Korean J Pain.
2018 Oct;31(4):296-304. 10.3344/kjp.2018.31.4.296.
Complication of epiduroscopy: a brief review and case report
- Affiliations
-
- 1Unit of Pain Therapy, Salvatore Maugeri Foundation, Scientific Institute of Pavia, Pavia, Italy. marchesinidoc@gmail.com
- 2Anaesthesia, Intensive Care and Pain Therapy Service, Azienda Ospedaliera Universitaria Parma Hospital, Parma, Italy.
- 3Department of Surgical Sciences, Azienda Ospedaliera Universitaria Parma Hospital, University of Parma, Parma, Italy.
- KMID: 2421521
- DOI: http://doi.org/10.3344/kjp.2018.31.4.296
Abstract
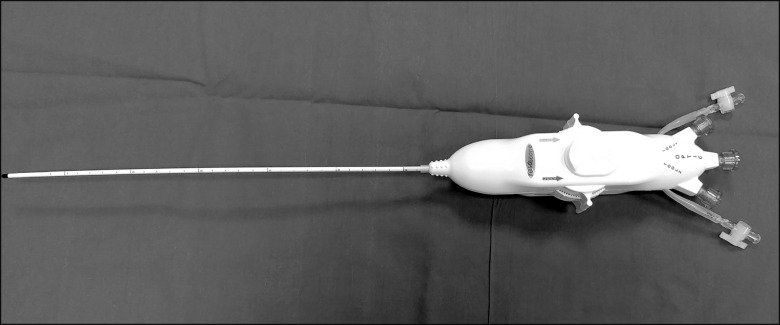
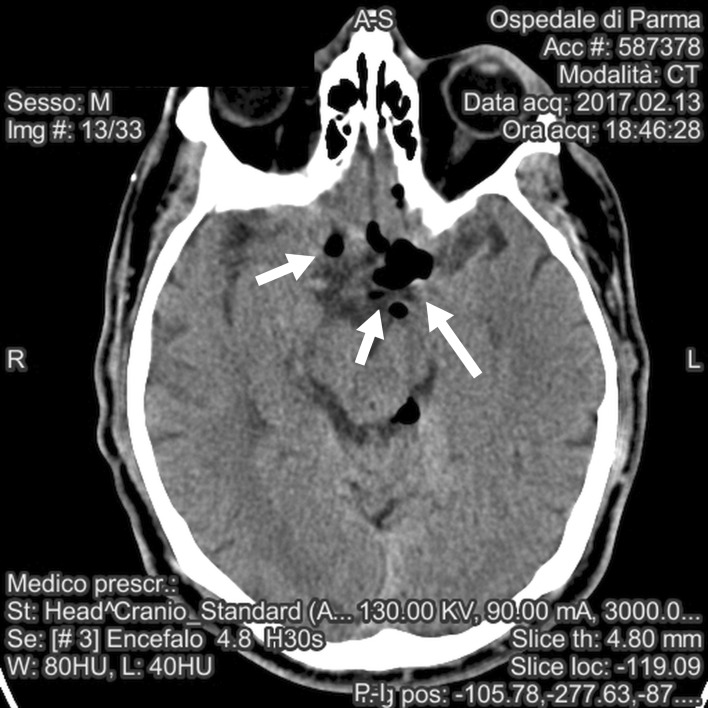
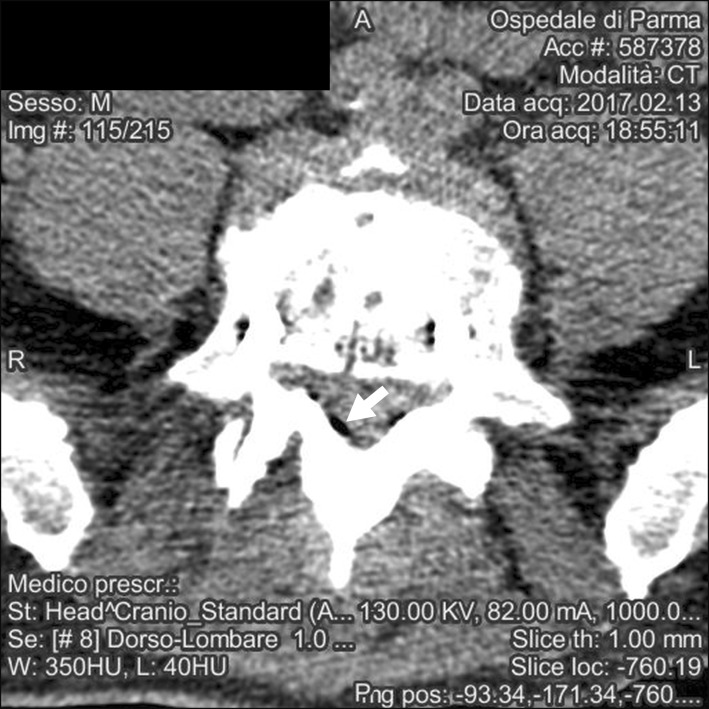
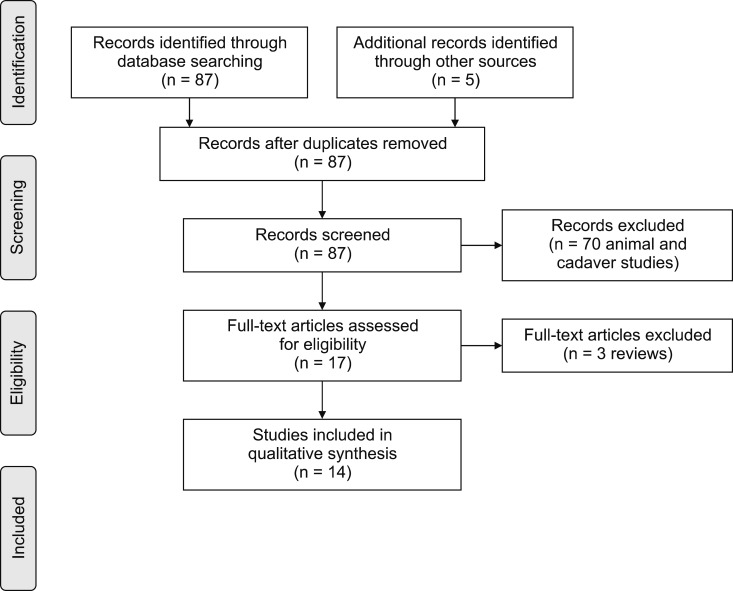
- Epiduroscopy is defined as a percutaneous, minimally invasive endoscopic investigation of the epidural space. Periduroscopy is currently used mainly as a diagnostic tool to directly visualize epidural adhesions in patients with failed back surgery syndrome (FBSS), and as a therapeutic action in patients with low back pain by accurately administering drugs, releasing inflammation, washing the epidural space, and mechanically releasing the scars displayed. Considering epiduroscopy a minimally invasive technique should not lead to underestimating its potential complications. The purpose of this review is to summarize and explain the mechanisms of the side effects strictly related to the technique itself, leaving aside complications considered typical for any kind of extradural procedure (e.g. adverse reactions due to the administration of drugs or bleeding) and not fitting the usual concept of epiduroscopy for which the data on its real usefulness are still lacking. The most frequent complications and side effects of epiduroscopy can be summarized as non-persistent post-procedural low back and/or leg discomfort/pain, transient neurological symptoms (headache, hearing impairment, paresthesia), dural puncture with or without post dural puncture headache (PDPH), post-procedural visual impairment with retinal hemorrhage, encephalopathy resulting in rhabdomyolysis due to a dural tear, intradural cyst, as well as neurogenic bladder and seizures. We also report for first time, to our knowledge, a case of symptomatic pneumocephalus after epiduroscopy, and try to explain the reason for this event and the precautions to avoid this complication.
Keyword
MeSH Terms
-
Brain Diseases
Cicatrix
Epidural Space
Failed Back Surgery Syndrome
Hearing Loss
Humans
Inflammation
Leg
Low Back Pain
Paresthesia
Pharmaceutical Preparations
Pneumocephalus
Post-Dural Puncture Headache
Punctures
Retinal Hemorrhage
Rhabdomyolysis
Seizures
Tears
Tissue Adhesions
Urinary Bladder, Neurogenic
Vision Disorders
Pharmaceutical Preparations
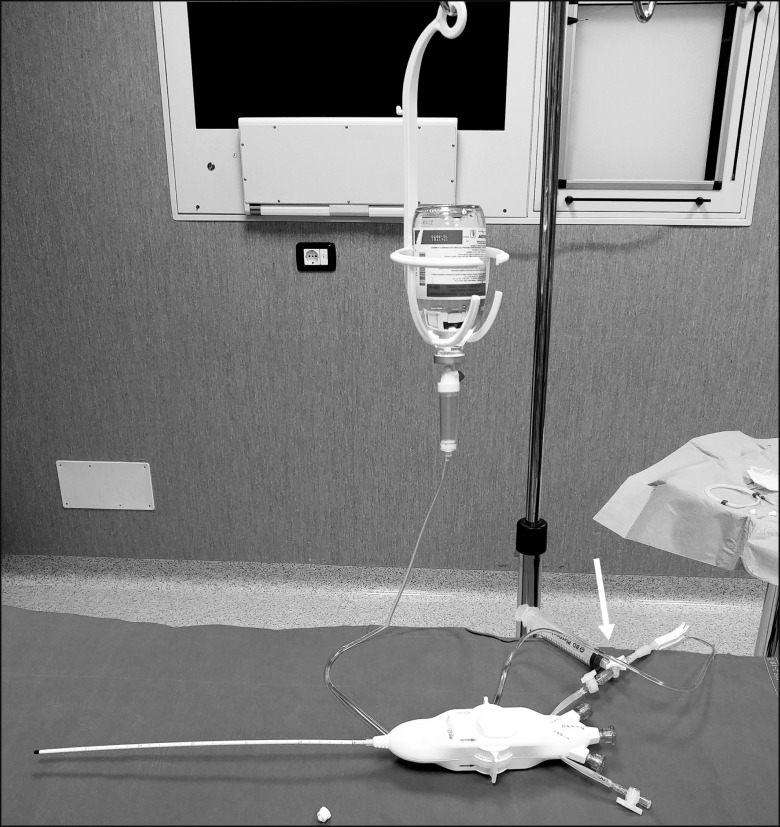
Figure
Reference
-
1. Burman MS. Myeloscopy or the direct visualization of the spinal canal and its contents. J Bone Joint Surg. 1931; 13:695–696.2. Shimoji K, Fujioka H, Onodera M, Hokari T, Fukuda S, Fujiwara N, et al. Observation of spinal canal and cisternae with the newly developed small-diameter, flexible fiberscopes. Anesthesiology. 1991; 75:341–344. PMID: 1859021.
Article3. Bosscher HA, Heavner JE. Incidence and severity of epidural fibrosis after back surgery: an endoscopic study. Pain Pract. 2010; 10:18–24. PMID: 19735365.
Article4. Avellanal M, Diaz-Reganon G. Interlaminar approach for epiduroscopy in patients with failed back surgery syndrome. Br J Anaesth. 2008; 101:244–249. PMID: 18552347.
Article5. Manchikanti L, Pampati V, Bakhit CE, Pakanati RR. Non-endoscopic and endoscopic adhesiolysis in post-lumbar laminectomy syndrome: a one-year outcome study and cost effectiveness analysis. Pain Physician. 1999; 2:52–58. PMID: 16906216.6. Amirikia A, Scott IU, Murray TG, Halperin LS. Acute bilateral visual loss associated with retinal hemorrhages following epiduroscopy. Arch Ophthalmol. 2000; 118:287–289. PMID: 10676802.7. Richardson J, McGurgan P, Cheema S, Prasad R, Gupta S. Spinal endoscopy in chronic low back pain with radiculopathy. A prospective case series. Anaesthesia. 2001; 56:454–460. PMID: 11350333.
Article8. Igarashi T, Hirabayashi Y, Seo N, Saitoh K, Fukuda H, Suzuki H. Lysis of adhesions and epidural injection of steroid/local anaesthetic during epiduroscopy potentially alleviate low back and leg pain in elderly patients with lumbar spinal stenosis. Br J Anaesth. 2004; 93:181–187. PMID: 15194631.
Article9. Dashfield AK, Taylor MB, Cleaver JS, Farrow D. Comparison of caudal steroid epidural with targeted steroid placement during spinal endoscopy for chronic sciatica: a prospective, randomized, double-blind trial. Br J Anaesth. 2005; 94:514–519. PMID: 15695544.
Article10. Mizuno J, Gauss T, Suzuki M, Hayashida M, Arita H, Hanaoka K. Encephalopathy and rhabdomyolysis induced by iotrolan during epiduroscopy. Can J Anaesth. 2007; 54:49–53. PMID: 17197468.
Article11. Heavner JE, Wyatt DE, Bosscher HA. Lumbosacral epiduroscopy complicated by intravascular injection. Anesthesiology. 2007; 107:347–350. PMID: 17667580.
Article12. Moschos MM, Rouvas A, Papaspirou A, Apostolopoulos M. Acute visual loss and intraocular hemorrhages associated with endoscopic spinal surgery. Clin Ophthalmol. 2008; 2:937–939. PMID: 19668448.
Article13. Justiz R, Taylor V, Day M. Neurogenic bladder: a complication after endoscopic adhesiolysis with return of bladder function while using nitrofurantoin. Anesth Analg. 2010; 110:1496–1498. PMID: 20304983.14. Ryu KS, Rathi NK, Kim G, Park CK. Iatrogenic intradural lumbosacral cyst following epiduroscopy. J Korean Neurosurg Soc. 2012; 52:491–494. PMID: 23323173.
Article15. Magalhães FN, Soares SC, Torres JM, Ungaretti A, Cacciacarro MF, Teixeira MJ, et al. Effects of ozone applied by spinal endoscopy in patients with chronic pain related to failed back surgery syndrome: a pilot study. Neuropsychiatr Dis Treat. 2013; 9:1759–1766. PMID: 24259984.16. Avellanal M, Diaz-Reganon G, Orts A, Soto S. One-year results of an algorithmic approach to managing failed back surgery syndrome. Pain Res Manag. 2014; 19:313–316. PMID: 25222573.
Article17. Beyaz SG. Seizures and transient neurological deficits during epiduroscopy in a patient with failed back surgery syndrome. Pain Med. 2015; 16:825–827. PMID: 25521450.
Article18. Gill JB, Heavner JE. Visual impairment following epidural fluid injections and epiduroscopy: a review. Pain Med. 2005; 6:367–374. PMID: 16266357.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fulminant Headache after Epiduroscopy
- The Effects of Epiduroscopy in Spinal Stenosis: A case report
- Iatrogenic Intradural Lumbosacral Cyst Following Epiduroscopy
- The Change of Cervical Epidural Pressure according to Infused Normal Saline in Epiduroscopy
- Severe Low Back Pain and Radiculopathy during Epiduroscopy