Endocrinol Metab.
2018 Jun;33(2):296-304. 10.3803/EnM.2018.33.2.296.
Influence of Vitamin D Deficiency on Progression of Experimental Otitis Media in Rats
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, BK21plus, Korea University College of Medicine, Seoul, Korea.
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea. hschoi402@dumc.or.kr
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea. cho69@dumc.or.kr
- KMID: 2420500
- DOI: http://doi.org/10.3803/EnM.2018.33.2.296
Abstract
- BACKGROUND
Vitamin D plays an important role in the immune response against infection. The purpose of the present study was to investigate the influence of vitamin D deficiency on the progression of otitis media (OM) using an experimental rat model.
METHODS
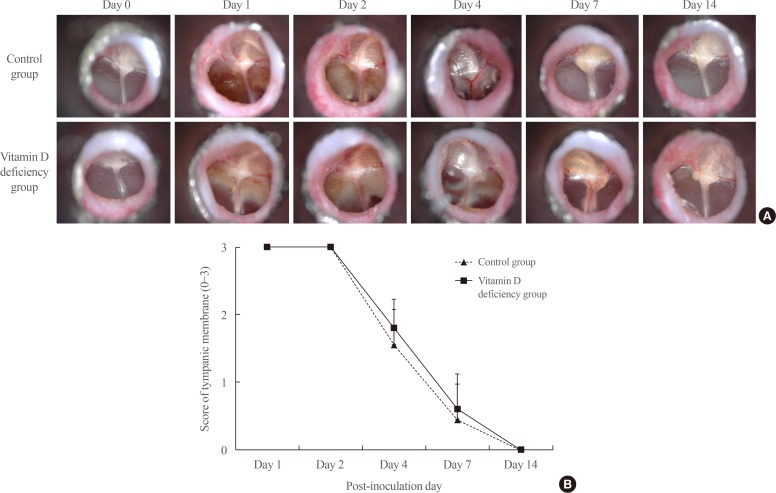
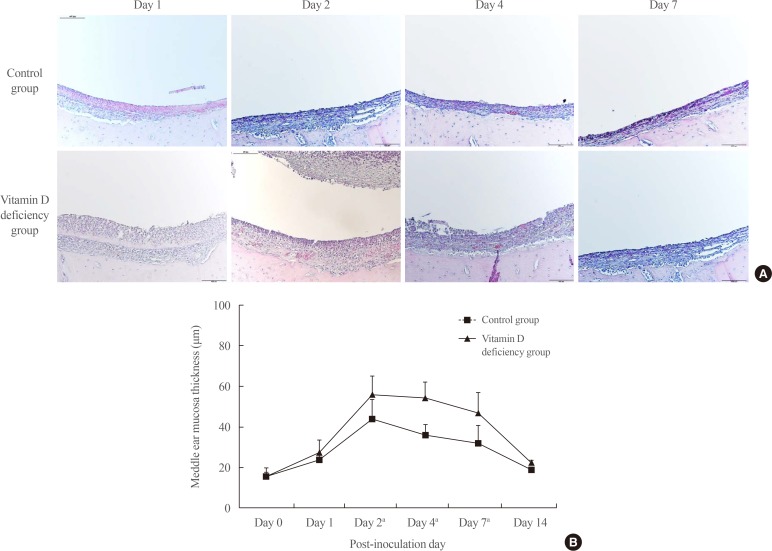
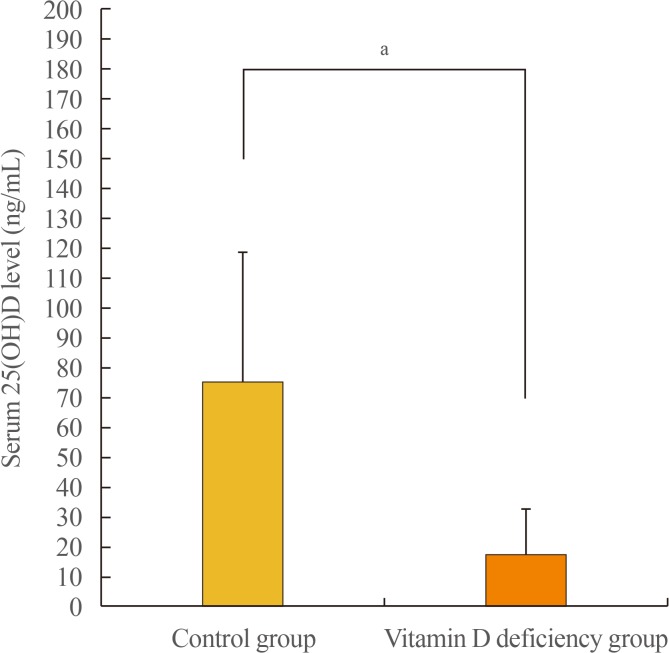
Four-week-old male Sprague-Dawley rats (n=72) were divided into two groups based on their diet: a control diet group (n=36) and a vitamin D-deficient diet group (n=36). After 8 weeks of diet, experimental OM was induced by inoculation of non-typeable Haemophilus influenzae in the middle ear cavity. The rats were evaluated with otomicroscopy to determine the inflammation in the middle ear mucosa on days 1, 2, 4, 7, and 14 post-inoculation. Bullae from sacrificed rats were collected and analyzed histologically.
RESULTS
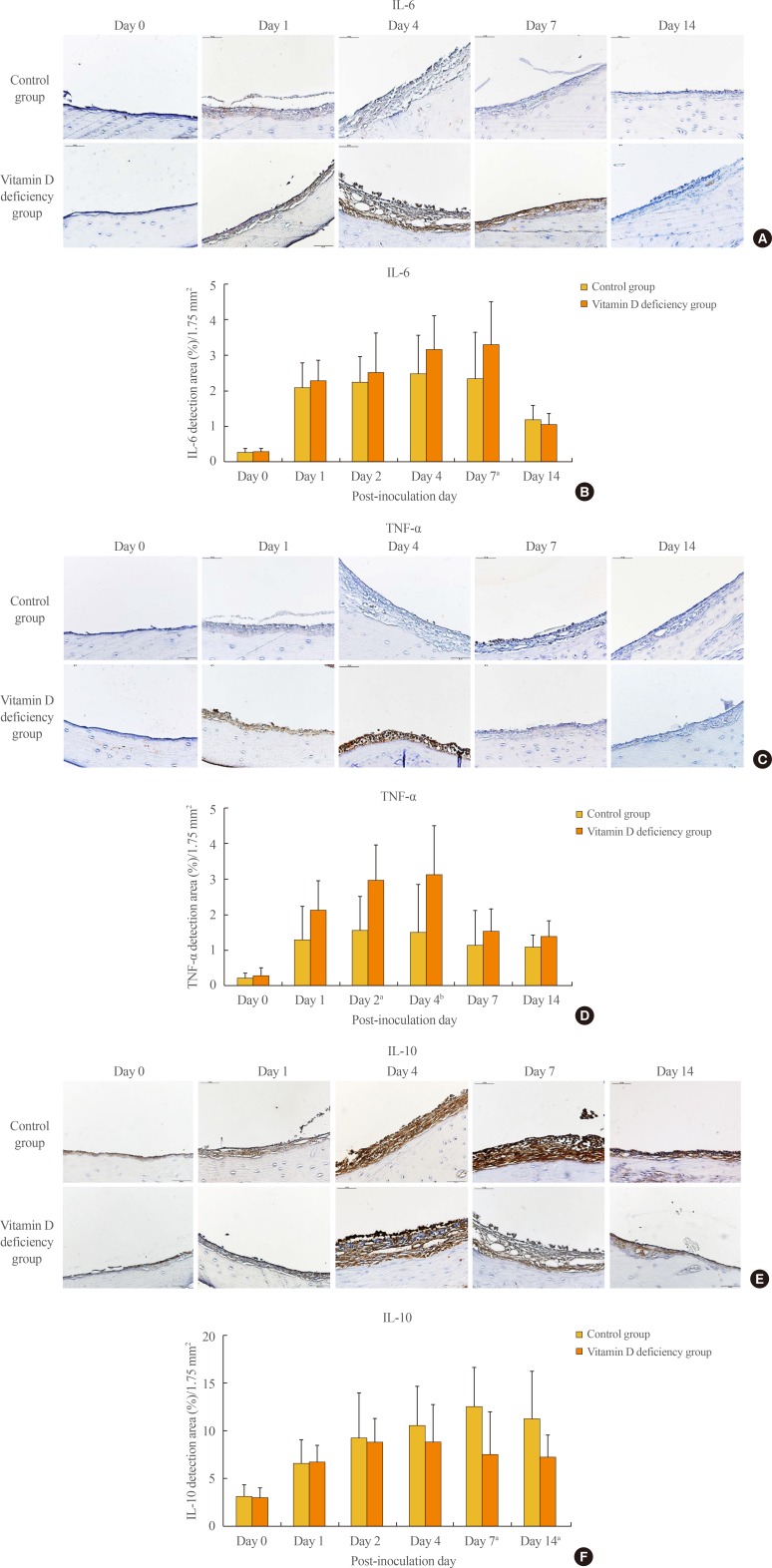
The middle ear mucosa from rats with vitamin D deficiency showed a significantly higher thickness than that of controls during the course of OM. The maximum mucosal thickness was 56.0±9.1 µm in the vitamin D deficiency group, and 43.9±9.8 µm in the control group, although there was no significant difference in the tympanic membrane score between the two groups evaluated with otomicroscopy. An immunohistochemical study showed increased expression of interleukin 6 (IL-6) and tumor necrosis factor α in rats manifesting vitamin D deficiency and decreased expression of IL-10 compared with controls.
CONCLUSION
Our results showed that vitamin D deficiency may exacerbate the pathophysiological changes of OM via altered cytokine production. Therefore, maintaining vitamin D status in the optimal range may be beneficial for proper management of OM.
Keyword
MeSH Terms
-
Animals
Diet
Ear, Middle
Haemophilus influenzae
Humans
Inflammation
Interleukin-10
Interleukin-6
Male
Models, Animal
Mucous Membrane
Otitis Media*
Otitis*
Rats*
Rats, Sprague-Dawley
Tumor Necrosis Factor-alpha
Tympanic Membrane
Vitamin D Deficiency*
Vitamin D*
Vitamins*
Interleukin-10
Interleukin-6
Tumor Necrosis Factor-alpha
Vitamin D
Vitamins
Figure
Reference
-
1. Prietl B, Treiber G, Pieber TR, Amrein K. Vitamin D and immune function. Nutrients. 2013; 5:2502–2521. PMID: 23857223.
Article2. Gunville CF, Mourani PM, Ginde AA. The role of vitamin D in prevention and treatment of infection. Inflamm Allergy Drug Targets. 2013; 12:239–245. PMID: 23782205.
Article3. Borella E, Nesher G, Israeli E, Shoenfeld Y. Vitamin D: a new anti-infective agent. Ann N Y Acad Sci. 2014; 1317:76–83. PMID: 24593793.
Article4. Bouillon R, Carmeliet G, Verlinden L, van Etten E, Verstuyf A, Luderer HF, et al. Vitamin D and human health: lessons from vitamin D receptor null mice. Endocr Rev. 2008; 29:726–776. PMID: 18694980.
Article5. Rathored J, Sharma SK, Singh B, Banavaliker JN, Sreenivas V, Srivastava AK, et al. Risk and outcome of multidrug-resistant tuberculosis: vitamin D receptor polymorphisms and serum 25(OH)D. Int J Tuberc Lung Dis. 2012; 16:1522–1528. PMID: 22990231.
Article6. Aslan S, Akil I, Aslan G, Onay H, Ozyut BC, Ozkinay F. Vitamin D receptor gene polymorphism in children with urinary tract infection. Pediatr Nephrol. 2012; 27:417–421. PMID: 21947233.
Article7. Teele DW, Klein JO, Rosner B. Epidemiology of otitis media during the first seven years of life in children in greater Boston: a prospective, cohort study. J Infect Dis. 1989; 160:83–94. PMID: 2732519.
Article8. Mittal R, Kodiyan J, Gerring R, Mathee K, Li JD, Grati M, et al. Role of innate immunity in the pathogenesis of otitis media. Int J Infect Dis. 2014; 29:259–267. PMID: 25447732.
Article9. Cho CG, Gong SH, Kim HB, Song JJ, Park JH, Lim YS, et al. Role of group 3 innate lymphoid cells during experimental otitis media in a rat model. Int J Pediatr Otorhinolaryngol. 2016; 88:146–152. PMID: 27497403.
Article10. Lim DJ, Birck H. Ultrastructural pathology of the middle ear mucosa in serous otitis media. Ann Otol Rhinol Laryngol. 1971; 80:838–853. PMID: 5127754.
Article11. Cho CG. Animal models of otitis media. Korean J Otorhinolaryngol-Head Neck Surg. 2015; 58:371–377.
Article12. Cayir A, Turan MI, Ozkan O, Cayir Y, Kaya A, Davutoglu S, et al. Serum vitamin D levels in children with recurrent otitis media. Eur Arch Otorhinolaryngol. 2014; 271:689–693. PMID: 23543299.
Article13. Walker RE, Bartley J, Camargo CA Jr, Flint D, Thompson JM, Mitchell EA. Higher serum 25(OH)D concentration is associated with lower risk of chronic otitis media with effusion: a case-control study. Acta Paediatr. 2017; 106:1487–1492. PMID: 28477429.
Article14. Marchisio P, Consonni D, Baggi E, Zampiero A, Bianchini S, Terranova L, et al. Vitamin D supplementation reduces the risk of acute otitis media in otitis-prone children. Pediatr Infect Dis J. 2013; 32:1055–1060. PMID: 23694840.
Article15. Li HB, Tai XH, Sang YH, Jia JP, Xu ZM, Cui XF, et al. Association between vitamin D and development of otitis media: a PRISMA-compliant meta-analysis and systematic review. Medicine (Baltimore). 2016; 95:e4739. PMID: 27749530.16. Hansdottir S, Monick MM, Lovan N, Powers L, Gerke A, Hunninghake GW. Vitamin D decreases respiratory syncytial virus induction of NF-kappaB-linked chemokines and cytokines in airway epithelium while maintaining the antiviral state. J Immunol. 2010; 184:965–974. PMID: 20008294.17. McNally P, Coughlan C, Bergsson G, Doyle M, Taggart C, Adorini L, et al. Vitamin D receptor agonists inhibit proinflammatory cytokine production from the respiratory epithelium in cystic fibrosis. J Cyst Fibros. 2011; 10:428–434. PMID: 21784717.
Article18. Wang TT, Nestel FP, Bourdeau V, Nagai Y, Wang Q, Liao J, et al. Cutting edge: 1,25-dihydroxyvitamin D3 is a direct inducer of antimicrobial peptide gene expression. J Immunol. 2004; 173:2909–2912. PMID: 15322146.
Article19. Gombart AF, Borregaard N, Koeffler HP. Human cathelicidin antimicrobial peptide (CAMP) gene is a direct target of the vitamin D receptor and is strongly up-regulated in myeloid cells by 1,25-dihydroxyvitamin D3. FASEB J. 2005; 19:1067–1077. PMID: 15985530.20. Liu PT, Stenger S, Li H, Wenzel L, Tan BH, Krutzik SR, et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006; 311:1770–1773. PMID: 16497887.
Article21. Rockett KA, Brookes R, Udalova I, Vidal V, Hill AV, Kwiatkowski D. 1,25-DihydroxyvitaminD3 induces nitric oxide synthase and suppresses growth of Mycobacterium tuberculosis in a human macrophage-like cell line. Infect Immun. 1998; 66:5314–5321. PMID: 9784538.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of Animal Models of Otitis Media
- Experimental otitis media with effusion induced by lipopolysaccharides from E. coli: the effects of endotoxin to the chronically of OME
- The Effects of Antibiotics and Steroid on the Middle Ear Mucosa in the Rats with Experimental Acute Otitis Media
- Management of otitis media
- Middle ear histopathology in children with otitis media with effusion