Korean J Ophthalmol.
2018 Oct;32(5):361-368. 10.3341/kjo.2017.0095.
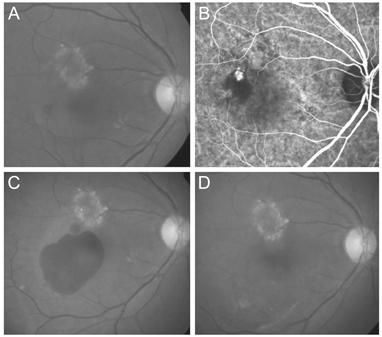
Development of Submacular Hemorrhage in Neovascular Age-related Macular Degeneration: Influence on Visual Prognosis in a Clinical Setting
- Affiliations
-
- 1Department of Ophthalmology, Konyang University College of Medicine, Daejeon, Korea.
- 2Department of Ophthalmology, Kim's Eye Hospital, Konyang University College of Medicine, Seoul, Korea. kimoph@gmail.com
- KMID: 2422065
- DOI: http://doi.org/10.3341/kjo.2017.0095
Abstract
- PURPOSE
This study aimed to evaluate changes in visual acuity before and after the development of submacular hemorrhage secondary to neovascular age-related macular degeneration (AMD) and to compare the visual outcomes between patients with and without hemorrhage.
METHODS
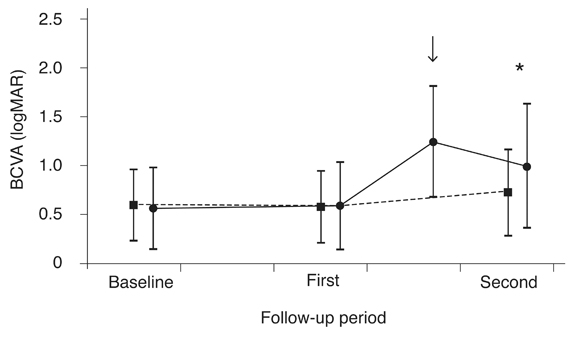
This retrospective observational study included 124 patients with neovascular AMD. Patients who developed a submacular hemorrhage involving the fovea were included in the hemorrhage group (n = 55). Patients with no sign of submacular hemorrhage during the follow-up period were included in the no-hemorrhage group (n = 69). Visual outcomes were compared between the two groups.
RESULTS
The logarithm of the minimal angle of resolution best-corrected visual acuity (BCVA) before the development of submacular hemorrhage, once the hemorrhage had developed, and 6 months after the development of hemorrhage was 0.59 ± 0.45, 1.24 ± 0.57, and 0.99 ± 0.64, respectively. BCVA was significantly worse 6 months after the hemorrhage compared to before the hemorrhage (p < 0.001). The BCVA before the development of hemorrhage (measured at a mean of 12.9 months after diagnosis) was comparable to that of the no-hemorrhage group (mean, 0.58 ± 0.37 at a mean of 12.4 months). However, the BCVA 6 months after identification of hemorrhage (mean, 21.5 months) was significantly worse in the hemorrhage group than in the no-hemorrhage group (mean, 0.73 ± 0.44 at mean 21.2 months) (p = 0.018).
CONCLUSIONS
Visual acuity was significantly worse after hemorrhage than before hemorrhage, even after treatment. In addition, patients with submacular hemorrhage had markedly worse visual outcomes than patients without hemorrhage. This result suggests that the development of hemorrhage during the treatment course of neovascular AMD has a devastating effect on visual prognosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Avery RL, Fekrat S, Hawkins BS, Bressler NM. Natural history of subfoveal subretinal hemorrhage in age-related macular degeneration. Retina. 1996; 16:183–189.
Article2. Bressler NM, Bressler SB, Childs AL, et al. Surgery for hemorrhagic choroidal neovascular lesions of age-related macular degeneration: ophthalmic findings: SST report no. 13. Ophthalmology. 2004; 111:1993–2006.3. Scupola A, Coscas G, Soubrane G, Balestrazzi E. Natural history of macular subretinal hemorrhage in age-related macular degeneration. Ophthalmologica. 1999; 213:97–102.
Article4. Hassan AS, Johnson MW, Schneiderman TE, et al. Management of submacular hemorrhage with intravitreous tissue plasminogen activator injection and pneumatic displacement. Ophthalmology. 1999; 106:1900–1906.5. Haupert CL, McCuen BW 2nd, Jaffe GJ, et al. Pars plana vitrectomy, subretinal injection of tissue plasminogen activator, and fluid-gas exchange for displacement of thick submacular hemorrhage in age-related macular degeneration. Am J Ophthalmol. 2001; 131:208–215.
Article6. Kamei M, Tano Y, Maeno T, et al. Surgical removal of submacular hemorrhage using tissue plasminogen activator and perfluorocarbon liquid. Am J Ophthalmol. 1996; 121:267–275.
Article7. Chang MA, Do DV, Bressler SB, et al. Prospective one-year study of ranibizumab for predominantly hemorrhagic choroidal neovascular lesions in age-related macular degeneration. Retina. 2010; 30:1171–1176.
Article8. Kim JH, Chang YS, Kim JW, et al. Intravitreal anti-vascular endothelial growth factor for submacular hemorrhage from choroidal neovascularization. Ophthalmology. 2014; 121:926–935.
Article9. Shienbaum G, Garcia Filho CA, Flynn HW Jr, et al. Management of submacular hemorrhage secondary to neovascular age-related macular degeneration with anti-vascular endothelial growth factor monotherapy. Am J Ophthalmol. 2013; 155:1009–1013.
Article10. Stifter E, Michels S, Prager F, et al. Intravitreal bevacizumab therapy for neovascular age-related macular degeneration with large submacular hemorrhage. Am J Ophthalmol. 2007; 144:886–892.
Article11. Altaweel MM, Daniel E, Martin DF, et al. O utcomes of eyes with lesions composed of >50% blood in the Comparison of Age-related Macular Degeneration Treatments Trials (CATT). Ophthalmology. 2015; 122:391–398.12. Shin JY, Lee JM, Byeon SH. Anti-vascular endothelial growth factor with or without pneumatic displacement for submacular hemorrhage. Am J Ophthalmol. 2015; 159:904–914.13. Kim KH, Kim JH, Chang YS, et al. Clinical outcomes of eyes with submacular hemorrhage secondary to age-related macular degeneration treated with anti-vascular endothelial growth factor. Korean J Ophthalmol. 2015; 29:315–324.
Article14. Shin KH, Lee TG, Kim JH, et al. The efficacy of intravitreal aflibercept in submacular hemorrhage secondary to wet age-related macular degeneration. Korean J Ophthalmol. 2016; 30:369–376.
Article15. Cho JH, Ryoo NK, Cho KH, et al. Incidence rate of massive submacular hemorrhage and its risk factors in polypoidal choroidal vasculopathy. Am J Ophthalmol. 2016; 169:79–88.
Article16. Kim KM, Kim JH, Chang YS, et al. Long-term outcomes in patients with neovascular age-related macular degeneration who maintain dry macula after three monthly ranibizumab injections. Semin Ophthalmol. 2018; 33:371–376.
Article17. Kuroda Y, Yamashiro K, Miyake M, et al. Factors associated with recurrence of age-related macular degeneration after anti-vascular endothelial growth factor treatment: a retrospective cohort study. Ophthalmology. 2015; 122:2303–2310.18. Hesgaard HB, Torkashvand M, la Cour M. Failure to detect an effect of pneumatic displacement in the management of submacular haemorrhage secondary to age-related macular degeneration: a retrospective case series. Acta Ophthalmol. 2012; 90:e498–e500.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravitreal Aflibercept Monotherapy for Treating Submacular Hemorrhage Secondary to Neovascular Age-related Macular Degeneration
- The Effect of Intrav it real Injection of tPA and C3F8 Gas in Submacular Hemorrhage
- Intravitreal Injection of tPA and Gas for Submacular Hemorrhage Associated with Age-related Macular Degeneration
- Pneumatic Displacement of Submacular Hemorrhage with Intravitreal Injection of tPA and SF6 Gas
- Pneumatic Displacement of Submacular Hemorrhage with Intravitreal Injection of SF6 Gas without Tissue Plasminogen Activator