Ann Rehabil Med.
2018 Aug;42(4):591-600. 10.5535/arm.2018.42.4.591.
The Nutritional Status and the Clinical Outcomes of Patients With a Spinal Cord Injury Using Nutritional Screening Tools
- Affiliations
-
- 1Department of Rehabilitation Medicine and Research Institute of Rehabilitation Medicine, Yonsei University College of Medicine, Seoul, Korea. leegal7@gmail.com
- KMID: 2420052
- DOI: http://doi.org/10.5535/arm.2018.42.4.591
Abstract
OBJECTIVE
To assess the nutritional status of Korean patients with spinal cord injury (SCI), identify the predictors of undernutrition, and investigate the relationship between undernutrition and clinical outcomes.
METHODS
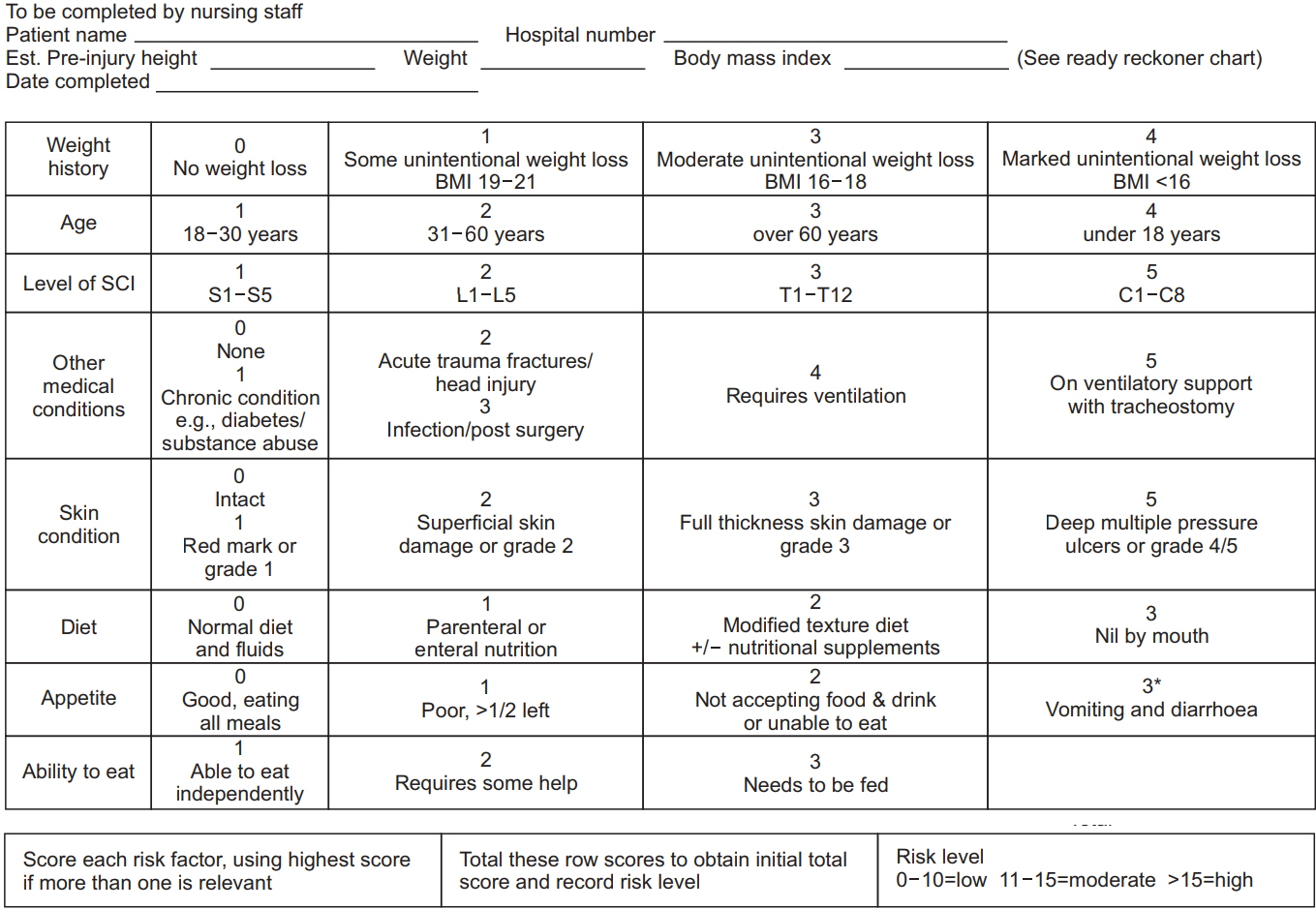
A retrospective study design was used to determine the nutritional status of 130 patients over 19 years old admitted to the rehabilitation hospital of Yonsei University Health System between June 2015 and February 2017. The nutritional status was assessed using the malnutrition universal screening tool (MUST) and the spinal nutrition screening tool (SNST). The relationship between undernutrition and clinical outcomes was examined by comparing a low-risk group with an at-risk group using a t-test.
RESULTS
Among the SCI patients, 70 (50.8%) were confirmed with undernutrition based on the MUST scores, while 60 (46.2%) had undernutrition based on the SNST scores. It was found that undernutrition has an effect on functional outcomes.
CONCLUSION
We assessed the undernutrition risk in Korean SCI patients, and found that approximately 50% of the patients were at risk of undernutrition. We also found that undernutrition can affect functional recovery.
MeSH Terms
Figure
Reference
-
1. Kubrak C, Jensen L. Malnutrition in acute care patients: a narrative review. Int J Nurs Stud. 2007; 44:1036–54.
Article2. Kyle UG, Pirlich M, Schuetz T, Luebke HJ, Lochs H, Pichard C. Prevalence of malnutrition in 1760 patients at hospital admission: a controlled population study of body composition. Clin Nutr. 2003; 22:473–81.
Article3. Wong S, Derry F, Jamous A, Hirani SP, Grimble G, Forbes A. The prevalence of malnutrition in spinal cord injuries patients: a UK multicentre study. Br J Nutr. 2012; 108:918–23.
Article4. Wong S, Derry F, Grimble G, Forbes A. How do spinal cord injury centres manage malnutrition? A crosssectional survey of 12 regional centres in the United Kingdom and Ireland. Spinal Cord. 2012; 50:132–5.
Article5. Naber TH, Schermer T, de Bree A, Nusteling K, Eggink L, Kruimel JW, et al. Prevalence of malnutrition in nonsurgical hospitalized patients and its association with disease complications. Am J Clin Nutr. 1997; 66:1232–9.
Article6. Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003; 22:235–9.7. Castro MJ, Apple DF Jr, Hillegass EA, Dudley GA. Influence of complete spinal cord injury on skeletal muscle cross-sectional area within the first 6 months of injury. Eur J Appl Physiol Occup Physiol. 1999; 80:373–8.
Article8. de Groot S, Post MW, Hoekstra T, Valent LJ, Faber WX, van der Woude LH. Trajectories in the course of body mass index after spinal cord injury. Arch Phys Med Rehabil. 2014; 95:1083–92.
Article9. Cheshire DJ, Coats DA. Respiratory and metabolic management in acute tetraplegia. Paraplegia. 1966; 4:1–23.
Article10. Buchholz AC, Pencharz PB. Energy expenditure in chronic spinal cord injury. Curr Opin Clin Nutr Metab Care. 2004; 7:635–9.
Article11. Guerra RS, Fonseca I, Sousa AS, Jesus A, Pichel F, Amaral TF. ESPEN diagnostic criteria for malnutrition - A validation study in hospitalized patients. Clin Nutr. 2017; 36:1326–32.
Article12. Kondrup J, Allison SP, Elia M, Vellas B, Plauth M; Educational and Clinical Practice Committee, European Society of Parenteral and Enteral Nutrition (ESPEN). ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003; 22:415–21.
Article13. Mueller C, Compher C, Ellen DM; American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Board of Directors. A.S.P.E.N. clinical guidelines: nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enteral Nutr. 2011; 35:16–24.14. Barbosa-Silva MC, Barros AJ. Indications and limitations of the use of subjective global assessment in clinical practice: an update. Curr Opin Clin Nutr Metab Care. 2006; 9:263–9.
Article15. Velasco C, Garcia E, Rodriguez V, Frias L, Garriga R, Alvarez J, et al. Comparison of four nutritional screening tools to detect nutritional risk in hospitalized patients: a multicentre study. Eur J Clin Nutr. 2011; 65:269–74.
Article16. Wong S, Derry F, Jamous A, Hirani SP, Grimble G, Forbes A. Validation of the spinal nutrition screening tool (SNST) in patients with spinal cord injuries (SCI): result from a multicentre study. Eur J Clin Nutr. 2012; 66(3):382–7.
Article17. Stratton RJ, Hackston A, Longmore D, Dixon R, Price S, Stroud M, et al. Malnutrition in hospital outpatients and inpatients: prevalence, concurrent validity and ease of use of the ‘malnutrition universal screening tool’ (‘MUST’) for adults. Br J Nutr. 2004; 92:799–808.
Article18. Chao PC, Chuang HJ, Tsao LY, Chen PY, Hsu CF, Lin HC, et al. The Malnutrition Universal Screening Tool (MUST) and a nutrition education program for high risk cancer patients: strategies to improve dietary intake in cancer patients. Biomedicine (Taipei). 2015; 5:17.
Article19. Bienertova-Vasku J, Novak J, Zlamal F, Forejt M, Havlenova S, Jackowska A, et al. The prediction role of indexes of circulating adipokines for common anthropometric and nutritional characteristics of obesity in the obese Central European population. Eat Behav. 2014; 15:244–51.20. Wong S, Derry F, Jamous A, Hirani SP, Forbes A. Is undernutrition risk associated with an adverse clinical outcome in spinal cord-injured patients admitted to a spinal centre? Eur J Clin Nutr. 2014; 68:125–30.
Article21. Wang YJ, Zhou HJ, Liu PJ, Liu GL, Zheng Y, Wei B, et al. Risks of undernutrition and malnutrition in hospitalized pediatric patients with spinal cord injury. Spinal Cord. 2017; 55:247–54.
Article22. Buzby GP, Mullen JL, Matthews DC, Hobbs CL, Rosato EF. Prognostic nutritional index in gastrointestinal surgery. Am J Surg. 1980; 139:160–7.
Article23. Ingenbleek Y, Carpentier YA. A prognostic inflammatory and nutritional index scoring critically ill patients. Int J Vitam Nutr Res. 1985; 55:91–101.24. Kuzu MA, Terzioglu H, Genc V, Erkek AB, Ozban M, Sonyurek P, et al. Preoperative nutritional risk assessment in predicting postoperative outcome in patients undergoing major surgery. World J Surg. 2006; 30:378–90.
Article25. Wada H, Dohi T, Miyauchi K, Doi S, Naito R, Konishi H, et al. Prognostic Impact of the Geriatric Nutritional Risk Index on Long-Term Outcomes in Patients Who Underwent Percutaneous Coronary Intervention. Am J Cardiol. 2017; 119:1740–5.
Article26. Burr RG, Clift-Peace L, Nuseibeh I. Haemoglobin and albumin as predictors of length of stay of spinal injured patients in a rehabilitation centre. Paraplegia. 1993; 31:473–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nutrition Screening and Assessment of Patients for Malnutrition
- The Importance of Nutrition in Neurological Disorders and Nutrition Assessment Methods
- Current status of nutritional screening in periodic health examination
- Nutritional Screening and Assessment in Hospitalized Patients
- Value of Nutritional Screening Tools Versus Anthropometric Measurements in Evaluating Nutritional Status of Children in a Low/Middle-Income Country