Tuberc Respir Dis.
2018 Apr;81(2):156-162. 10.4046/trd.2017.0039.
Peripheral Eosinophilia and Clinico-radiological Characteristics among Health Screening Program Recipients
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea. jykimmd@cau.ac.kr
- KMID: 2420604
- DOI: http://doi.org/10.4046/trd.2017.0039
Abstract
- BACKGROUND
Eosinophilia is well recognized in specific conditions. The objective of the present study was to determine clinico-radiologic characteristics of eosinophilia and changes in prevalence over 10 years in recipients of private health screening program at a tertiary hospital in Korea.
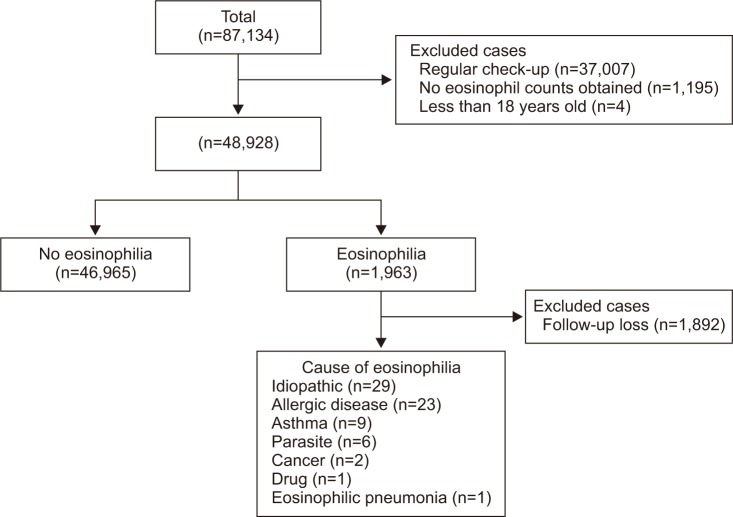
METHODS
Data of private health screening program recipients at the health promotion center of Chung-Ang University Hospital from 2004 to 2013 were collected. Health-related questionnaires and laboratory findings of private health screening program with possible relation with eosinophilia were reviewed. Results of enzyme-linked immunosorbent assay (ELISA) for parasite, chest computed tomography, and pulmonary function test were also reviewed.
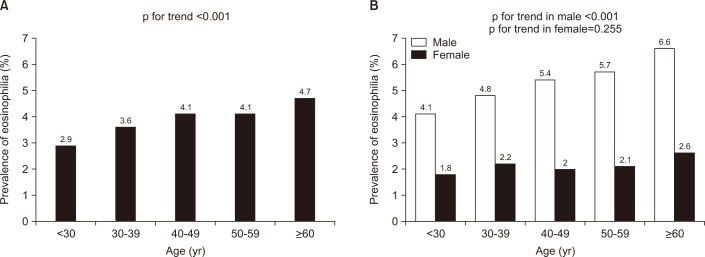
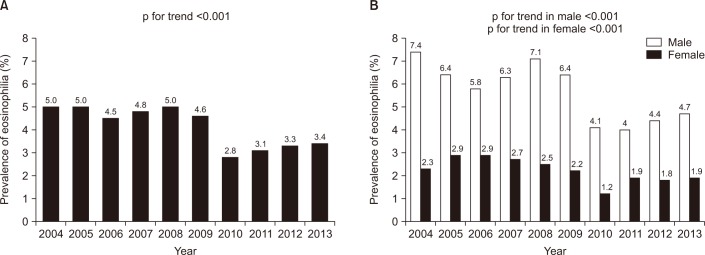
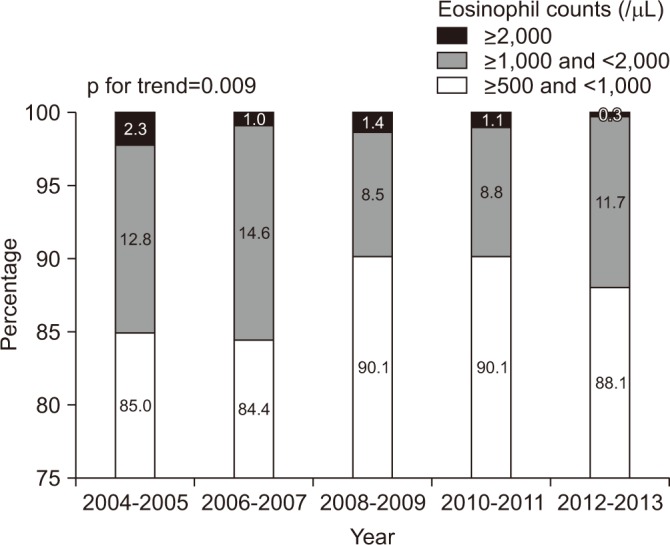
RESULTS
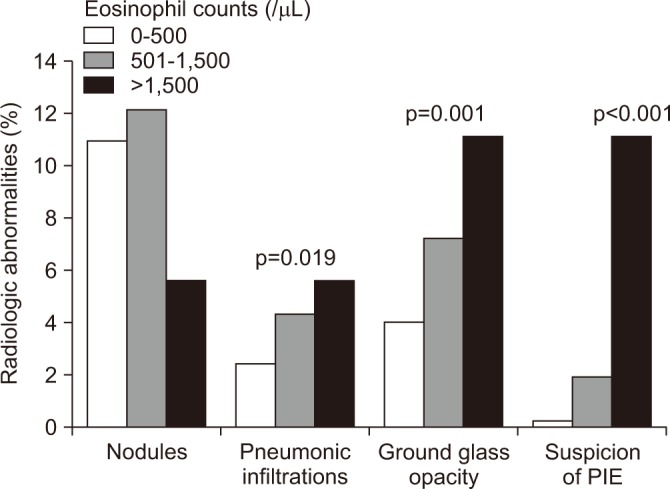
The cumulative prevalence of eosinophilia was 4.0% (1,963 of 48,928). Prevalence of eosinophilia showed a decreased trend from 2004 to 2013. Most cases (96.6%) had mild degree of eosinophilia. Eosinophilic subjects were older and male-predominant. They showed lower levels of forced expiratory volume in 1 second (FEVâ‚%), forced vital capacity (FVC%), and FEVâ‚/FVC than those without eosinophilia. Eosinophilic subjects showed higher positive rate for common parasite in ELISA than those without eosinophilia. On radiologic findings, consolidation and ground glass opacities were positively associated with the degree of eosinophilia. When eosinophil was classified based on severity, statistically significant correlation between the severity of eosinophil and radiologic abnormalities was found.
CONCLUSION
Eosinophilia is uncommon in healthy population. It usually occurs at a mild degree. Eosinophilic patients have more radiologic abnormalities compared to those without eosinophilia. Such radiologic abnormalities are associated with the severity of eosinophilia.
Keyword
MeSH Terms
Figure
Reference
-
1. Tefferi A. Blood eosinophilia: a new paradigm in disease classification, diagnosis, and treatment. Mayo Clin Proc. 2005; 80:75–83. PMID: 15667033.
Article2. Helbig G. Advances in the diagnosis and treatment of eosinophilia. Curr Opin Hematol. 2014; 21:3–7. PMID: 24322486.
Article3. Crane MM, Chang CM, Kobayashi MG, Weller PF. Incidence of myeloproliferative hypereosinophilic syndrome in the United States and an estimate of all hypereosinophilic syndrome incidence. J Allergy Clin Immunol. 2010; 126:179–181. PMID: 20639012.
Article4. Mejia R, Nutman TB. Evaluation and differential diagnosis of marked, persistent eosinophilia. Semin Hematol. 2012; 49:149–159. PMID: 22449625.
Article5. Dulohery MM, Patel RR, Schneider F, Ryu JH. Lung involvement in hypereosinophilic syndromes. Respir Med. 2011; 105:114–121. PMID: 21036585.
Article6. Sluzevich JC, Sheth AP, Lucky AW. Persistent eosinophilia as a presenting sign of scabies in patients with disorders of keratinization. Arch Dermatol. 2007; 143:670–673.
Article7. Schleich FN, Chevremont A, Paulus V, Henket M, Manise M, Seidel L, et al. Importance of concomitant local and systemic eosinophilia in uncontrolled asthma. Eur Respir J. 2014; 44:97–108. PMID: 24525441.
Article8. Vu Thi N, Pozio E, Van De N, Praet N, Pezzotti P, Gabriel S, et al. Anti-Trichinella IgG in ethnic minorities living in Trichinella-endemic areas in northwest Vietnam: study of the predictive value of selected clinical signs and symptoms for the diagnosis of trichinellosis. Acta Trop. 2014; 139:93–98. PMID: 25076109.9. Naldi L, Crotti S. Epidemiology of cutaneous drug-induced reactions. G Ital Dermatol Venereol. 2014; 149:207–218. PMID: 24819642.10. Hogan SP, Rosenberg HF, Moqbel R, Phipps S, Foster PS, Lacy P, et al. Eosinophils: biological properties and role in health and disease. Clin Exp Allergy. 2008; 38:709–750. PMID: 18384431.
Article11. Gotlib J. World Health Organization-defined eosinophilic disorders: 2011 update on diagnosis, risk stratification, and management. Am J Hematol. 2011; 86:677–688. PMID: 21761433.
Article12. Kauffmann F, Neukirch F, Korobaeff M, Marne MJ, Claude JR, Lellouch J. Eosinophils, smoking, and lung function: an epidemiologic survey among 912 working men. Am Rev Respir Dis. 1986; 134:1172–1175. PMID: 3491554.13. Kim HS, Jin Y, Choi MH, Kim JH, Lee YH, Yoon CH, et al. Significance of serum antibody test for toxocariasis in healthy healthcare examinees with eosinophilia in Seoul and Gyeongsangnam-do, Korea. J Korean Med Sci. 2014; 29:1618–1625. PMID: 25469060.
Article14. Hong SJ, Lee MS, Sohn MH, Shim JY, Han YS, Park KS, et al. Self-reported prevalence and risk factors of asthma among Korean adolescents: 5-year follow-up study, 1995-2000. Clin Exp Allergy. 2004; 34:1556–1562. PMID: 15479270.
Article15. Kim YY. Past, present, and future of allergy in Korea. Allergy Asthma Immunol Res. 2010; 2:155–164. PMID: 20592913.
Article16. Hong ST, Chai JY, Choi MH, Huh S, Rim HJ, Lee SH. A successful experience of soil-transmitted helminth control in the Republic of Korea. Korean J Parasitol. 2006; 44:177–185. PMID: 16969055.
Article17. Mensinga TT, Schouten JP, Weiss ST, Van der Lende R. Relationship of skin test reactivity and eosinophilia to level of pulmonary function in a community-based population study. Am Rev Respir Dis. 1992; 146:638–643. PMID: 1519840.
Article18. Ulrik CS. Eosinophils and pulmonary function: an epidemiologic study of adolescents and young adults. Ann Allergy Asthma Immunol. 1998; 80:487–493. PMID: 9647272.
Article19. Katz LE, Gleich GJ, Hartley BF, Yancey SW, Ortega HG. Blood eosinophil count is a useful biomarker to identify patients with severe eosinophilic asthma. Ann Am Thorac Soc. 2014; 11:531–536. PMID: 24606022.
Article20. LifeLines Cohort Study. Amini M, Bashirova D, Prins BP, Corpeleijn E, Bruinenberg M, et al. Eosinophil count is a common factor for complex metabolic and pulmonary traits and diseases: the LifeLines Cohort Study. PLoS One. 2016; 11:e0168480. PMID: 27978545.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Affecting the Participation Rate in the Health Screening Program of Medical Insurance
- National Health Screening Program of Korea
- Peripheral Blood Eosinophilia: An Unusual Presentation of Bone Marrow Involvement in a Patient with Relapsed Thyroid Papillary Carcinoma
- Two Cases of Apathetic Hyperthyroidism associated with Peripheral Eosinophilia
- Regional Variation in National Gastric Cancer Screening Rate in Korea