Tuberc Respir Dis.
2018 Apr;81(2):99-105. 10.4046/trd.2017.0094.
What Can We Apply to Manage Acute Exacerbation of Chronic Obstructive Pulmonary Disease with Acute Respiratory Failure?
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea. kimdkmd@gmail.com
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea.
- KMID: 2420597
- DOI: http://doi.org/10.4046/trd.2017.0094
Abstract
- Acute exacerbation(s) of chronic obstructive pulmonary disease (AECOPD) tend to be critical and debilitating events leading to poorer outcomes in relation to chronic obstructive pulmonary disease (COPD) treatment modalities, and contribute to a higher and earlier mortality rate in COPD patients. Besides pro-active preventative measures intended to obviate acquisition of AECOPD, early recovery from severe AECOPD is an important issue in determining the long-term prognosis of patients diagnosed with COPD. Updated GOLD guidelines and recently published American Thoracic Society/European Respiratory Society clinical recommendations emphasize the importance of use of pharmacologic treatment including bronchodilators, systemic steroids and/or antibiotics. As a non-pharmacologic strategy to combat the effects of AECOPD, noninvasive ventilation (NIV) is recommended as the treatment of choice as this therapy is thought to be most effective in reducing intubation risk in patients diagnosed with AECOPD with acute respiratory failure. Recently, a few adjunctive modalities, including NIV with helmet and helium-oxygen mixture, have been tried in cases of AECOPD with respiratory failure. As yet, insufficient documentation exists to permit recommendation of this therapy without qualification. Although there are too few findings, as yet, to allow for regular andr routine application of those modalities in AECOPD, there is anecdotal evidence to indicate both mechanical and physiological benefits connected with this therapy. High-flow nasal cannula oxygen therapy is another supportive strategy which serves to improve the symptoms of hypoxic respiratory failure. The therapy also produced improvement in ventilatory variables, and it may be successfully applied in cases of hypercapnic respiratory failure. Extracorporeal carbon dioxide removal has been successfully attempted in cases of adult respiratory distress syndrome, with protective hypercapnic ventilatory strategy. Nowadays, it is reported that it was also effective in reducing intubation in AECOPD with hypercapnic respiratory failure. Despite the apparent need for more supporting evidence, efforts to improve efficacy of NIV have continued unabated. It is anticipated that these efforts will, over time, serve toprogressively decrease the risk of intubation and invasive mechanical ventilation in cases of AECOPD with acute respiratory failure.
Keyword
MeSH Terms
-
Anti-Bacterial Agents
Bronchodilator Agents
Carbon Dioxide
Catheters
Head Protective Devices
Humans
Intubation
Mortality
Noninvasive Ventilation
Oxygen
Oxygen Inhalation Therapy
Prognosis
Pulmonary Disease, Chronic Obstructive*
Respiration, Artificial
Respiratory Distress Syndrome, Adult
Respiratory Insufficiency*
Steroids
Anti-Bacterial Agents
Bronchodilator Agents
Carbon Dioxide
Oxygen
Steroids
Figure
Reference
-
1. European Respiratory Society. European Respiratory Society's white book. Sheffield: European Respiratory Society;2016.2. Yoon HK, Park YB, Rhee CK, Lee JH, Oh YM. Committee of the Korean COPD Guideline 2014. Summary of the chronic obstructive pulmonary disease clinical practice guideline revised in 2014 by the Korean Academy of Tuberculosis and Respiratory Disease. Tuberc Respir Dis. 2017; 80:230–240.
Article3. Singh D. Pharmacological treatment for COPD; GOLD 2017 changes direction. Br J Clin Pharmacol. 2017; 83:935–937.
Article4. Zhou A, Zhou Z, Zhao Y, Chen P. The recent advances of phenotypes in acute exacerbations of COPD. Int J Chron Obstruct Pulmon Dis. 2017; 12:1009–1018.
Article5. Hillas G, Perlikos F, Tzanakis N. Acute exacerbation of COPD: is it the “stroke of the lungs”? Int J Chron Obstruct Pulmon Dis. 2016; 11:1579–1586.6. Ko FW, Chan KP, Hui DS, Goddard JR, Shaw JG, Reid DW, et al. Acute exacerbation of COPD. Respirology. 2016; 21:1152–1165.
Article7. Donaldson GC, Law M, Kowlessar B, Singh R, Brill SE, Allinson JP, et al. Impact of prolonged exacerbation recovery in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015; 192:943–950.
Article8. Wedzicha JA, Miravitlles M, Hurst JR, Calverley PM, Albert RK, Anzueto A, et al. Management of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J. 2017; 49:1600791.9. Mazhar SH, Ismail NE, Newton DA, Chrystyn H. Relative lung deposition of salbutamol following inhalation from a spacer and a Sidestream jet nebulizer following an acute exacerbation. Br J Clin Pharmacol. 2008; 65:334–337.
Article10. Bafadhel M, McKenna S, Terry S, Mistry V, Pancholi M, Venge P, et al. Blood eosinophils to direct corticosteroid treatment of exacerbations of chronic obstructive pulmonary disease: a randomized placebo-controlled trial. Am J Respir Crit Care Med. 2012; 186:48–55.11. Austin MA, Wills KE, Blizzard L, Walters EH, Wood-Baker R. Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial. BMJ. 2010; 341:c5462.
Article12. Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Arch Bronconeumol. 2017; 53:128–149.
Article13. Seol YM, Park YE, Kim SR, Lee JH, Lee SJ, Kim KU, et al. Application of noninvasive positive pressure ventilation in patients with respiratory failure. Tuberc Respir Dis. 2006; 61:26–33.
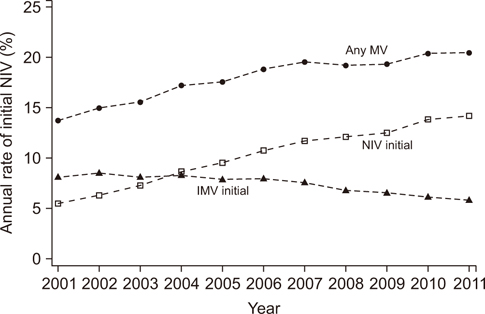
Article14. Stefan MS, Shieh MS, Pekow PS, Hill N, Rothberg MB, Lindenauer PK. Trends in mechanical ventilation among patients hospitalized with acute exacerbations of COPD in the United States, 2001 to 2011. Chest. 2015; 147:959–968.
Article15. Osadnik CR, Tee VS, Carson-Chahhoud KV, Picot J, Wedzicha JA, Smith BJ. Non-invasive ventilation for the management of acute hypercapnic respiratory failure due to exacerbation of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2017; 7:CD004104.
Article16. Esquinas Rodriguez AM, Papadakos PJ, Carron M, Cosentini R, Chiumello D. Clinical review: helmet and non-invasive mechanical ventilation in critically ill patients. Crit Care. 2013; 17:223.
Article17. Liu Q, Gao Y, Chen R, Cheng Z. Noninvasive ventilation with helmet versus control strategy in patients with acute respiratory failure: a systematic review and meta-analysis of controlled studies. Crit Care. 2016; 20:265.
Article18. Patel BK, Wolfe KS, Pohlman AS, Hall JB, Kress JP. Effect of noninvasive ventilation delivered by helmet vs face mask on the rate of endotracheal intubation in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2016; 315:2435–2441.19. Ozlem CG, Ali A, Fatma U, Mehtap T, Saziye S. Comparison of helmet and facial mask during noninvasive ventilation in patients with acute exacerbation of chronic obstructive pulmonary disease: a randomized controlled study. Turk J Med Sci. 2015; 45:600–606.20. Pisani L, Mega C, Vaschetto R, Bellone A, Scala R, Cosentini R, et al. Oronasal mask versus helmet in acute hypercapnic respiratory failure. Eur Respir J. 2015; 45:691–699.
Article21. Abroug F, Ouanes-Besbes L, Hammouda Z, Benabidallah S, Dachraoui F, Ouanes I, et al. Noninvasive ventilation with helium-oxygen mixture in hypercapnic COPD exacerbation: aggregate meta-analysis of randomized controlled trials. Ann Intensive Care. 2017; 7:59.
Article22. Jolliet P, Ouanes-Besbes L, Abroug F, Ben Khelil J, Besbes M, Garnero A, et al. A multicenter randomized trial assessing the efficacy of helium/oxygen in severe exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017; 195:871–880.
Article23. Bhatt N, Osborn E. Extracorporeal gas exchange: the expanding role of extracorporeal support in respiratory failure. Clin Chest Med. 2016; 37:765–780.24. Kluge S, Braune SA, Engel M, Nierhaus A, Frings D, Ebelt H, et al. Avoiding invasive mechanical ventilation by extracorporeal carbon dioxide removal in patients failing noninvasive ventilation. Intensive Care Med. 2012; 38:1632–1639.
Article25. Del Sorbo L, Pisani L, Filippini C, Fanelli V, Fasano L, Terragni P, et al. Extracorporeal CO2 removal in hypercapnic patients at risk of noninvasive ventilation failure: a matched cohort study with historical control. Crit Care Med. 2015; 43:120–127.26. Braune S, Sieweke A, Brettner F, Staudinger T, Joannidis M, Verbrugge S, et al. The feasibility and safety of extracorporeal carbon dioxide removal to avoid intubation in patients with COPD unresponsive to noninvasive ventilation for acute hypercapnic respiratory failure (ECLAIR study): multicentre case-control study. Intensive Care Med. 2016; 42:1437–1444.27. Del Sorbo L, Fan E, Nava S, Ranieri VM. ECCO2R in COPD exacerbation only for the right patients and with the right strategy. Intensive Care Med. 2016; 42:1830–1831.
Article28. Nishimura M. High-flow nasal cannula oxygen therapy in adults: physiological benefits, indication, clinical benefits, and adverse effects. Respir Care. 2016; 61:529–541.
Article29. Silva Santos P, Esquinas AM. The use of high-flow nasal oxygen in COPD patients. Int J Chron Obstruct Pulmon Dis. 2016; 11:2259–2260.
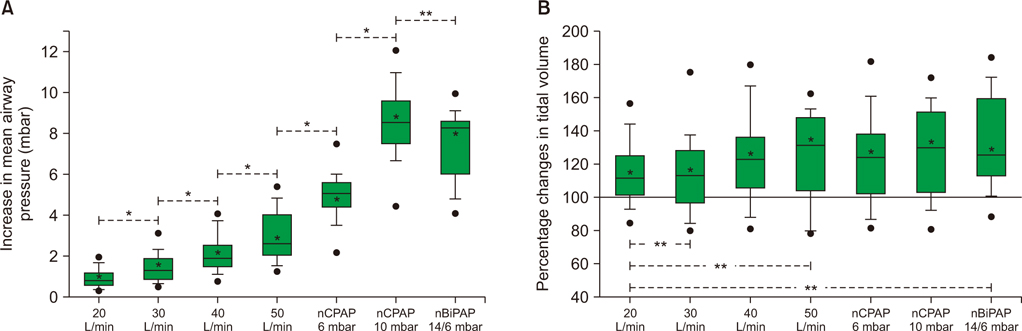
Article30. Braunlich J, Kohler M, Wirtz H. Nasal highflow improves ventilation in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2016; 11:1077–1085.31. Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015; 372:2185–2196.
Article32. Pilcher J, Eastlake L, Richards M, Power S, Cripps T, Bibby S, et al. Physiological effects of titrated oxygen via nasal high-flow cannulae in COPD exacerbations: a randomized controlled cross-over trial. Respirology. 2017; 22:1149–1155.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Study of Clarithromycin for the Treatment of Acute Exacerbation of Chronic Obstructive Pulmonary Disease
- Pulmonary Strongyloidiasis Masquerading as Exacerbation of Chronic Obstructive Pulmonary Disease
- Desaturaton due to Acute Exacerbation of Chronic Obstructive Pulmonary Disease in the Patient Who Underwent the Cephalic Vein Bypass Surgery under Epidural Anesthesia
- Successful noninvasive ventilation in a severely acidotic and hypercapnic comatose COVID-19 patient with multiple comorbidities: a case report
- Bacterial etiology of acute exacerbations of chronic obstructive pulmonary disease in hospitalized patients