Obstet Gynecol Sci.
2018 Mar;61(2):202-208. 10.5468/ogs.2018.61.2.202.
Fetal Doppler to predict cesarean delivery for non-reassuring fetal status in the severe small-for-gestational-age fetuses of late preterm and term
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. mongkoko@catholic.ac.kr
- KMID: 2420173
- DOI: http://doi.org/10.5468/ogs.2018.61.2.202
Abstract
OBJECTIVE
To evaluate the significance of fetal Doppler parameters in predicting adverse neonatal outcomes and the risk of cesarean delivery due to non-reassuring fetal status, in severe small for gestational age (SGA) fetuses of late preterm and term gestation.
METHODS
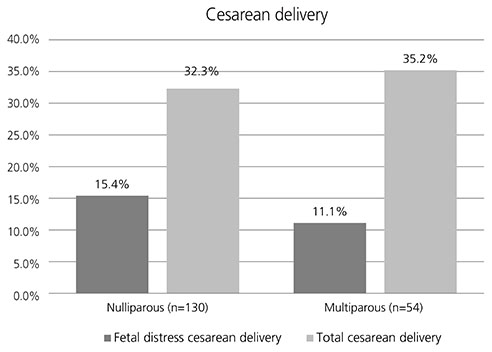
Fetal brain and umbilical artery (UmA) Doppler parameters of cerebroplacental ratio (CPR) and UmA pulsatility index (PI) were evaluated in a cohort of 184 SGA fetuses between 34 and 41 weeks gestational age, who were less than the 5th percentile. The risks of neonatal morbidities and cesarean delivery due to non-reassuring fetal status were analyzed.
RESULTS
Univariate analysis revealed that abnormal CPR was significantly associated with cesarean delivery due to non-reassuring fetal status (P=0.018), but not with neonatal morbidities. However, abnormal CPR did not increase the risk of cesarean delivery due to non-reassuring fetal status in multivariate logistic regression analysis. Abnormal CPR with abnormal PI of UmA was associated with low Apgar score at 1 minute (P=0.048), mechanical ventilation (P=0.013) and cesarean delivery due to non-reassuring fetal status (P < 0.001), in univariate analysis. It increased risk of cesarean delivery for non-reassuring fetal status (adjusted odds ratio, 7.0; 95% confidence interval, 1.2-41.3; P=0.033), but did not increase risk of low Apgar score or mechanical ventilation in multivariate logistic regression analysis.
CONCLUSION
Abnormal CPR with abnormal PI of UmA increases the risk of cesarean delivery for non-reassuring fetal status, in severe SGA fetuses of late preterm and term. Monitoring of CPR and PI of UmA can help guide management including maternal hospitalization and fetal monitoring.
MeSH Terms
Figure
Cited by 1 articles
-
Management of isolated oligohydramnios in Korea: a questionnaire-based study of clinical practice patterns among the members of the Korean Society of Maternal Fetal Medicine
Seung Woo Yang, Yihua Jin, Eun bi Jang, Hee Sun Kim, In Sook Sohn, Han Sung Kwon, Han-Sung Hwang
Obstet Gynecol Sci. 2020;63(5):586-593. doi: 10.5468/ogs.20061.
Reference
-
1. McIntire DD, Bloom SL, Casey BM, Leveno KJ. Birth weight in relation to morbidity and mortality among newborn infants. N Engl J Med. 1999; 340:1234–1238.
Article2. Khalil A, Thilaganathan B. Role of uteroplacental and fetal Doppler in identifying fetal growth restriction at term. Best Pract Res Clin Obstet Gynaecol. 2017; 38:38–47.
Article3. Severi FM, Bocchi C, Visentin A, Falco P, Cobellis L, Florio P, et al. Uterine and fetal cerebral Doppler predict the outcome of third-trimester small-for-gestational age fetuses with normal umbilical artery Doppler. Ultrasound Obstet Gynecol. 2002; 19:225–228.
Article4. Sirico A, Diemert A, Glosemeyer P, Hecher K. Prediction of adverse perinatal outcome by cerebroplacental ratio adjusted for estimated fetal weight. Ultrasound Obstet Gynecol. 2017; Epub.
Article5. Lee JK, Jang HL, Kang BH, Lee KS, Choi YS, Shim KS, et al. Percentile distributions of birth weight according to gestational ages in Korea (2010–2012). J Korean Med Sci. 2016; 31:939–949.
Article6. Warshak CR, Masters H, Regan J, DeFranco E. Doppler for growth restriction: the association between the cerebroplacental ratio and a reduced interval to delivery. J Perinatol. 2015; 35:332–337.
Article7. Acharya G, Wilsgaard T, Berntsen GK, Maltau JM, Kiserud T. Reference ranges for serial measurements of umbilical artery Doppler indices in the second half of pregnancy. Am J Obstet Gynecol. 2005; 192:937–944.
Article8. Blackwell SC, Grobman WA, Antoniewicz L, Hutchinson M, Gyamfi Bannerman C. Interobserver and intraobserver reliability of the NICHD 3-Tier Fetal Heart Rate Interpretation System. Am J Obstet Gynecol. 2011; 205:378.e1–378.e5.
Article9. Arbeille P, Roncin A, Berson M, Patat F, Pourcelot L. Exploration of the fetal cerebral blood flow by duplex Doppler--linear array system in normal and pathological pregnancies. Ultrasound Med Biol. 1987; 13:329–337.
Article10. Khalil A, Morales-Roselló J, Townsend R, Morlando M, Papageorghiou A, Bhide A, et al. Value of third-trimester cerebroplacental ratio and uterine artery Doppler indices as predictors of stillbirth and perinatal loss. Ultrasound Obstet Gynecol. 2016; 47:74–80.
Article11. Dunn L, Sherrell H, Kumar S. Review: Systematic review of the utility of the fetal cerebroplacental ratio measured at term for the prediction of adverse perinatal outcome. Placenta. 2017; 54:68–75.
Article12. Mari G, Tate DL. Detection and surveillance of IUGR [Internet]. North Olmsted (OH): Contemporary OB/GYN;2013. cited 2017 May 8. Available from: http://contemporaryobgyn.modernmedicine.com/contemporary-obgyn/content/tags/intrauterine-growth-restriction/detection-and-surveillance-iugr.13. Makhseed M, Jirous J, Ahmed MA, Viswanathan DL. Middle cerebral artery to umbilical artery resistance index ratio in the prediction of neonatal outcome. Int J Gynaecol Obstet. 2000; 71:119–125.
Article14. Gramellini D, Folli MC, Raboni S, Vadora E, Merialdi A. Cerebral-umbilical Doppler ratio as a predictor of adverse perinatal outcome. Obstet Gynecol. 1992; 79:416–420.
Article15. Flood K, Unterscheider J, Daly S, Geary MP, Kennelly MM, McAuliffe FM, et al. The role of brain sparing in the prediction of adverse outcomes in intrauterine growth restriction: results of the multicenter PORTO Study. Am J Obstet Gynecol. 2014; 211:288.e1–288.e5.16. Ebrashy A, Azmy O, Ibrahim M, Waly M, Edris A. Middle cerebral/umbilical artery resistance index ratio as sensitive parameter for fetal well-being and neonatal outcome in patients with preeclampsia: case-control study. Croat Med J. 2005; 46:821–825.17. Bahado-Singh RO, Kovanci E, Jeffres A, Oz U, Deren O, Copel J, et al. The Doppler cerebroplacental ratio and perinatal outcome in intrauterine growth restriction. Am J Obstet Gynecol. 1999; 180:750–756.
Article18. Arias F. Accuracy of the middle-cerebral-to-umbilical-artery resistance index ratio in the prediction of neonatal outcome in patients at high risk for fetal and neonatal complications. Am J Obstet Gynecol. 1994; 171:1541–1545.19. American College of Obstetricians and Gynecologists. ACOG Practice bulletin no. 134: fetal growth restriction. Obstet Gynecol. 2013; 121:1122–1133.20. Arabin B, Goerges J, Bilardo CM. The importance of the cerebroplacental ratio in the evaluation of fetal well-being in SGA and AGA fetuses. Am J Obstet Gynecol. 2016; 214:298–299.
Article21. Khalil AA, Morales-Rosello J, Morlando M, Hannan H, Bhide A, Papageorghiou A, et al. Is fetal cerebroplacental ratio an independent predictor of intrapartum fetal compromise and neonatal unit admission? Am J Obstet Gynecol. 2015; 213:54.e1–54.10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebroplacental Ratio to Predict Adverse Perinatal Outcomes in Small-for-Gestational-Age Pregnancies
- Umbilical Artery Doppler Velocimetry in Small for Gestational Age Fetuses
- The Clinical Significance of Absence of Umbilical Artery End-Diastolic Flow in Severe Pre-Eclampsia and Eclampsia
- Decision-to-delivery interval in emergency cesarean delivery in tertiary care hospital in Thailand
- Cardiovascular Doppler Flow Waveforms in Human Fetuses