Korean J Gastroenterol.
2018 Sep;72(3):155-158. 10.4166/kjg.2018.72.3.155.
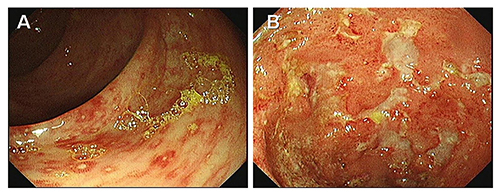
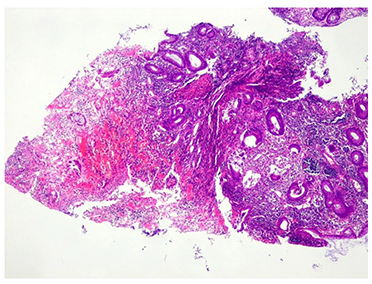
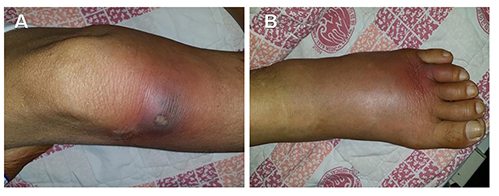
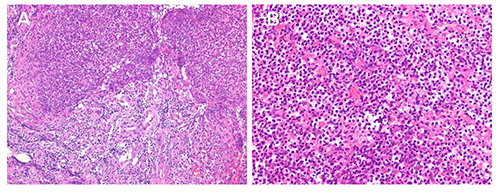
Multiple Pyoderma Gangrenosum in Ulcerative Colitis
- Affiliations
-
- 1Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea. dr9696@nate.com
- KMID: 2420755
- DOI: http://doi.org/10.4166/kjg.2018.72.3.155
Abstract
- No abstract available.
Figure
Reference
-
1. Lee JI, Park HJ, Lee JY, Cho BK. A case of pyoderma gangrenosum with ulcerative colitis treated with mesalazine. Ann Dermatol. 2010; 22:422–425.
Article2. Binus AM, Qureshi AA, Li VW, Winterfield LS. Pyoderma gangrenosum: a retrospective review of patient characteristics, comorbidities and therapy in 103 patients. Br J Dermatol. 2011; 165:1244–1250.
Article3. Powell FC, Su WP, Perry HO. Pyoderma gangrenosum: classification and management. J Am Acad Dermatol. 1996; 34:395–409. quiz 410-412.
Article4. Mlika RB, Riahi I, Fenniche S, et al. Pyoderma gangrenosum: a report of 21 cases. Int J Dermatol. 2002; 41:65–68.
Article5. Greuter T, Navarini A, Vavricka SR. Skin manifestations of inflammatory bowel disease. Clin Rev Allergy Immunol. 2017; 53:413–427.
Article6. Ahn C, Negus D, Huang W. Pyoderma gangrenosum: a review of pathogenesis and treatment. Expert Rev Clin Immunol. 2018; 14:225–233.
Article7. Byeon YM, Lee J, Lee SJ, et al. Peritonsillar involvement in pyoderma gangrenosum associated with ulcerative colitis. Intest Res. 2014; 12:153–156.
Article8. Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015; 21:1982–1992.
Article9. Herberger K, Dissemond J, Hohaus K, Schaller J, Anastasiadou Z, Augustin M. Treatment of pyoderma gangrenosum: retrospective multicentre analysis of 121 patients. Br J Dermatol. 2016; 175:1070–1072.
Article10. Ormerod AD, Thomas KS, Craig FE, et al. Comparison of the two most commonly used treatments for pyoderma gangrenosum: results of the STOP GAP randomised controlled trial. BMJ. 2015; 350:h2958.
Article11. Brooklyn TN, Dunnill MG, Shetty A, et al. Infliximab for the treatment of pyoderma gangrenosum: a randomised, double blind, placebo controlled trial. Gut. 2006; 55:505–509.
Article12. Al Rajabi W, Venturini M, Sala R, Calzavara-Pinton P. Wegener's granulomatosis of the penis: genital presentation of systemic disease. Dermatology. 2006; 212:370–372.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Post-traumatic Pyoderma Gangrenosum Associated with Ulcerative Colitis
- A Case of Pyoderma Gangrenosum Associated with Ulcerative Colitis
- A Case of Simultaneous Presentation of Bullous and Ulcerative Types of Pyoderma Gangrenosum in an Ulcerative Colitis Patient
- Pyoderma Gangrenosum in a Patient with Ulcerative Colitis: A Case Report
- A Case of Multiple Bullous Pyoderma Gangrenosum Lesions on the Face of a Patient with Ulcerative Colitis