Obstet Gynecol Sci.
2018 Jan;61(1):102-110. 10.5468/ogs.2018.61.1.102.
Efficacy of luteal estrogen administration and an early follicular Gonadotropin-releasing hormone antagonist priming protocol in poor responders undergoing in vitro fertilization
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Cheil General Hospital and Women's Healthcare Center, College of Medicine, Dankook University, Seoul, Korea.
- 2Department of Obstetrics and Gynecology, Maria Fertility Hospital, Seoul, Korea. deligh@naver.com
- KMID: 2420158
- DOI: http://doi.org/10.5468/ogs.2018.61.1.102
Abstract
OBJECTIVES
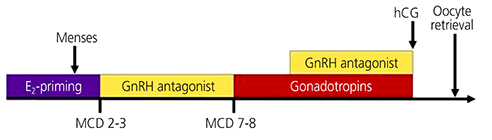
We investigated whether luteal estrogen administration and an early follicular Gonadotropin-releasing hormone antagonist (E/G-ant) priming protocol improves clinical outcomes in poor responders to controlled ovarian stimulation for in vitro fertilization (IVF)-embryo transfer, and identified underlying mechanisms.
METHODS
This restrospective study consisted of 65 poor responders who underwent the E/G-ant priming protocol. Sixty-four other poor responders undergoing conventional protocols without pretreatment were included as the control group. Clinical outcomes were compared between 2 groups.
RESULTS
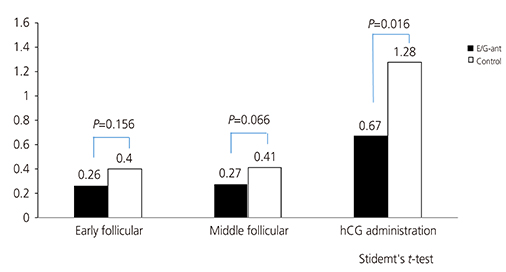
The E/G-ant priming protocol group exhibited improvements over the control group in terms of the number of retrieved oocytes (3.58±2.24 vs. 1.70±1.45; P=0.000), mature oocytes (2.68±2.11 vs. 1.65±1.23; P=0.000), fertilized oocytes (2.25±1.74 vs. 1.32±1.26; P=0.001), good embryos (1.62±0.91 vs. 1.14±0.90, P=0.021). Day 3 follicle-stimulating hormone (FSH; 8.40±4.84 vs. 16.39±13.56; P=0.000) and pre-ovulation progesterone levels (0.67 vs. 1.28 ng/mL; P=0.016) were significantly higher in the control group than in the E/G-ant priming group. The overall rate of positive human chorionic gonadotropin tests was higher in the E/G-ant priming group than in the control group (32.3% vs.16.1%; P=0.039). Also, clinical pregnancy rate (26.2% vs. 12.5%; P=0.048) and the rate of live births (23.1% vs. 7.1%; P=0.023) were significantly higher in the E/G-ant priming group than in the control group.
CONCLUSION
The E/G-ant priming protocol would lead to promising results in poor responders to IVF by suppressing endogenous FSH and by preventing premature luteinization.
Keyword
MeSH Terms
-
Chorionic Gonadotropin
Embryonic Structures
Estrogens*
Fertilization in Vitro*
Follicle Stimulating Hormone
Gonadotropin-Releasing Hormone*
In Vitro Techniques*
Live Birth
Lutein
Luteinization
Oocytes
Ovulation Induction
Pregnancy Rate
Progesterone
Chorionic Gonadotropin
Estrogens
Follicle Stimulating Hormone
Gonadotropin-Releasing Hormone
Lutein
Progesterone
Figure
Reference
-
1. Hendriks DJ, Mol BW, Bancsi LF, Te Velde ER, Broekmans FJ. Antral follicle count in the prediction of poor ovarian response and pregnancy after in vitro fertilization: a meta-analysis and comparison with basal follicle-stimulating hormone level. Fertil Steril. 2005; 83:291–301.2. Pandian Z, McTavish AR, Aucott L, Hamilton MP, Bhattacharya S. Interventions for ‘poor responders’ to controlled ovarian hyper stimulation (COH) in in-vitro fertilisation (IVF). Cochrane Database Syst Rev. 2010; CD004379.
Article3. Cakmak H, Tran ND, Zamah AM, Cedars MI, Rosen MP. A novel “delayed start” protocol with gonadotropin-releasing hormone antagonist improves outcomes in poor responders. Fertil Steril. 2014; 101:1308–1314.
Article4. Polyzos NP, Devroey P. A systematic review of randomized trials for the treatment of poor ovarian responders: is there any light at the end of the tunnel? Fertil Steril. 2011; 96:1058–1061.e7.5. Keay SD, Liversedge NH, Mathur RS, Jenkins JM. Assisted conception following poor ovarian response to gonadotrophin stimulation. Br J Obstet Gynaecol. 1997; 104:521–527.
Article6. Surrey ES, Schoolcraft WB. Evaluating strategies for improving ovarian response of the poor responder undergoing assisted reproductive techniques. Fertil Steril. 2000; 73:667–676.
Article7. Vollenhoven B, Osianlis T, Catt J. Is there an ideal stimulation regimen for IVF for poor responders and does it change with age? J Assist Reprod Genet. 2008; 25:523–529.
Article8. Jenkins JM, Davies DW, Devonport H, Anthony FW, Gadd SC, Watson RH, et al. Comparison of ‘poor’ responders with ‘good’ responders using a standard buserelin/human menopausal gonadotrophin regime for in-vitro fertilization. Hum Reprod. 1991; 6:918–921.9. Cheung LP, Lam PM, Lok IH, Chiu TT, Yeung SY, Tjer CC, et al. GnRH antagonist versus long GnRH agonist protocol in poor responders undergoing IVF: a randomized controlled trial. Hum Reprod. 2005; 20:616–621.
Article10. Ubaldi F, Vaiarelli A, D'Anna R, Rienzi L. Management of poor responders in IVF: is there anything new. BioMed Res Int. 2014; 2014:352098.
Article11. Kyrou D, Kolibianakis EM, Venetis CA, Papanikolaou EG, Bontis J, Tarlatzis BC. How to improve the probability of pregnancy in poor responders undergoing in vitro fertilization: a systematic review and meta-analysis. Fertil Steril. 2009; 91:749–766.12. Kligman I, Rosenwaks Z. Differentiating clinical profiles: predicting good responders, poor responders, and hyperresponders. Fertil Steril. 2001; 76:1185–1190.
Article13. Saldeen P, Källen K, Sundström P. The probability of successful IVF outcome after poor ovarian response. Acta Obstet Gynecol Scand. 2007; 86:457–461.
Article14. Rosen MP, Shen S, Dobson AT, Rinaudo PF, McCulloch CE, Cedars MI. A quantitative assessment of follicle size on oocyte developmental competence. Fertil Steril. 2008; 90:684–690.
Article15. Devreker F, Pogonici E, De Maertelaer V, Revelard P, Van den Bergh M, Englert Y. Selection of good embryos for transfer depends on embryo cohort size: implications for the ‘mild ovarian stimulation’ debate. Hum Reprod. 1999; 14:3002–3008.
Article16. Opsahl MS, Blauer KL, Black SH, Lincoln SR, Thorsell L, Sherins RJ. The number of embryos available for transfer predicts successful pregnancy outcome in women over 39 years with normal ovarian hormonal reserve testing. J Assist Reprod Genet. 2001; 18:551–556.17. Fanchin R, Cunha-Filho JS, Schonäuer LM, Kadoch IJ, Cohen-Bacri P, Frydman R. Coordination of early antral follicles by luteal estradiol administration provides a basis for alternative controlled ovarian hyperstimulation regimens. Fertil Steril. 2003; 79:316–321.
Article18. Klein NA, Battaglia DE, Fujimoto VY, Davis GS, Bremner WJ, Soules MR. Reproductive aging: accelerated ovarian follicular development associated with a monotropic follicle-stimulating hormone rise in normal older women. J Clin Endocrinol Metab. 1996; 81:1038–1045.
Article19. Chun SY, Eisenhauer KM, Minami S, Billig H, Perlas E, Hsueh AJ. Hormonal regulation of apoptosis in early antral follicles: follicle-stimulating hormone as a major survival factor. Endocrinology. 1996; 137:1447–1456.
Article20. Dragisic KG, Davis OK, Fasouliotis SJ, Rosenwaks Z. Use of a luteal estradiol patch and a gonadotropin-releasing hormone antagonist suppression protocol before gonadotropin stimulation for in vitro fertilization in poor responders. Fertil Steril. 2005; 84:1023–1026.21. Fanchin R, Salomon L, Castelo-Branco A, Olivennes F, Frydman N, Frydman R. Luteal estradiol pre-treatment coordinates follicular growth during controlled ovarian hyperstimulation with GnRH antagonists. Hum Reprod. 2003; 18:2698–2703.
Article22. Van Soom A, Mateusen B, Leroy J, De Kruif A. Assessment of mammalian embryo quality: what can we learn from embryo morphology? Reprod Biomed Online. 2003; 7:664–670.
Article23. Frattarelli JL, Hill MJ, McWilliams GD, Miller KA, Bergh PA, Scott RT Jr. A luteal estradiol protocol for expected poor-responders improves embryo number and quality. Fertil Steril. 2008; 89:1118–1122.
Article24. Chang EM, Han JE, Won HJ, Kim YS, Yoon TK, Lee WS. Effect of estrogen priming through luteal phase and stimulation phase in poor responders in in-vitro fertilization. J Assist Reprod Genet. 2012; 29:225–230.25. Copperman AB. Antagonists in poor-responder patients. Fertil Steril. 2003; 80:Suppl 1. S16–S24.
Article26. Frankfurter D, Dayal M, Dubey A, Peak D, Gindoff P. Novel follicular-phase gonadotropin-releasing hormone antagonist stimulation protocol for in vitro fertilization in the poor responder. Fertil Steril. 2007; 88:1442–1445.27. Younis JS, Soltsman S, Izhaki I, Radin O, Bar-Ami S, Ben-Ami M. Early and short follicular gonadotropin-releasing hormone antagonist supplementation improves the meiotic status and competence of retrieved oocytes in in vitro fertilization-embryo transfer cycles. Fertil Steril. 2010; 94:1350–1355.28. Blockeel C, Devroey P. Optimisation of the follicular phase in IVF/ICSI. Facts Views Vis ObGyn. 2012; 4:203–212.29. Fanchin R, Hourvitz A, Olivennes F, Taieb J, Hazout A, Frydman R. Premature progesterone elevation spares blastulation but not pregnancy rates in in vitro fertilization with coculture. Fertil Steril. 1997; 68:648–652.30. Fanchin R, Righini C, Olivennes F, Ferreira AL, de Ziegler D, Frydman R. Consequences of premature progesterone elevation on the outcome of in vitro fertilization: insights into a controversy. Fertil Steril. 1997; 68:799–805.31. Hugues JN. Impact of ‘LH activity’ supplementation on serum progesterone levels during controlled ovarian stimulation: a systematic review. Hum Reprod. 2012; 27:232–243.
Article32. Shulman A, Ghetler Y, Beyth Y, Ben-Nun I. The significance of an early (premature) rise of plasma progesterone in in vitro fertilization cycles induced by a “long protocol” of gonadotropin releasing hormone analogue and human menopausal gonadotropins. J Assist Reprod Genet. 1996; 13:207–211.33. Lidor AL, Goldenberg M, Cohen SB, Seidman DS, Mashiach S, Rabinovici J. Management of women with polycystic ovary syndrome who experienced premature luteinization during clomiphene citrate treatment. Fertil Steril. 2000; 74:749–752.
Article34. Younis JS, Matilsky M, Radin O, Ben-Ami M. Increased progesterone/estradiol ratio in the late follicular phase could be related to low ovarian reserve in in vitro fertilization-embryo transfer cycles with a long gonadotropin-releasing hormone agonist. Fertil Steril. 2001; 76:294–299.35. Venetis CA, Kolibianakis EM, Tarlatzis BC. Progesterone elevation and probability of pregnancy after IVF: facts and fiction. Hum Reprod Update. 2008; 14:538.
Article36. Xu B, Li Z, Zhang H, Jin L, Li Y, Ai J, et al. Serum progesterone level effects on the outcome of in vitro fertilization in patients with different ovarian response: an analysis of more than 10,000 cycles. Fertil Steril. 2012; 97:1321–1327.e1-4.37. Venetis CA, Kolibianakis EM, Bosdou JK, Tarlatzis BC. Progesterone elevation and probability of pregnancy after IVF: a systematic review and meta-analysis of over 60 000 cycles. Hum Reprod Update. 2013; 19:433–457.
Article38. Ferraretti AP, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L, et al. ESHRE consensus on the definition of ‘poor response’ to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011; 26:1616–1624.39. Jansen R, Mortimer D. Towards reproductive certainty: fertility and genetics beyond 1999: the plenary Proceedings of the 11th World Congress. London: CRC Press;1999.40. Garcia JE, Jones GS, Acosta AA, Wright G Jr. Human menopausal gonadotropin/human chorionic gonadotropin follicular maturation for oocyte aspiration: phase II, 1981. Fertil Steril. 1983; 39:174–179.
Article41. Templeton A, Morris JK, Parslow W. Factors that affect outcome of in-vitro fertilisation treatment. Lancet. 1996; 348:1402–1406.42. Ulug U, Ben-Shlomo I, Turan E, Erden HF, Akman MA, Bahceci M. Conception rates following assisted reproduction in poor responder patients: a retrospective study in 300 consecutive cycles. Reprod Biomed Online. 2003; 6:439–443.
Article43. Hendriks DJ, te Velde ER, Looman CW, Bancsi LF, Broekmans FJ. Expected poor ovarian response in predicting cumulative pregnancy rates: a powerful tool. Reprod Biomed Online. 2008; 17:727–736.
Article44. Gougeon A, Lefèvre B. Evolution of the diameters of the largest healthy and atretic follicles during the human menstrual cycle. J Reprod Fertil. 1983; 69:497–502.
Article45. Bosch E, Valencia I, Escudero E, Crespo J, Simón C, Remohí J, et al. Premature luteinization during gonadotropin-releasing hormone antagonist cycles and its relationship with in vitro fertilization outcome. Fertil Steril. 2003; 80:1444–1449.46. Harada T, Yoshida S, Katagiri C, Takao N, Ikenari T, Toda T, et al. Reduced implantation rate associated with a subtle rise in serum progesterone concentration during the follicular phase of cycles stimulated with a combination of a gonadotrophin-releasing hormone agonist and gonadotrophin. Hum Reprod. 1995; 10:1060–1064.47. Fanchin R, de Ziegler D, Taieb J, Hazout A, Frydman R. Premature elevation of plasma progesterone alters pregnancy rates of in vitro fertilization and embryo transfer. Fertil Steril. 1993; 59:1090–1094.48. Hofmann GE, Khoury J, Johnson CA, Thie J, Scott RT Jr. Premature luteinization during controlled ovarian hyperstimulation for in vitro fertilization-embryo transfer has no impact on pregnancy outcome. Fertil Steril. 1996; 66:980–986.49. Fanchin R, Righini C, Olivennes F, de Ziegler D, Selva J, Frydman R. Premature progesterone elevation does not alter oocyte quality in in vitro fertilization. Fertil Steril. 1996; 65:1178–1183.50. Saleh HA, Omran MS, Draz M. Does subtle progesterone rise on the day of HCG affect pregnancy rate in long agonist ICSI cycles? J Assist Reprod Genet. 2009; 26:239–242.
Article51. Requena A, Cruz M, Bosch E, Meseguer M, García-Velasco JA. High progesterone levels in women with high ovarian response do not affect clinical outcomes: a retrospective cohort study. Reprod Biol Endocrinol. 2014; 12:69.
Article52. Kolibianakis EM, Albano C, Camus M, Tournaye H, Van Steirteghem AC, Devroey P. Prolongation of the follicular phase in in vitro fertilization results in a lower ongoing pregnancy rate in cycles stimulated with recombinant follicle-stimulating hormone and gonadotropin-releasing hormone antagonists. Fertil Steril. 2004; 82:102–107.53. Fleming R, Jenkins J. The source and implications of progesterone rise during the follicular phase of assisted reproduction cycles. Reprod Biomed Online. 2010; 21:446–449.
Article54. Achache H, Revel A. Endometrial receptivity markers, the journey to successful embryo implantation. Hum Reprod Update. 2006; 12:731–746.
Article55. Shufaro Y, Sapir O, Oron G, Ben Haroush A, Garor R, Pinkas H, et al. Progesterone-to-follicle index is better correlated with in vitro fertilization cycle outcome than blood progesterone level. Fertil Steril. 2015; 103:669–674.e3.56. Oudendijk JF, Yarde F, Eijkemans MJ, Broekmans FJ, Broer SL. The poor responder in IVF: is the prognosis always poor?: a systematic review. Hum Reprod Update. 2012; 18:1–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effective of ultrashort-term gonadotropin-releasing hormone agonist administration in controlled ovarian hyperstimulation for in vitro fertilization
- GnRH antagonist multiple dose protocol with oral contraceptive pill pretreatment in poor responders undergoing IVF/ICSI
- Comparison between GnRH Antagonist and Agonist Long Protocols in Poor Responders
- The study for in vitro fertilization using GnRH agonist to tigger follicular maturation
- The effect of aromatase inhibitor letrozole incorporated in gonadotrophin-releasing hormone antagonist multiple dose protocol in poor responders undergoing in vitro fertilization