Allergy Asthma Immunol Res.
2017 Nov;9(6):517-525. 10.4168/aair.2017.9.6.517.
Seasonal Cycle and Relationship of Seasonal Rhino- and Influenza Virus Epidemics With Episodes of Asthma Exacerbation in Different Age Groups
- Affiliations
-
- 1Department of Pediatrics, CHA University School of Medicine, Seongnam, Korea. drmesh@gmail.com
- 2Department of Pediatrics, CHA Gangnam Medical Center, CHA University School of Medicine, Seoul, Korea.
- 3Department of Pediatrics, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea.
- 5Department of Biomedical Science, CHA University School of Medicine, Seongnam, Korea.
- 6Division of Respiratory Viruses Center for Infectious Diseases, National Institutes of Health, Korea Centers for Disease Control and Prevention, Cheongju, Korea.
- KMID: 2421662
- DOI: http://doi.org/10.4168/aair.2017.9.6.517
Abstract
- PURPOSE
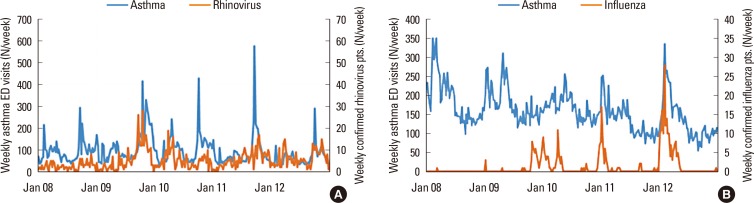
Seasonal variations in asthma exacerbation (AE) are associated with respiratory virus outbreaks and the return of children to school after vacation. This study aims to elucidate the period, phase, and amplitude of seasonal cycles of AE in 5 different age groups with regard to rhino- and influenza virus epidemics in Korea.
METHODS
The number of daily emergency department (ED) visits for AE in all age groups of Korea and the nationwide weekly incidence of rhino- and influenza virus, were obtained for 2008-2012. Fourier regression was used to model rhythmicity, and the Cosinor method was used to determine the amplitude and phase of the cycles in each age group. The cross-correlation function (CCF) between AE and the rhino- and influenza virus epidemics was also calculated.
RESULTS
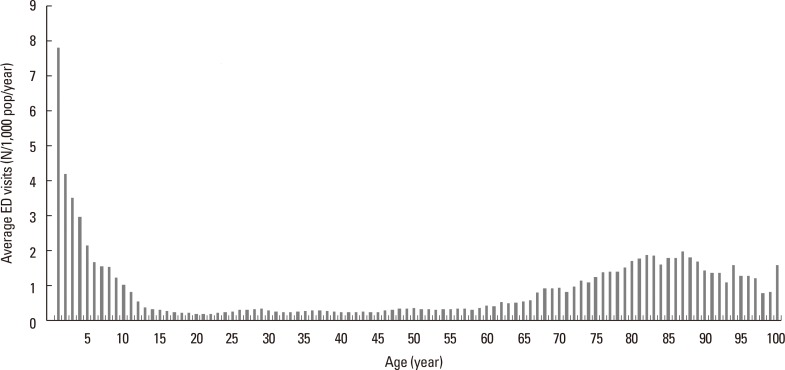
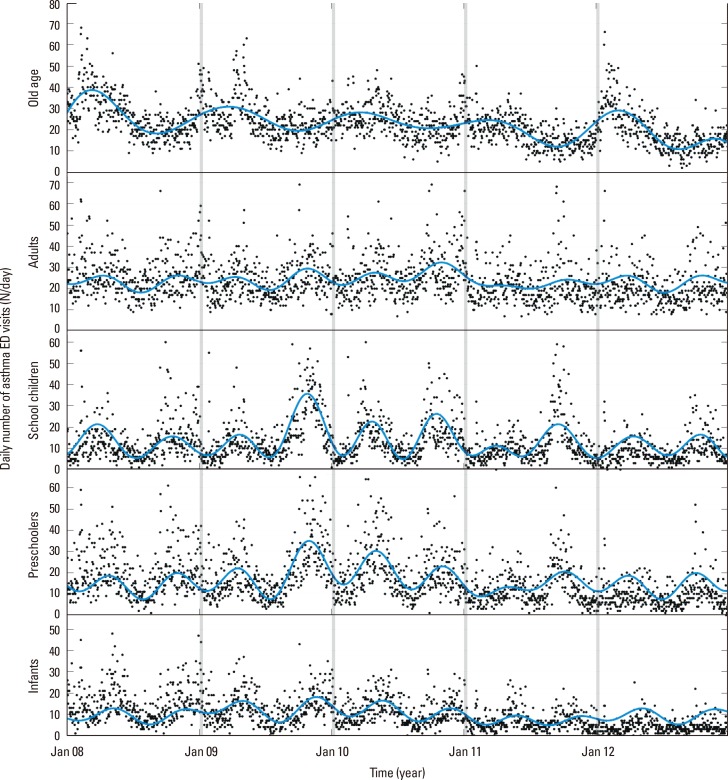
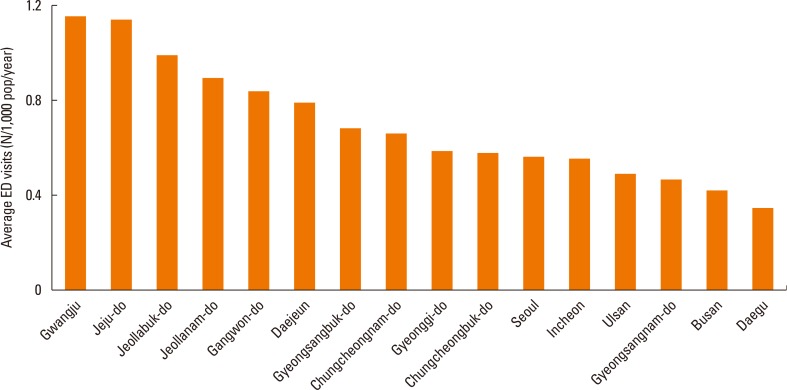
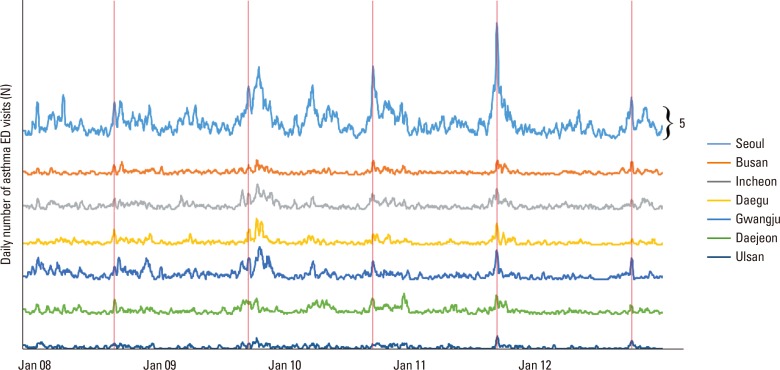
There were 157,559 events of AE (0.62 events/1,000 individuals/year) during the study period. There were spring and fall peaks of AE in children and adults, but only 1 winter peak in the elderly. The amplitude of the AE peak in infants was higher in spring than in fall (9.16 vs 3.04, P < 0.010), and the fall peak was approximately 1 month later in infants than in school children (October 11 vs November 13, P < 0.010). The association between AE and rhinovirus was greatest in school children (rho=0.331), and the association between AE and influenza virus was greatest in those aged ≥60 years (rho=0.682).
CONCLUSIONS
The rhythmicity, amplitude, and phase of the annual cycle of AE differed among different age groups. The patterns of AE were related to the annual rhino- and influenza virus epidemics.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Hospitalization Due to Asthma Exacerbation: A China Asthma Research Network (CARN) Retrospective Study in 29 Provinces Across Mainland China
Jiangtao Lin, Bin Xing, Huaping Tang, Lan Yang, Yadong Yuan, Yuhai Gu, Ping Chen, Xiaoju Liu, Jie Zhang, Huiguo Liu, Changzheng Wang, Wei Zhou, Dejun Sun, Yiqiang Chen, Zhuochang Chen, Mao Huang, Qichang Lin, Chengping Hu, Xiaohong Yang, Jianmin Huo, Xianwei Ye, Xin Zhou, Ping Jiang, Wei Zhang, Yijiang Huang, Luming Dai, Rongyu Liu, Shaoxi Cai, Jianying Xu, Jianying Zhou,
Allergy Asthma Immunol Res. 2020;12(3):485-495. doi: 10.4168/aair.2020.12.3.485.
Reference
-
1. Reddel HK, Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009; 180:59–99. PMID: 19535666.2. Szefler SJ, Chmiel JF, Fitzpatrick AM, Giacoia G, Green TP, Jackson DJ, et al. Reply: to PMID 24290281. J Allergy Clin Immunol. 2014; 133:1776–1777.3. Larsen K, Zhu J, Feldman LY, Simatovic J, Dell S, Gershon AS, et al. The annual September peak in asthma exacerbation rates. Still a reality? Ann Am Thorac Soc. 2016; 13:231–239. PMID: 26636481.
Article4. Johnston NW, Sears MR. Asthma exacerbations. 1: epidemiology. Thorax. 2006; 61:722–728. PMID: 16877691.5. Cohen HA, Blau H, Hoshen M, Batat E, Balicer RD. Seasonality of asthma: a retrospective population study. Pediatrics. 2014; 133:e923–e932. PMID: 24616356.
Article6. Khetsuriani N, Kazerouni NN, Erdman DD, Lu X, Redd SC, Anderson LJ, et al. Prevalence of viral respiratory tract infections in children with asthma. J Allergy Clin Immunol. 2007; 119:314–321. PMID: 17140648.
Article7. Laor A, Cohen L, Danon YL. Effects of time, sex, ethnic origin, and area of residence on prevalence of asthma in Israeli adolescents. BMJ. 1993; 307:841–844. PMID: 8401126.
Article8. Song DJ. Rhinovirus and childhood asthma: an update. Korean J Pediatr. 2016; 59:432–439. PMID: 27895690.
Article9. Toivonen L, Schuez-Havupalo L, Karppinen S, Teros-Jaakkola T, Rulli M, Mertsola J, et al. Rhinovirus infections in the first 2 years of life. Pediatrics. 2016; 138:e20161309. PMID: 27581858.
Article10. Nicholson KG, Kent J, Ireland DC. Respiratory viruses and exacerbations of asthma in adults. BMJ. 1993; 307:982–986. PMID: 8241910.
Article11. Kim L, Kim JA, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health. 2014; 36:e2014008. PMID: 25078381.
Article12. Sanders DL, Gregg W, Aronsky D. Identifying asthma exacerbations in a pediatric emergency department: a feasibility study. Int J Med Inform. 2007; 76:557–564. PMID: 16647876.
Article13. Cornelissen G. Cosinor-based rhythmometry. Theor Biol Med Model. 2014; 11:16. PMID: 24725531.
Article14. Refinetti R, Lissen GC, Halberg F. Procedures for numerical analysis of circadian rhythms. Biol Rhythm Res. 2007; 38:275–325. PMID: 23710111.
Article15. Park HS, Choi GS, Cho JS, Kim YY. Epidemiology and current status of allergic rhinitis, asthma, and associated allergic diseases in Korea: ARIA Asia-Pacific workshop report. Asian Pac J Allergy Immunol. 2009; 27:167–171. PMID: 19839504.16. Won YK, Hwang TH, Roh EJ, Chung EH. Seasonal patterns of asthma in children and adolescents presenting at emergency departments in Korea. Allergy Asthma Immunol Res. 2016; 8:223–229. PMID: 26922932.
Article17. Teach SJ, Gergen PJ, Szefler SJ, Mitchell HE, Calatroni A, Wildfire J, et al. Seasonal risk factors for asthma exacerbations among inner-city children. J Allergy Clin Immunol. 2015; 135:1465–1473.e5. PMID: 25794658.
Article18. Eggo RM, Scott JG, Galvani AP, Meyers LA. Respiratory virus transmission dynamics determine timing of asthma exacerbation peaks: evidence from a population-level model. Proc Natl Acad Sci U S A. 2016; 113:2194–2199. PMID: 26858436.
Article19. Harju T, Keistinen T, Tuuponen T, Kivelä SL. Seasonal variation in childhood asthma hospitalisations in Finland, 1972-1992. Eur J Pediatr. 1997; 156:436–439. PMID: 9208236.
Article20. Kim JH, Choi JY, Kim NY, Kim JW, Baek JH, Baek HS, et al. Clinical risk factors associated with the development of wheezing in children less than 2 years of age who required hospitalization for viral lower respiratory tract infections. Korean J Pediatr. 2015; 58:245–250. PMID: 26300938.
Article21. Rossi GA, Colin AA. Infantile respiratory syncytial virus and human rhinovirus infections: respective role in inception and persistence of wheezing. Eur Respir J. 2015; 45:774–789. PMID: 25359340.
Article22. Zheng XY, Ding H, Jiang LN, Chen SW, Zheng JP, Qiu M, et al. Association between air pollutants and asthma emergency room visits and hospital admissions in time series studies: a systematic review and meta-analysis. PLoS One. 2015; 10:e0138146. PMID: 26382947.
Article23. Keegan AD, Shirey KA, Bagdure D, Blanco J, Viscardi RM, Vogel SN. Enhanced allergic responsiveness after early childhood infection with respiratory viruses: are long-lived alternatively activated macrophages the missing link? Pathog Dis. 2016; 74:ftw047. PMID: 27178560.
Article24. Nakamura T, Hashizume M, Ueda K, Shimizu A, Takeuchi A, Kubo T, et al. Asian dust and pediatric emergency department visits due to bronchial asthma and respiratory diseases in Nagasaki, Japan. J Epidemiol. 2016; 26:593–601. PMID: 27180931.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Seasonal Cycle and Relationship of Seasonal Rhino- and Influenza Virus Epidemics With Episodes of Asthma Exacerbation in Different Age Groups
- Seasonality of asthma exacerbation in children caused by respiratory virus infection and allergen sensitization
- Variations in Number of Hospitalized Patients with Cardiopulmonary Diseases Associated with 2009 H1N1 Pandemic Influenza in a Tertiary Teaching Hospital - Comparison with Seasonal Influenza
- Influenza
- Application of the Time Derivative (TD) Method for Early Alert of Influenza Epidemics