J Korean Orthop Assoc.
2017 Dec;52(6):543-551. 10.4055/jkoa.2017.52.6.543.
Subtalar Arthroereisis Using Kalix® Sinus Tarsi Implant for Pediatric Flexible Flatfoot
- Affiliations
-
- 1Department of Orthopedic Surgery, Konkuk University School of Medicine, Seoul, Korea. Jungfoot@hanmail.net
- 2Department of Orthopedic Surgery, Seoul Red Cross Hospital, Seoul, Korea.
- 3Department of Orthopedic Surgery, Myongji Hospital, Goyang, Korea.
- KMID: 2421348
- DOI: http://doi.org/10.4055/jkoa.2017.52.6.543
Abstract
- PURPOSE
The purpose of this study was to evaluate the radiographic and clinical outcomes of subtalar arthroereisis as a method of treatment for pediatric flexible flatfoot.
MATERIALS AND METHODS
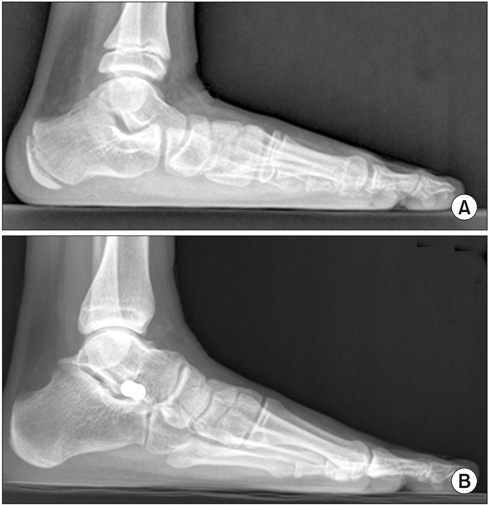
We retrospectively investigated 14 feet among 10 patients with flexible flatfoot, who were treated with a subtalar arthroereisis using a sinus tarsi implant between March 2007 and June 2012. Radiographically, the talo-1st metatarsal angle, talar declination, and calcaneal pitch angle have all been measured on lateral radiographs. The talo-navicular coverage angle and talo-1st metatarsal angle was measured on anteroposterior (AP) radiographs and tibio-calcaneal angle was assessed by hindfoot alignment view. Visual analogue scale (VAS) pain scores and the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot scores were used for clinical evaluation.
RESULTS
The mean follow-up was 48.7 months (16-98 months), and the mean age was 11.6 years (6-19 years). Radiographically, the mean pre-operative and postoperative values measured by the lateral foot radiograph were −25.1° and −7.5° for talo-1st metatarsal angle, 37.4° and 23.2° for talar declination, and 8.3° and 15.0° for calcaneal pitch angle, respectively. The mean preoperative and postoperative values measured by foot AP radiograph were 23.0° and 11.9° for talo-navicular coverage angle and 17.2° and 9.0° for talo-1st metatarsal angle, respectively. Moreover, tibio-calcaneal angle improved from valgus 17.4° on average to 4.5° on average. Clinically, the VAS score and AOFAS score was improved from 5.8 to 1.5 and from 61.8 to 90.4, respectively. Complication was sinus tarsi pain that occurred in 5 cases (35.7%).
CONCLUSION
We achieved a satisfactory correction of pediatric flexible flatfoot deformities via subtalar arthroereisis, using a sinus tarsi implant with favorable radiographic and clinical measures. However, high potential complication rate of postoperative sinus tarsi pain on weight-bearing should carefully be considered.
MeSH Terms
Figure
Reference
-
1. Cappello T, Song KM. Determining treatment of flatfeet in children. Curr Opin Pediatr. 1998; 10:77–81.2. Wenger DR, Leach J. Foot deformities in infants and children. Pediatr Clin North Am. 1986; 33:1411–1427.3. Sheikh Taha AM, Feldman DS. Painful flexible flatfoot. Foot Ankle Clin. 2015; 20:693–704.4. Bouchard M, Mosca VS. Flatfoot deformity in children and adolescents: surgical indications and management. J Am Acad Orthop Surg. 2014; 22:623–632.5. Needleman RL. Current topic review: subtalar arthroereisis for the correction of flexible flatfoot. Foot Ankle Int. 2005; 26:336–346.6. Fernández de Retana P, Alvarez F, Viladot R. Subtalar arthroereisis in pediatric flatfoot reconstruction. Foot Ankle Clin. 2010; 15:323–335.7. Maxwell JR, Carro A, Sun C. Use of the Maxwell-Brancheau arthroereisis implant for the correction of posterior tibial tendon dysfunction. Clin Podiatr Med Surg. 1999; 16:479–489.8. Addante JB, Ioli JP, Chin MW. Silastic sphere arthroereisis for surgical treatment of flexible flatfoot: a preliminary report. J Foot Surg. 1982; 21:91–95.9. Nelson SC, Haycock DM, Little ER. Flexible flatfoot treatment with arthroereisis: radiographic improvement and child health survey analysis. J Foot Ankle Surg. 2004; 43:144–155.10. Scharer BM, Black BE, Sockrider N. Treatment of painful pediatric flatfoot with Maxwell-Brancheau subtalar arthroereisis implant a retrospective radiographic review. Foot Ankle Spec. 2010; 3:67–72.11. Brancheau SP, Walker KM, Northcutt DR. An analysis of outcomes after use of the Maxwell-Brancheau Arthroereisis implant. J Foot Ankle Surg. 2012; 51:3–8.12. Chambers EF. An operation for the correction of flexible flat feet of adolescents. West J Surg Obstet Gynecol. 1946; 54:77–86.13. LeLièvre J. Current concepts and correction in the valgus foot. Clin Orthop Relat Res. 1970; 70:43–55.14. Subotnick SI. The subtalar joint lateral extra-articular arthroereisis: a preliminary report. J Am Podiatry Assoc. 1974; 64:701–711.15. Smith SD, Millar EA. Arthrorisis by means of a subtalar polyethylene peg implant for correction of hindfoot pronation in children. Clin Orthop Relat Res. 1983; 181:15–23.16. Arangio GA, Reinert KL, Salathe EP. A biomechanical model of the effect of subtalar arthroereisis on the adult flexible flat foot. Clin Biomech (Bristol, Avon). 2004; 19:847–852.17. Gutiérrez PR, Lara MH. Giannini prosthesis for flatfoot. Foot Ankle Int. 2005; 26:918–926.18. Forg P, Feldman K, Flake E, Green DR. Flake-Austin modification of the STA-Peg arthroereisis: a retrospective study. J Am Podiatr Med Assoc. 2001; 91:394–405.19. Ozan F, Doğar F, Gençer K, et al. Symptomatic flexible flatfoot in adults: subtalar arthroereisis. Ther Clin Risk Manag. 2015; 11:1597–1602.20. Lee KT, Kim JS, Young KW, Kim JY, Choi JH. The results of subtalar arthroereisis for flexible flatfoot of children. J Korean Foot Ankle Soc. 2006; 10:218–222.21. Moon JS, Bae WH, Seo JG, Lee WC. Clinical results of the subtalar arthroereisis for the flat foot. J Korean Foot Ankle Soc. 2008; 12:117–121.22. Viladot R, Pons M, Alvarez F, Omaña J. Subtalar arthroereisis for posterior tibial tendon dysfunction: a preliminary report. Foot Ankle Int. 2003; 24:600–606.23. Needleman RL. A surgical approach for flexible flatfeet in adults including a subtalar arthroereisis with the MBA sinus tarsi implant. Foot Ankle Int. 2006; 27:9–18.24. Jay RM, Din N. Correcting pediatric flatfoot with subtalar arthroereisis and gastrocnemius recession: a retrospective study. Foot Ankle Spec. 2013; 6:101–107.25. van Ooij B, Vos CJ, Saouti R. Arthroereisis of the subtalar joint: an uncommon complication and literature review. J Foot Ankle Surg. 2012; 51:114–117.26. Giannini BS, Ceccarelli F, Benedetti MG, Catani F, Faldini C. Surgical treatment of flexible flatfoot in children a four-year follow-up study. J Bone Joint Surg Am. 2001; 83:Suppl 2 Pt 2. 73–79.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adult Idiopathic Flexible Flat Foot Treated with Medial Sliding Calcaneal Osteotomy and Subtalar Arthroereisis: Report of 1 Case
- The Treatment of Failed Kidner Procedure for Adolescent Prehallux: A Case Report
- The Results of Subtalar Arthroereisis for Flexible Flatfoot of Children
- Clinical Results of the Subtalar Arthroereisis for the Flat Foot
- Management of Flexible Flatfoot in Chidren and Adolescent