Obstet Gynecol Sci.
2018 Jan;61(1):1-6. 10.5468/ogs.2018.61.1.1.
Colposcopy at a turning point
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Soonchunhyang University Bucheon Hospital, Bucheon, Korea. khnam@schmc.ac.kr
- KMID: 2420145
- DOI: http://doi.org/10.5468/ogs.2018.61.1.1
Abstract
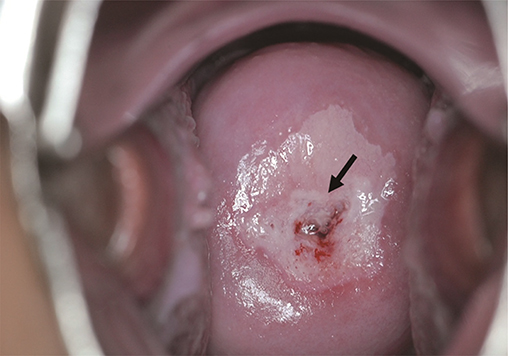
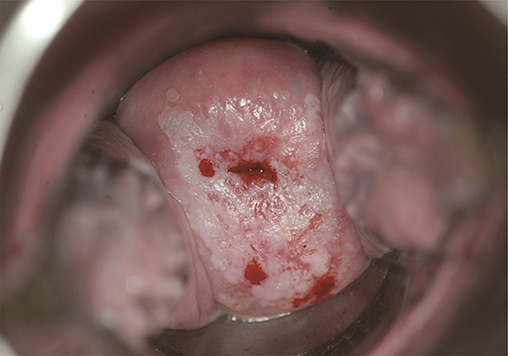
- For women who have abnormal Pap test results, the biopsy under colposcopic evaluation is the gold standard for determining the treatment modality. To increase the effectiveness of colposcopic communication, the International Federation for Cervical Pathology and Colposcopy (IFCPC) recently published fourth new nomenclature, aiming to create an evidence-based terminology. To increase the diagnostic accuracy of colposcopy, multiple biopsies of two or more sites are recommended. Recently, with the introduction of human papillomavirus (HPV) vaccine for cervical cancer prevention, pre-cancerous diseases caused by virus types 16 and 18 have been reduced, which is expected to reduce the number of colposcopic examinations and make colposcopic diagnosis more difficult.
MeSH Terms
Figure
Cited by 1 articles
-
Predictive value of ‘Smartscopy’ for the detection of preinvasive cervical lesions during the COVID-19 pandemic: a diagnostic study
Thamawoot Phoblap, Amornrat Temtanakitpaisan, Apiwat Aue-angkul, Pilaiwan Kleebkaow, Bandit Chumworathayi, Sanguanchoke Luanratanakorn, Yuwadee Itarat
Obstet Gynecol Sci. 2022;65(5):451-458. doi: 10.5468/ogs.22092.
Reference
-
1. Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012 v1.0, cancer incidence and mortality worldwide: IARC cancer base no. 11 [Internet]. Lyon (FR): International Agency for Research on Cancer;2014. cited 2017 May 10. Available from: http://globocan.iarc.fr.2. Sankaranarayanan R. Screening for cancer in low- and middle-income countries. Ann Glob Health. 2014; 80:412–417.
Article3. National Cancer Center (KR). Annual report of cancer statistics in Korea in 2014 [Internet]. Goyang (KR): National Cancer Center;2017. cited 2017 May 10. Available from: http://www.ncc.re.kr/cancerStatsView.ncc?bbsnum=397&searchKey=total&searchValue=&pageNum=1.4. Bornstein J, Bentley J, Bösze P, Girardi F, Haefner H, Menton M, et al. 2011 colposcopic terminology of the International Federation for Cervical Pathology and Colposcopy. Obstet Gynecol. 2012; 120:166–172.
Article5. Vercellino GF, Erdemoglu E, Chiantera V, Vasiljeva K, Malak AH, Schneider A, et al. Clinical relevance of objectifying colposcopy. Arch Gynecol Obstet. 2015; 291:907–915.
Article6. Reid R, Scalzi P. Genital warts and cervical cancer. VII. An improved colposcopic index for differentiating benign papillomaviral infections from high-grade cervical intraepithelial neoplasia. Am J Obstet Gynecol. 1985; 153:611–618.7. Massad LS, Collins YC. Strength of correlations between colposcopic impression and biopsy histology. Gynecol Oncol. 2003; 89:424–428.
Article8. Massad LS, Jeronimo J, Katki HA, Schiffman M; National Institutes of Health/American Society for Colposcopy and Cervical Pathology Research Group. The accuracy of colposcopic grading for detection of high-grade cervical intraepithelial neoplasia. J Low Genit Tract Dis. 2009; 13:137–144.
Article9. Pretorius RG, Zhang WH, Belinson JL, Huang MN, Wu LY, Zhang X, et al. Colposcopically directed biopsy, random cervical biopsy, and endocervical curettage in the diagnosis of cervical intraepithelial neoplasia II or worse. Am J Obstet Gynecol. 2004; 191:430–434.
Article10. Gage JC, Hanson VW, Abbey K, Dippery S, Gardner S, Kubota J, et al. Number of cervical biopsies and sensitivity of colposcopy. Obstet Gynecol. 2006; 108:264–272.
Article11. Wentzensen N, Walker JL, Gold MA, Smith KM, Zuna RE, Mathews C, et al. Multiple biopsies and detection of cervical cancer precursors at colposcopy. J Clin Oncol. 2015; 33:83–89.
Article12. Pretorius RG, Belinson JL, Burchette RJ, Hu S, Zhang X, Qiao YL. Regardless of skill, performing more biopsies increases the sensitivity of colposcopy. J Low Genit Tract Dis. 2011; 15:180–188.
Article13. Nam K, Chung S, Kwak J, Cha S, Kim J, Jeon S, et al. Random biopsy after colposcopy-directed biopsy improves the diagnosis of cervical intraepithelial neoplasia grade 2 or worse. J Low Genit Tract Dis. 2010; 14:346–351.
Article14. Huh WK, Sideri M, Stoler M, Zhang G, Feldman R, Behrens CM. Relevance of random biopsy at the transformation zone when colposcopy is negative. Obstet Gynecol. 2014; 124:670–678.
Article15. Chen Q, Du H, Pretorius RG, Wang C, Yang B, Wang G, et al. High-grade cervical intraepithelial neoplasia detected by colposcopy-directed or random biopsy relative to age, cytology, human papillomavirus 16, and lesion size. J Low Genit Tract Dis. 2016; 20:207–212.
Article16. Sherman ME, Wang SS, Tarone R, Rich L, Schiffman M. Histopathologic extent of cervical intraepithelial neoplasia 3 lesions in the atypical squamous cells of undetermined significance low-grade squamous intraepithelial lesion triage study: implications for subject safety and lead-time bias. Cancer Epidemiol Biomarkers Prev. 2003; 12:372–379.17. Wright TC Jr, Schiffman M, Solomon D, Cox JT, Garcia F, Goldie S, et al. Interim guidance for the use of human papillomavirus DNA testing as an adjunct to cervical cytology for screening. Obstet Gynecol. 2004; 103:304–309.
Article18. Landers EE, Erickson BK, Bae S, Huh WK. Trends in colposcopy volume: where do we go from here? J Low Genit Tract Dis. 2016; 20:292–295.
Article19. Brotherton JM, Malloy M, Budd AC, Saville M, Drennan KT, Gertig DM. Effectiveness of less than three doses of quadrivalent human papillomavirus vaccine against cervical intraepithelial neoplasia when administered using a standard dose spacing schedule: observational cohort of young women in Australia. Papillomavirus Res. 2015; 1:59–73.
Article20. Smith LM, Strumpf EC, Kaufman JS, Lofters A, Schwandt M, Lévesque LE. The early benefits of human papillomavirus vaccination on cervical dysplasia and anogenital warts. Pediatrics. 2015; 135:e1131–e1140.
Article21. Jeronimo J, Massad LS, Schiffman M; National Institutes of Health/American Society for Colposcopy and Cervical Pathology (NIH/ASCCP) Research Group. Visual appearance of the uterine cervix: correlation with human papillomavirus detection and type. Am J Obstet Gynecol. 2007; 197:47.e1–47.e8.
Article22. Nam K, Kwak J, Kim J, Jeon S. Human papillomavirus type 16 causes larger colposcopic lesions than other HPV types in patients with grade 3 cervical intraepithelial neoplasia. J Low Genit Tract Dis. 2013; 17:1–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Colposcopy of Vagina
- New Terminology and Classification of Colposcopy
- Learning curves of total laparoscopic hysterectomies in three gynecologists
- Brain-machine Interface in Robot-assisted Neurorehabilitation for Patients with Stroke and Upper Extremity Weakness – the Therapeutic Turning Point
- Role of Colposcopy in Cervical Cancer, Including Cervicography