Korean J Health Promot.
2018 Sep;18(3):127-137. 10.15384/kjhp.2018.18.3.127.
Gender Perspectives on the Relationship between Red and Processed Meat Intake and Colorectal Cancer: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Center for Gendered Innovations in Science and Technology Research (GISTeR), Korea Federation of Women's Science & Technology Associations, Seoul, Korea. hypaik@kofwst.org
- 2Department of Food and Nutrition, Seoul National University, Seoul, Korea.
- 3Research Institute of Human Ecology, Seoul National University, Seoul, Korea.
- 4Department of Food and Nutrition, Daejeon University, Daejeon, Korea.
- 5Daejeon Dong-gu Center for Children's Food Service Management, Daejeon, Korea.
- KMID: 2421871
- DOI: http://doi.org/10.15384/kjhp.2018.18.3.127
Abstract
- BACKGROUND
Men and women choose different food items, and consume different amounts of food, due to biological, cultural, and social differences. However, when dietary assessment instruments are developed, gender differences in food selection and/or the portion sizes are often not considered.
METHODS
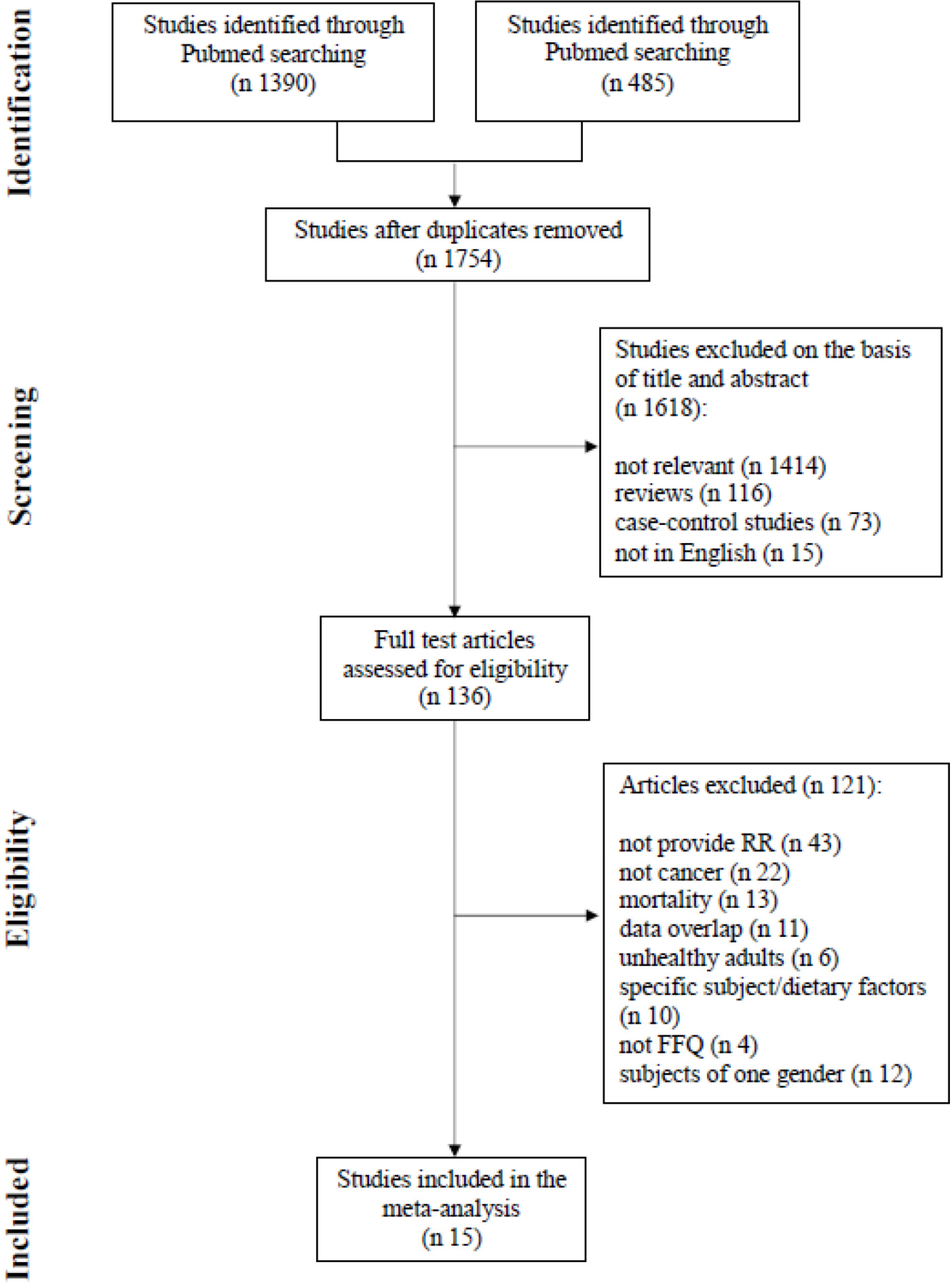
Prospective cohort studies with men and women that examined the association between red or processed meat intake and colorectal cancer and published up to July 2017, were identified using PubMed. Studies were categorized as gender-specific (GS) group if the Food Frequency Questionnaire was developed using gender-specific data, and as not gender-specific (NGS) group if not gender-specific data were used.
RESULTS
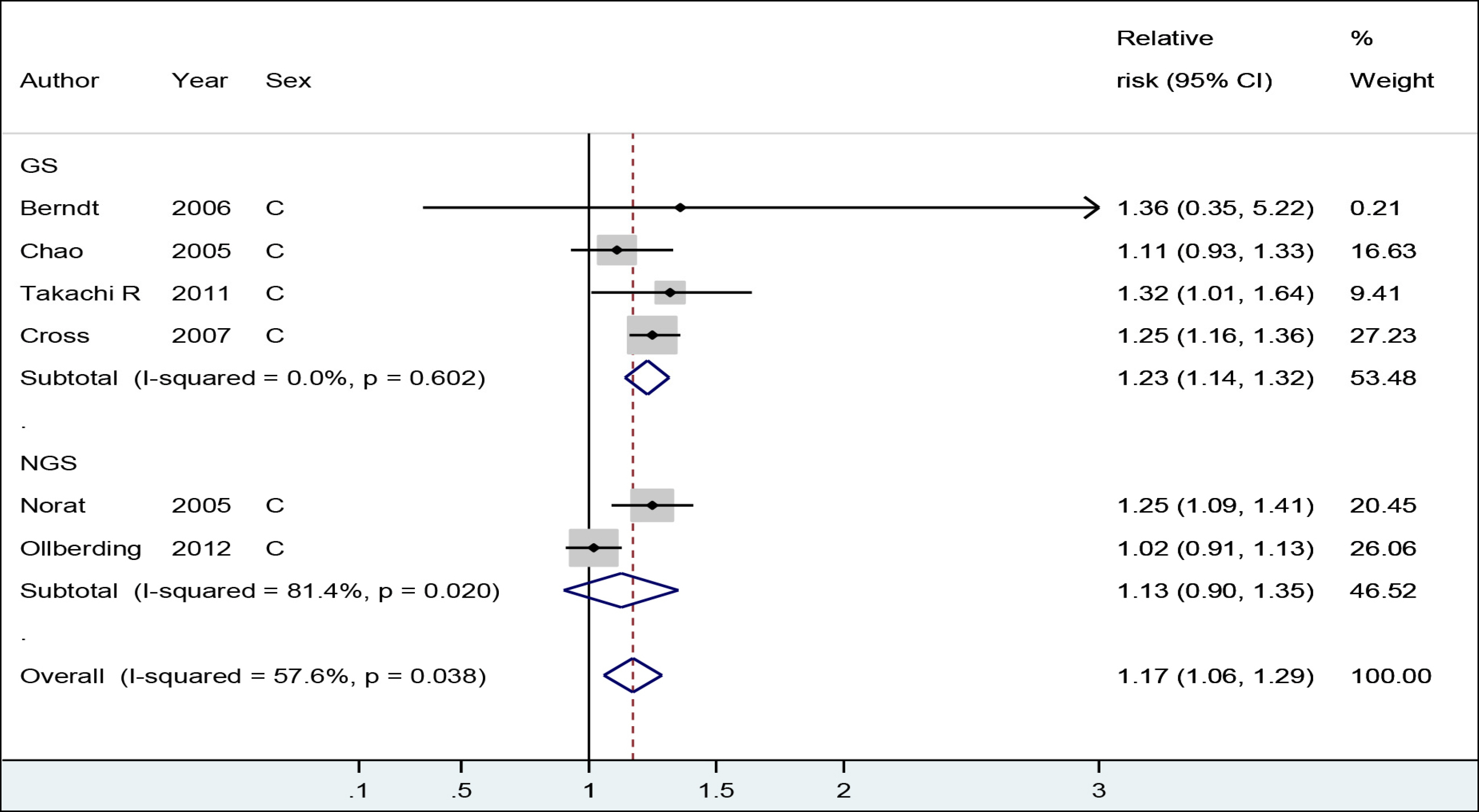
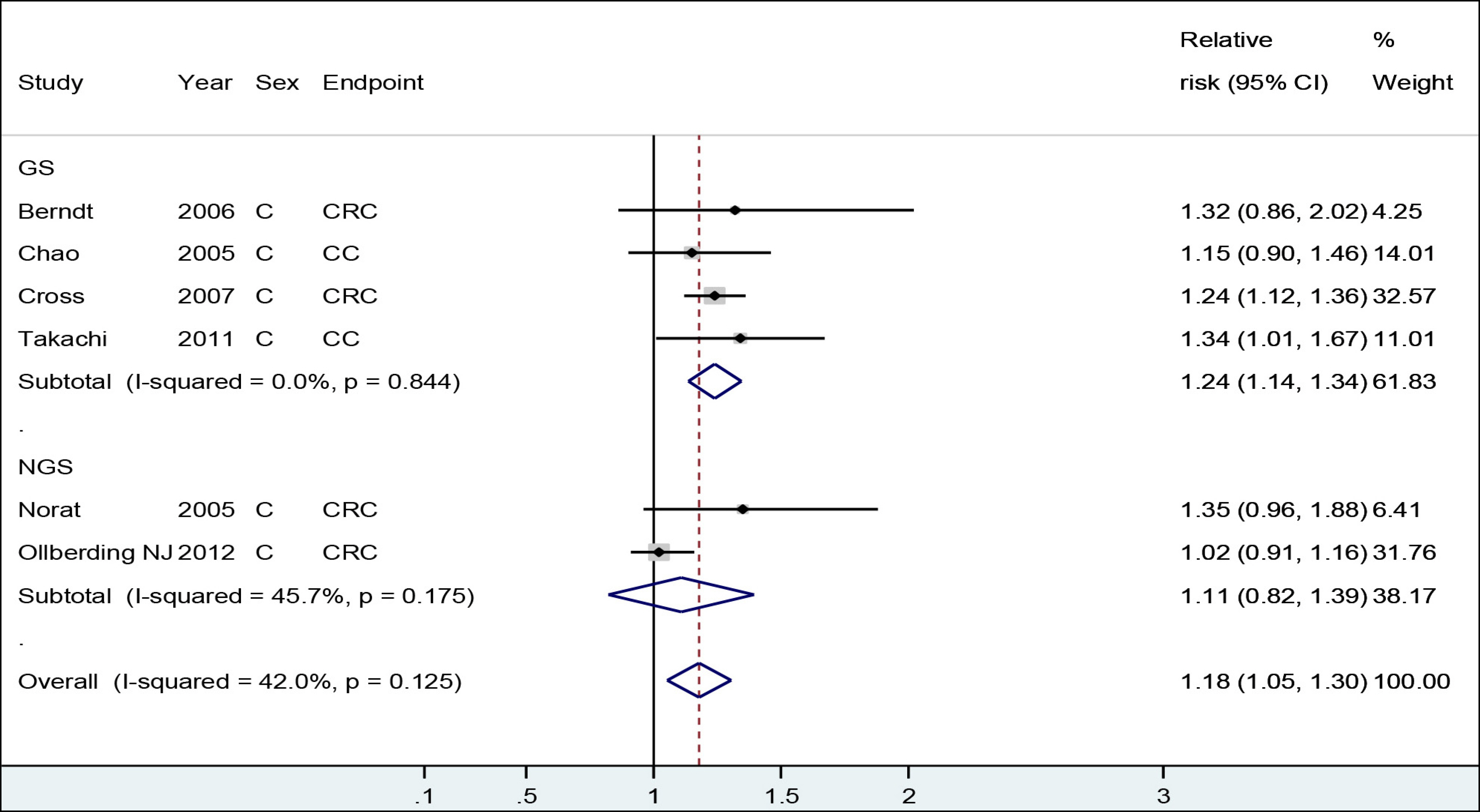
For cohort studies that reported combined intake estimates of men and women, a 100 g/day increment in red and processed meat intake was positively associated with a risk of colorectal or colon cancer in GS group (relative risk [RR], 1.23; 95% confidence interval [CI], 1.14-1.32) but not in NGS group (RR, 1.13; 95% CI, 0.90-1.35). For processed meat, the RR for 50 g/day increase was 1.28 (95% CI, 1.15-1.40) in GS group and 1.15 (95% CI, 1.03-1.27) in NGS group.
CONCLUSIONS
Gender differences need to be considered during development of dietary assessment tools because this may improve the quality of the findings of nutritional epidemiological studies.
MeSH Terms
Figure
Reference
-
References
1. Gender, women and Health. [Internet]. Geneva: World Health Organization;2015. [Accessed August 31, 2017] Available from:. https://www.legal-tools.org/doc/a33dc3/pdf/.2. Schiebinger L, Schraudner M. Interdisciplinary approaches to achieving gendered innovations in science, medicine, and engineering. Interdiscip Sci Rev. 2011; 36(2):154–67.3. Bates CJ, Prentice A, Finch S. Gender differences in food and nutrient intakes and status indices from the National Diet and Nutrition Survey of people aged 65 years and over. Eur J Clin Nutr. 1999; 53(9):694–9.4. Wardle J, Haase AM, Steptoe A, Nillapun M, Jonwutiwes K, Bellisle F. Gender differences in food choice: the contribution of health beliefs and dieting. Ann Behav Med. 2004; 27(2):107–16.
Article5. Turrell G. Determinants of gender differences in dietary behavior. Nutr Res. 1997; 17(7):1105–20.
Article6. Brug J, Tak NI, te Velde SJ, Bere E, de Bourdeaudhuij I. Taste preferences, liking and other factors related to fruit and vegetable intakes among schoolchildren: results from observational studies. Br J Nutr. 2008; 99(Suppl 1):S7–14.
Article7. Blaak E. Gender differences in fat metabolism. Curr Opin Clin Nutr Metab Care. 2001; 4(6):499–502.
Article8. Tarnopolsky MA. Females and males: should nutritional recommendations be gender specific? Schweiz Z Med Traumatol. 2003; 51(1):39–46.9. Wu BN, O'Sullivan AJ. Sex differences in energy metabolism need to be considered with lifestyle modifications in humans. J Nutr Metab. 2011; 2011:391809.
Article10. Lee H, Kang M, Song WO, Shim JE, Paik HY. Gender analysis in the development and validation of FFQ: a systematic review. Br J Nutr. 2016; 115(4):666–71.
Article11. Willett W. Nutritional epidemiology. 3rd ed.New York: Oxford University Press;2012. p. 70–141.12. Bouvard V, Loomis D, Guyton KZ, Grosse Y, Ghissassi FE, Benbrahim-Tallaa L, et al. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015; 16(16):1599–600.
Article13. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000; 283(15):2008–12.14. Sato Y, Nakaya N, Kuriyama S, Nishino Y, Tsubono Y, Tsuji I. Meat consumption and risk of colorectal cancer in Japan: the Miyagi cohort study. Eur J Cancer Prev. 2006; 15(3):211–8.
Article15. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986; 7(3):177–88.
Article16. Orsini N, Bellocco R, Greenland S. Generalized least squares for trend estimation of summarized doseresponse data. Stata J. 2006; 6(1):40–57.
Article17. Chan DS, Lau R, Aune D, Vieira R, Greenwood DC, Kampman E, et al. Red and processed meat and colorectal cancer incidence: metaanalysis of prospective studies. PLoS One. 2011; 6(6):e20456.
Article18. Kang M, Park S, Boushey CJ, Wilkens LR, et al. Portion sizes from 24-hour dietary recalls differed by sex among those who selected the same portion size category on a food frequency questionnaire. J Acad of Nutr Diet. 2018; 118(9):1711–8.
Article19. Marks GC, Hughes MC, van der Pols JC. The effect of personal characteristics on the validity of nutrient intake estimates using a food-frequency questionnaire. Public Health Nutr. 2006; 9(3):394–402.
Article20. Marks GC, Hughes MC, van der Pols JC. Relative validity of food intake estimates using a food frequency questionnaire is associated with sex, age, and other personal characteristics. J Nutr. 2006; 136(2):459–65.
Article21. Cade JE, Burley VJ, Warm DL, Thompson RL, Margetts BM. Food-frequency questionnaires: a review of their design, validation and utilisation. Nutr Res Rev. 2004; 17(1):5–22.
Article22. Berndt SI, Platz EA, Fallin MD, Thuita LW, Hoffman SC, Helzlsouer KJ. Genetic variation in the nucleotide excision repair pathway and colorectal cancer risk. Cancer Epidemiol Biomarkers Prev. 2006; 15(11):2263–9.
Article23. Chao A, Thun MJ, Connell CJ, McCullough ML, Jacobs EJ, Flanders WD, et al. Meat consumption and risk of colorectal cancer. JAMA. 2005; 293(2):172–82.
Article24. Takachi R, Tsubono Y, Baba K, Inoue M, Sasazuki S, Iwasaki M, et al. Red meat intake may increase the risk of colon cancer in Japanese, a population with relatively low red meat consumption. Asia Pac J Clin Nutr. 2011; 20(4):603–12.25. English DR, MacInnis RJ, Hodge AM, Hopper JL, Haydon AM, Giles GG. Red meat, chicken, and fish consumption and risk of colorectal cancer. Cancer Epidemiol Biomarkers Prev. 2004; 13(9):1509–14.26. Cross AJ, Leitzmann MF, Gail MH, Hollenbeck AR, Schatzkin A, Sinha R. A prospective study of red and processed meat intake in relation to cancer risk. PLoS Med. 2007; 4(12):e325.
Article27. Singh PN, Fraser GE. Dietary risk factors for colon cancer in a low-risk population. Am J Epidemiol. 1998; 148(8):761–74.
Article28. Norat T, Bingham S, Ferrari P, Slimani N, Jenab M, Mazuir M, et al. Meat, fish, and colorectal cancer risk: the European prospective investigation into cancer and nutrition. J Natl Cancer Inst. 2005; 97(12):906–16.29. Järvinen R, Knekt P, Hakulinen T, Rissanen H, Heliövaara M. Dietary fat, cholesterol and colorectal cancer in a prospective study. Br J Cancer. 2001; 85(3):357–61.
Article30. Knekt P, Järvinen R, Dich J, Hakulinen T. Risk of colorectal and other gastrointestinal cancers after exposure to nitrate, nitrite and N-nitroso compounds: a follow-up study. Int J Cancer. 1999; 80(6):852–6.31. Iso H, Kubota Y. Japan Collaborative Cohort Study for Evaluation of Cancer. Nutrition and disease in the Japan collaborative cohort study for evaluation of cancer (JACC). Asian Pac J Cancer Prev. 2007; 8(Suppl):35–80.32. Ollberding NJ, Wilkens LR, Henderson BE, Kolonel LN, Le Marchand L. Meat consumption, heterocyclic amines and colorectal cancer risk: the Multiethnic Cohort Study. Int J Cancer. 2012; 131(7):E1125–33.
Article33. Chen J, Stampfer MJ, Hough HL, Garcia-Closas M, Willett WC, Hennekens CH, et al. A prospective study of N-acetyltransferase genotype, red meat intake, and risk of colorectal cancer. Cancer Res. 1998; 58(15):3307–11.34. Balder HF, Vogel J, Jansen MC, Weijenberg MP, van den Brandt PA, Westenbrink S, et al. Heme and chlorophyll intake and risk of colorectal cancer in the Netherlands cohort study. Cancer Epidemiol Biomarkers Prev. 2006; 15(4):717–25.
Article35. Wada K, Oba S, Tsuji M, Tamura T, Konishi K, Goto Y, et al. Meat consumption and colorectal cancer risk in Japan: the Takayama study. Cancer Sci. 2017; 108(5):1065–70.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nutritional Issues for Colorectal Cancer Prevention
- Estimation of Usual Meat Intake Distribution Considering Meat Content in Processed Foods: Based on the KNHANES 2009
- The Colorectal Cancer Risk of Meat Intake, Smoking, and CYP2E1 Polymorphisms: The Comparison of Colorectal Cancer Patients with Controls
- Population Attributable Fraction of Established Modifiable Risk Factors on Colorectal Cancer in Korea
- Intake Trends of Red Meat, Alcohol, and Fruits and Vegetables as Cancer-Related Dietary Factors from 1998 to 2009