J Korean Neurosurg Soc.
2018 Sep;61(5):625-632. 10.3340/jkns.2018.0045.
Analysis According to Characteristics of 18 Cases of Brachial Plexus Tumors : A Review of Surgical Treatment Experience
- Affiliations
-
- 1Department of Neurosurgery, Dankook University College of Medicine, Cheonan, Korea. melway@hanmail.net
- KMID: 2420071
- DOI: http://doi.org/10.3340/jkns.2018.0045
Abstract
OBJECTIVE
Because the anatomical structure of the brachial plexus is very complex, surgical treatment of tumors in this region is challenging. Therefore, a lot of clinical and surgical experience is required for successful treatment; however, many neurosurgeons have difficulty accumulating this experience owing to the rarity of brachial plexus tumors. The purpose of this report is to share our surgical experience with brachial plexus tumor with other neurosurgeons.
METHODS
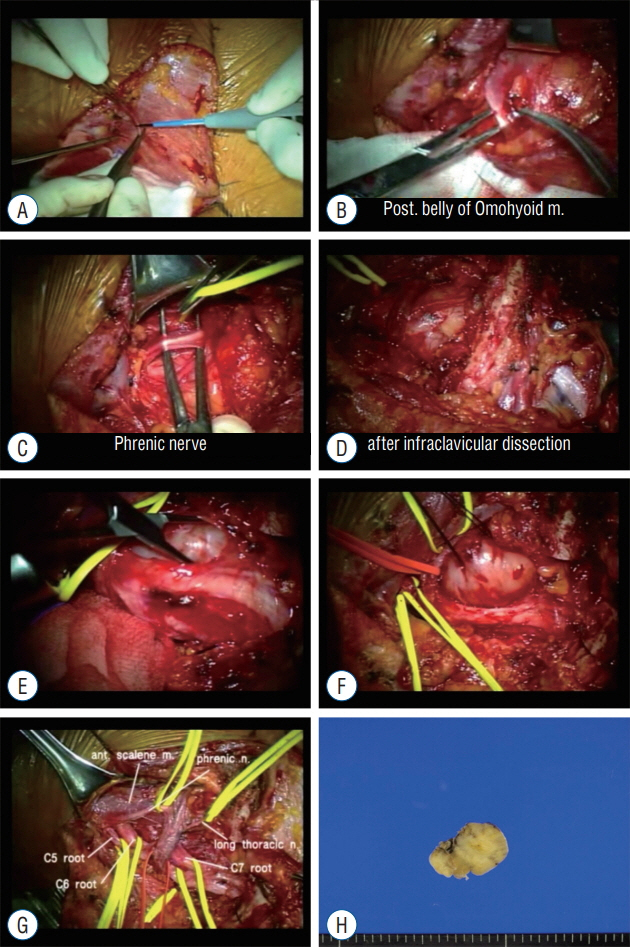
The records of 18 consecutive patients with brachial plexus tumors who underwent surgical treatment between January 2010 and December 2017 in a single institution were retrospectively reviewed. The surgical approach was determined according to the tumor location and size, and intraoperative neurophysiological monitoring (IONM) was used in most of cases to prevent iatrogenic nerve injury during surgery. In addition, to evaluate the differences in tumor characteristics according to pathologic diagnosis, the tumors were divided twice into two groups, based on two separate classifications, and statistical analysis was performed.
RESULTS
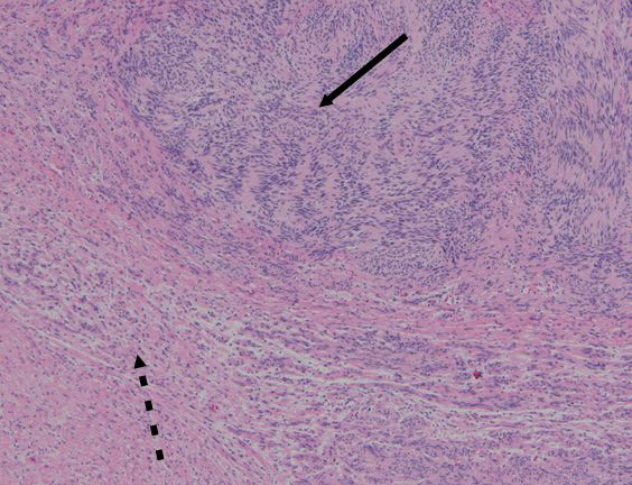
The 18 brachial plexus tumors comprised 15 (83.3%) benign peripheral nerve sheath tumors including schwannoma and neurofibroma, one (5.6%) malignant peripheral nerve sheath tumor, one (5.6%) benign tumor of non-neural sheath origin (neurogenic cyst), and one (5.6%) metastatic tumor (papillary carcinoma). The authors analyzed relationship between tumor size/location and tumor characteristic parameters such as age, size, right-left, and pathology. There were no statistically significant differences except a tendency of bigger tumor size in young age.
CONCLUSION
For a successful surgical outcome, an appropriate surgical approach is essential, and the appropriate surgical approach is determined by the location and size of the tumor. Furthermore, applying IONM may prevent postoperative complications and it is favorable option for brachial plexus tumors surgery.
MeSH Terms
Figure
Reference
-
References
1. Binder DK, Smith JS, Barbaro NM. Primary brachial plexus tumors: imaging, surgical, and pathological findings in 25 patients. Neurosurg Focus. 16:E11. 2004.
Article2. Burger PC, Scheithauer BW, Vogel FS. Surgical pathology of the nervous system and its coverings. ed 4. New York: Churchill Livingstone;2002.3. Crutcher CL 2nd, Kline DG, Tender GC. A modified, less invasive posterior subscapular approach to the brachial plexus: case report and technical note. Neurosurg Focus. 42:E7. 2017.
Article4. Das S, Ganju A, Tiel RL, Kline DG. Tumors of the brachial plexus. Neurosurg Focus. 22:E26. 2007.
Article5. Dubuisson AS, Kline DG, Weinshel SS. Posterior subscapular approach to the brachial plexus. Report of 102 patients. J Neurosurg. 79:319–330. 1993.6. Ellison D, Love S, Chimelli LMC, Harding B, Lowe JS, Vinters HV, et al. Neuropathology E-Book: A Reference Text of CNS Pathology. ed 3. Edinburgh: Mosby Elsevier;2013.7. Ganju A, Roosen N, Kline DG, Tiel RL. Outcomes in a consecutive series of 111 surgically treated plexal tumors: a review of the experience at the Louisiana State University Health Sciences Center. J Neurosurg. 95:51–60. 2001.
Article8. Kim DH, Murovic JA, Tiel RL, Moes G, Kline DG. A series of 146 peripheral non-neural sheath nerve tumors: 30-year experience at Louisiana State University Health Sciences Center. J Neurosurg. 102:256–266. 2005.
Article9. Lwu S, Midha R. Clinical examination of brachial and pelvic plexus tumors. Neurosurg Focus. 22:E5. 2007.
Article10. Tschoe C, Holsapple JW, Binello E. Resection of primary brachial plexus tumor via a modified supraclavicular approach. J Neurol Surg Rep. 75:e133–e135. 2014.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Granular Cell Tumor of Brachial Plexus Mimicking Nerve Sheath Tumor: A Case Report
- A Case of Brachial Plexus Neurofibroma
- Brachial Plexus Injury: Mechanisms, Surgical Treatment and Outcomes
- The Surgical Management of the Brachial Plexus Injuries: Report of 4 Among 7 Cases
- Progressive Brachial Plexus Palsy after Fixation of Clavicle Shaft Nonunion: A Case Report