Tuberc Respir Dis.
2018 Oct;81(4):281-288. 10.4046/trd.2017.0114.
The Comparison of Clinical Variables in Two Classifications: GOLD 2017 Combined Assessment and Spirometric Stage of Chronic Obstructive Pulmonary Disease
- Affiliations
-
- 1Ataturk Chest Diseases and Chest Surgery Education and Research Hospital, Pulmonary Rehabilitation and Home Care Center, Ankara, Turkey. ipekcayli@yahoo.com
- KMID: 2420561
- DOI: http://doi.org/10.4046/trd.2017.0114
Abstract
- BACKGROUND
There are limited number of studies that investigate clinical variables instead of chronic obstructive lung disease (COPD) management according to Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2017 classification. The aim of the study was to investigate whether there was a difference between GOLD 2017 classification and spirometric stage in clinical variables in patients with COPD. The data of 427 male patients with stable COPD were investigated retrospectively.
METHODS
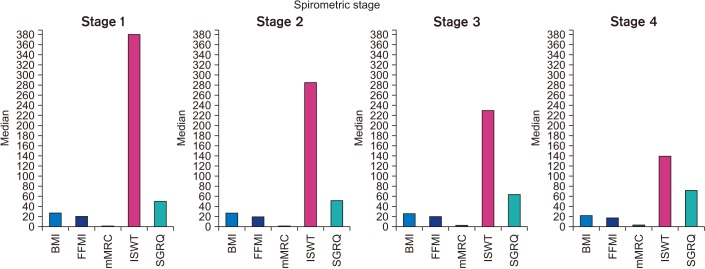
Patients were allocated into combined assessment of GOLD 2017 and spirometric stage. Age, amount of smoking, pulmonary function, modified Medical Research Council (mMRC), incremental shuttle walk test (ISWT), Hospital Anxiety-Depression Scale (HADS), St. George's Respiratory Questionnaire (SGRQ), body mass index (BMI), and fat free mass index (FFMI) were recorded.
RESULTS
Seventy-three (17%) patients were in group A, 103 (24%) constituted group B, 38 (9%) were included in group C, and 213 (50%) comprised group D according to the combined assessment of GOLD 2017. Twenty-three patients (5%) were in stage 1, 95 (22%) were in stage 2, 149 (35%) were in stage 3, and 160 (38%) were in stage 4 according to spirometric stage. According to GOLD 2017, age, amount of smoking, mMRC, BMI, FFMI, SGRQ, HADS, forced vital capacity, forced expiratory volume in 1 second (FEV1), and ISWT were significantly different between groups. Ages, amount of smoking, FFMI, BMI, HADS of group A were different from B and D. Smiliar values of FEV1 were found in A-C and B-D. A and C had smiliar ISWT. According to spirometric stage, BMI, FFMI of stage 4 were statistically different. mMRC, ISWT, and SGRQ of stages 3 and 4 were different from other stages, amongst themselves. FEV1 was correlated with mMRC, SGRQ, anxiety scores, BMI, FFMI, and ISWT.
CONCLUSION
This study showed that the GOLD ABCD classification might not represent the severity of COPD sufficiently well in terms of lung function or exercise capacity. The combination of both spirometric stage and combined assessment of GOLD 2017 is important, especially for estimating clinical variables.
MeSH Terms
Figure
Cited by 2 articles
-
Does the GOLD 2017 Classification Improve the Ability to Predict Exacerbation and Mortality?
Hun-Gyu Hwang
Tuberc Respir Dis. 2018;81(3):256-257. doi: 10.4046/trd.2018.0033.Old Friends, Old Wine, and Old COPD Classification Are Best
Chin Kook Rhee
Tuberc Respir Dis. 2018;81(4):347-348. doi: 10.4046/trd.2018.0071.
Reference
-
1. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management and prevention of chronic, obstructive pulmonary disease, 2017 report [Internet]. Global Initiative for Chronic Obstructive Lung Disease;2017. cited 2017 Dec 5. Available from: http://goldcopd.org.2. Rennard SI, Vestbo J. COPD: the dangerous underestimate of 15%. Lancet. 2006; 367:1216–1219. PMID: 16631861.
Article3. Soriano JB, Lamprecht B, Ramirez AS, Martinez-Camblor P, Kaiser B, Alfageme I, et al. Mortality prediction in chronic obstructive pulmonary disease comparing the GOLD 2007 and 2011 staging systems: a pooled analysis of individual patient data. Lancet Respir Med. 2015; 3:443–450. PMID: 25995071.
Article4. Goossens LM, Leimer I, Metzdorf N, Becker K, Rutten-van Molken MP. Does the 2013 GOLD classification improve the ability to predict lung function decline, exacerbations and mortality: a post-hoc analysis of the 4-year UPLIFT trial. BMC Pulm Med. 2014; 14:163. PMID: 25326750.
Article5. Kim J, Yoon HI, Oh YM, Lim SY, Lee JH, Kim TH, et al. Lung function decline rates according to GOLD group in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015; 10:1819–1827. PMID: 26379432.
Article6. Han MK, Muellerova H, Curran-Everett D, Dransfield MT, Washko GR, Regan EA, et al. GOLD 2011 disease severity classification in COPDGene: a prospective cohort study. Lancet Respir Med. 2013; 1:43–50. PMID: 24321803.
Article7. Fletcher CM. Standardised questionnaire on respiratory symptoms. Br Med J. 1960; 2:1665. PMID: 13688719.8. Singh SJ, Morgan MD, Scott S, Walters D, Hardman AE. Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax. 1992; 47:1019–1024. PMID: 1494764.
Article9. Aydemir O, Guvenir T, Kuey L, Kultur S. Validity and reliability of Turkish version of Hospital Anxiety and Depression Scale. Turk Psikiyatri Derg. 1997; 8:280–287.10. Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A selfcomplete measure of health status for chronic airflow limitation. The St. George's Respiratory Questionnaire. Am Rev Respir Dis. 1992; 145:1321–1327. PMID: 1595997.
Article11. Polatli M, Yorgancioglu A, Aydemir O, Yilmaz Demirci N, Kırkil G, Atis Nayci S, et al. St. George Solunum Anketinin Turkce gecerlilik ve guven ilirligi. Tuberkuloz Toraks. 2013; 61:81–87.12. Hurst JR, Vestbo J, Anzueto A, Locantore N, Mullerova H, Tal-Singer R, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010; 363:1128–1138. PMID: 20843247.
Article13. Anzueto A, Leimer I, Kesten S. Impact of frequency of COPD exacerbations on pulmonary function, health status and clinical outcomes. Int J Chron Obstruct Pulmon Dis. 2009; 4:245–251. PMID: 19657398.14. Kanner RE, Anthonisen NR, Connett JE. Lung Health Study Research Group. Lower respiratory illnesses promote FEV(1) decline in current smokers but not ex-smokers with mild chronic obstructive pulmonary disease: results from the lung health study. Am J Respir Crit Care Med. 2001; 164:358–364. PMID: 11500333.15. Cote CG, Dordelly LJ, Celli BR. Impact of COPD exacerbations on patient-centered outcomes. Chest. 2007; 131:696–704. PMID: 17356082.
Article16. Vestbo J, Edwards LD, Scanlon PD, Yates JC, Agusti A, Bakke P, et al. Changes in forced expiratory volume in 1 second over time in COPD. N Engl J Med. 2011; 365:1184–1192. PMID: 21991892.
Article17. Agusti A, Calverley PM, Celli B, Coxson HO, Edwards LD, Lomas DA, et al. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir Res. 2010; 11:122. PMID: 20831787.
Article18. Seemungal TA, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998; 157(5 Pt 1):1418–1422. PMID: 9603117.
Article19. Connors AF Jr, Dawson NV, Thomas C, Harrell FE Jr, Desbiens N, Fulkerson WJ. Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments). Am J Respir Crit Care Med. 1996; 154(4 Pt 1):959–967. PMID: 8887592.
Article20. Gunen H, Hacievliyagil SS, Kosar F, Mutlu LC, Gulbas G, Pehlivan E, et al. Factors affecting survival of hospitalised patients with COPD. Eur Respir J. 2005; 26:234–241. PMID: 16055870.
Article21. Soler-Cataluna JJ, Martinez-Garcia MA, Roman Sanchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005; 60:925–931. PMID: 16055622.
Article22. Hallin R, Koivisto-Hursti UK, Lindberg E, Janson C. Nutritional status, dietary energy intake and the risk of exacerbations in patients with chronic obstructive pulmonary disease (COPD). Respir Med. 2006; 100:561–567. PMID: 16019198.
Article23. Zapatero A, Barba R, Ruiz J, Losa JE, Plaza S, Canora J, et al. Malnutrition and obesity: influence in mortality and readmissions in chronic obstructive pulmonary disease patients. J Hum Nutr Diet. 2013; 26(Suppl 1):16–22. PMID: 23656492.
Article24. Donaldson GC, Wilkinson TM, Hurst JR, Perera WR, Wedzicha JA. Exacerbations and time spent outdoors in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005; 171:446–452. PMID: 15579723.
Article25. Bagade AA, Jiandani MP, Mehta A. Medical research council dyspnoea score and forced expiratory volume in one second as the predictors of vertical climbing in chronic obstructive pulmonary disease patients. Int J Res Med Sci. 2017; 5:1558–1562.
Article26. Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999; 54:581–586. PMID: 10377201.
Article27. Kaymaz D, Candemir IC, Ergun P, Demir N, Tasdemir F, Demir P. Relation between upper-limb muscle strength with exercise capacity, quality of life and dyspnea in patients with severe chronic obstructive pulmonary disease. Clin Respir J. 2018; 12:1257–1263. PMID: 28618190.
Article28. Stenton C. The MRC breathlessness scale. Occup Med (Lond). 2008; 58:226–227. PMID: 18441368.
Article29. Divo M, Cote C, de Torres JP, Casanova C, Marin JM, Pinto-Plata V, et al. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012; 186:155–161. PMID: 22561964.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical History and Diagnosis of Chronic Obstructive Pulmonary Disease (COPD)
- Evaluation of Quality of Life with the Chronic Obstructive Pulmonary Disease Assessment Test in Chronic Obstructive Pulmonary Disease and the Effect of Dyspnea on Disease-Specific Quality of Life in These Patients
- Phenotype of asthma-chronic obstructive pulmonary disease overlap syndrome
- Nutritional Assessment in Patients with Chronic Obstructive Pulmonary Disease
- Application of a New Spirometric Reference Equation and Its Impact on the Staging of Korean Chronic Obstructive Pulmonary Disease Patients