiliations
-
- 1Department of Pediatrics, Nihon University School of Medicine, Tokyo, Japan. urakami.tatsuhiko@nihon-u.ac.jp
- KMID: 2422473
- DOI: http://doi.org/10.6065/apem.2018.23.3.113
Abstract
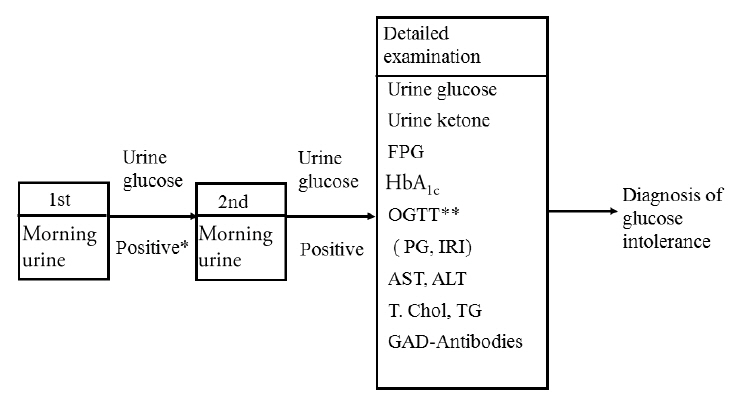
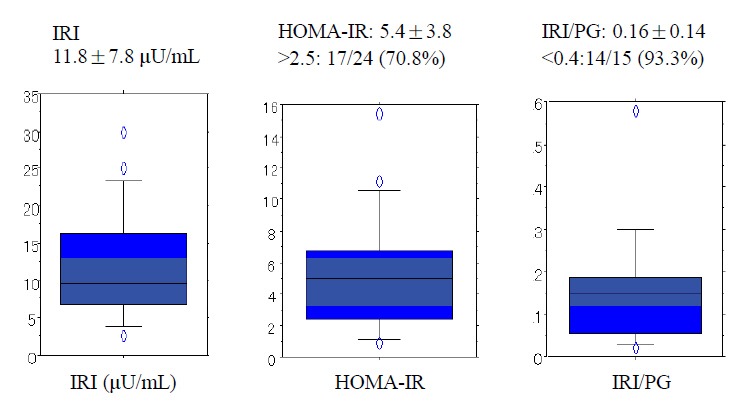
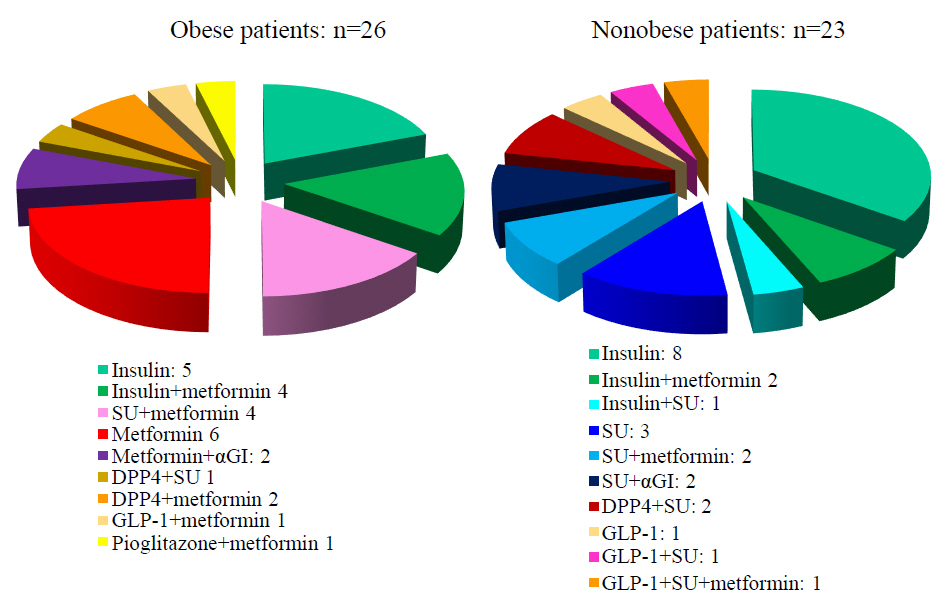
- It is well known that the incidence of youth-onset type 2 diabetes is increasing worldwide. On the other hand, most studies have shown that the majority of youth-onset type 2 diabetes occurs in obese individuals, generally with a body mass index (BMI) greater than the 90th or 95th centile for sex- and age-matched children and adolescents. However, we identified some Japanese children with nonobese type 2 diabetes and BMI less than 90th centile by a urine glucose screening program at schools in the Tokyo Metropolitan Area. According to the results obtained from the screening, clinical characteristics of patients with nonobese type 2 diabetes seemed to be different from those in obese type 2 diabetes. Nonobese patients tended to show lower insulin secretion abilities and milder, but evident, insulin resistance from the time of diagnosis. Female, low birth weight (small for gestational age), and genetic background, not related to β-cell-associated autoimmunity, may play a role in development of nonobese type 2 diabetes. In addition, nonobese patients tend to progress earlier to pharmacological treatment including oral hypoglycemic drugs and insulin. Further studies are needed to confirm to these findings and clarify the pathophysiology of children with nonobese type 2 diabetes.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Zeitler P, Fu J, Tandon N, Nadeau K, Urakami T, Barrett T, et al. ISPAD Clinical Practice Consensus Guidelines 2014. Type 2 diabetes in the child and adolescent. Pediatr Diabetes. 2014; 15 Suppl 20:26–46.2. Mayer-Davis EJ, Lawrence JM, Dabelea D, Divers J, Isom S, Dolan L, et al. Incidence trends of type 1 and type 2 diabetes among youths, 2002-2012. N Engl J Med. 2017; 376:1419–29.
Article3. Fu JF, Liang L, Gong CX, Xiong F, Luo FH, Liu GL, et al. Status and trends of diabetes in Chinese children: analysis of data from 14 medical centers. World J Pediatr. 2013; 9:127–34.
Article4. Dabelea D, Mayer-Davis EJ, Saydah S, Imperatore G, Linder B, Divers J, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014; 311:1778–86.
Article5. Urakami T, Miyamoto Y, Fujita H, Kitagawa T. Type 1 (insulin-dependent) diabetes in Japanese children is not a uniform disease. Diabetologia. 1989; 32:312–5.
Article6. Urakami T, Kubota S, Nitadori Y, Harada K, Owada M, Kitagawa T. Annual incidence and clinical characteristics of type 2 diabetes in children as detected by urine glucose screening in the Tokyo metropolitan area. Diabetes Care. 2005; 28:1876–81.
Article7. Urakami T, Morimoto S, Nitadori Y, Harada K, Owada M, Kitagawa T. Urine glucose screening program at schools in Japan to detect children with diabetes and its outcome-incidence and clinical characteristics of childhood type 2 diabetes in Japan. Pediatr Res. 2007; 61:141–5.
Article8. Urakami T, Suzuki J, Mugishima H, Amemiya S, Sugihara S, Kawamura T, et al. Screening and treatment of childhood type 1 and type 2 diabetes mellitus in Japan. Pediatr Endocrinol Rev. 2012; 10 Suppl 1:51–61.9. Urakami T, Miyata M, Yoshida K, Mine Y, Kuwabara R, Aoki M, et al. Changes in annual incidence of school children with type 2 diabetes in the Tokyo Metropolitan Area during 1975-2015. Pediatr Diabetes;2018.10. Urakami T, Miyamoto Y, Matsunaga H, Owada M, Kitagawa T. Serial changes in the prevalence of islet cell antibodies and islet cell antibody titer in children with IDDM of abrupt or slow onset. Diabetes Care. 1995; 18:1095–9.
Article11. Urakami T, Suzuki J, Yoshida A, Saito H, Mugishima H. Incidence of children with slowly progressive form of type 1 diabetes detected by the urine glucose screening at schools in the Tokyo Metropolitan Area. Diabetes Res Clin Pract. 2008; 80:473–6.
Article12. Zimmet PZ, Tuomi T, Mackay IR, Rowley MJ, Knowles W, Cohen M, et al. Latent autoimmune diabetes mellitus in adults (LADA): the role of antibodies to glutamic acid decarboxylase in diagnosis and prediction of insulin dependency. Diabet Med. 1994; 11:299–303.
Article13. Naik RG, Brooks-Worrell BM, Palmer JP. Latent autoimmune diabetes in adults. J Clin Endocrinol Metab. 2009; 94:4635–44.
Article14. Urakami T, Kuwabara R, Habu M, Okuno M, Suzuki J, Takahashi S, et al. Clinical characteristics of non-obese children with type 2 diabetes mellitus without involvement of β-cell autoimmunity. Diabetes Res Clin Pract. 2013; 99:105–11.
Article15. Sugihara S, Sasaki N, Amemiya S, Kohno H, Tanaka T, Matsuura N. Analysis of weight at birth and at diagnosis of childhood-onset type 2 diabetes mellitus in Japan. Pediatr Diabetes. 2008; 9(4 Pt 1):285–90.
Article16. Morimoto S, Urakami T. Insulin resistance during puberty in non-obese Japanese children. Clin Pediatr Endocrinol. 2011; 20:1–6.
Article17. Urakami T, Habu M, Kuwabara R, Komiya K, Nagano N, Suzuki J, et al. Insulin resistance at diagnosis in Japanese children with type 2 diabetes mellitus. Pediatr Int. 2012; 54:516–9.
Article18. Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006; 368:1681–8.
Article19. Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009; 301:2129–40.20. Tfayli H, Bacha F, Gungor N, Arslanian S. Phenotypic type 2 diabetes in obese youth: insulin sensitivity and secretion in islet cell antibody-negative versus -positive patients. Diabetes. 2009; 58:738–44.21. Urakami T, Kuwabara R, Habu M, Yoshida A, Okuno M, Suzuki J, et al. Pharmacologic treatment strategies in children with type 2 diabetes mellitus. Clin Pediatr Endocrinol. 2013; 22:1–8.
Article22. Urakami T. New insights into the pharmacological treatment of pediatric patients with type 2 diabetes. Clin Pediatr Endocrinol. 2018; 27:1–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Fulminant Type 1 Diabetes
- The Clinical Types and Characteristics of Diabetes Mellitus in Korean Children
- Pancreatogenic Diabetes
- Tumor Necrosis Factor and Lymphotoxin-alpha Gene Polymorphism in Korean Children with Type 1 Diabetes
- Comparison of Insulin-Treated Patients with Ambiguous Diabetes Type with Definite Type 1 and Type 2 Diabetes Mellitus Subjects: A Clinical Perspective