J Korean Orthop Assoc.
2018 Aug;53(4):350-357. 10.4055/jkoa.2018.53.4.350.
Measuring Needle Angle and Depth for Lumbar Medial Branch Block Using Ultrasonography: An Evaluation of Efficiency Compared with Magnetic Resonance Imaging
- Affiliations
-
- 1Department of Orthopedic Surgery, Kosin University Gospel Hospital, Busan, Korea. mewha98@naver.com
- 2Department of Orthopedic Surgery, Wonkwang University School of Medicine, Iksan, Korea.
- 3Department of Orthopedic Surgery, Keimyung University School of Medicine, Daegu, Korea.
- 4Department of Orthopedic Surgery, Bumin Hospital Busan, Busan, Korea.
- KMID: 2419471
- DOI: http://doi.org/10.4055/jkoa.2018.53.4.350
Abstract
- PURPOSE
The purpose of this study was to compare accuracy of proper needle insertion angle between magnetic resonance imaging (MRI) and ultrasonography during lumbar medial branch nerve block procedure.
MATERIALS AND METHODS
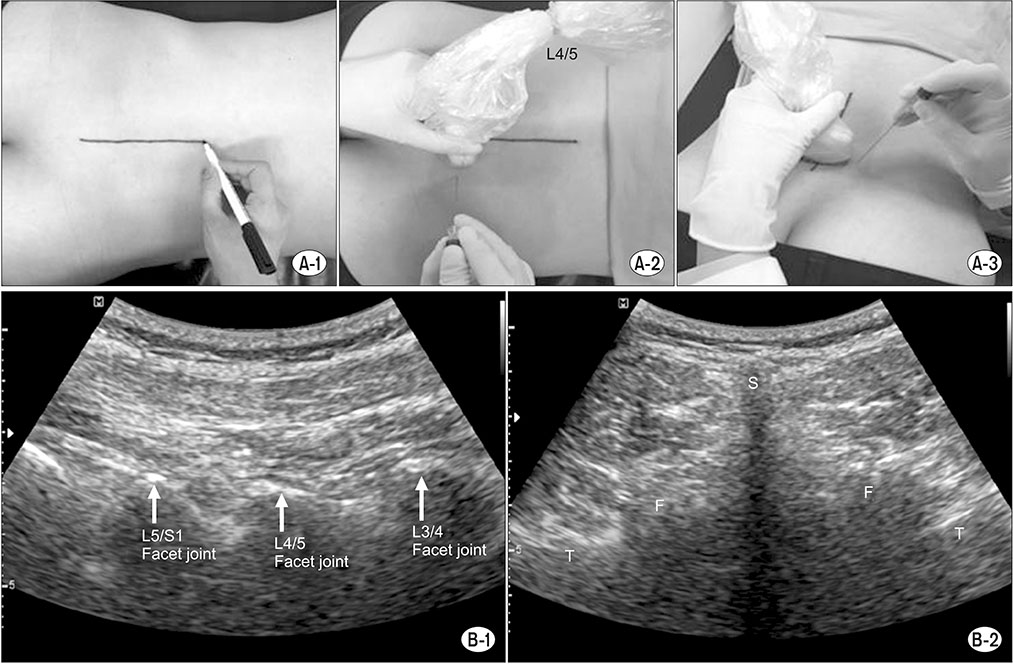
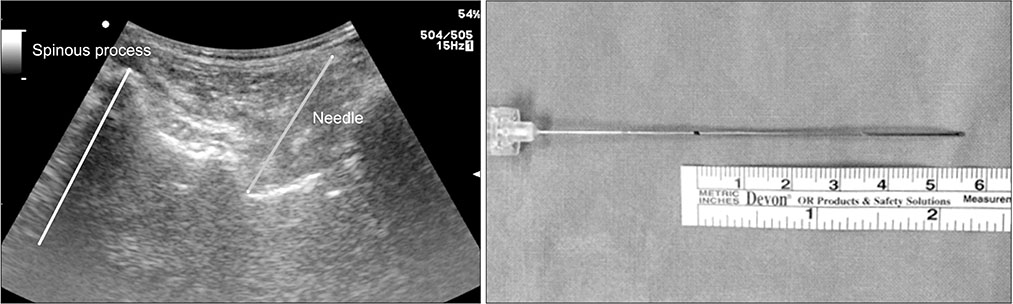
Between January 2015 and June 2016, 80 people who underwent MRI in the past 3 months with improved lumbar pain after sono-guided medial branch nerve block were enrolled for analysis (male, 39; female, 41; average age, 63.3 years). The insertion angle and depth between the spinous process and needle at each target points were measured at various levels (superior, inferior segment of each facet joints from L2-3 to L5-S1). The needle was positioned 1 cm apart from both lateral sides of the probe, locating spinous process in the middle. A comparative analysis was performed between an ultrasonography and an MRI. We determined the statistical correlation between the two methods.
RESULTS
The average differences with respect to the distance between each level on a sono-guided medial branch nerve block were 1.28±1.07 mm in L2 (7 cases), 1.27±4.26 mm in L3 (25 cases), 1.63±5.89 mm in L4 (93 cases), 1.99±4.12 mm in L5 (141 cases), and 1.51±3.87 mm in S1 (66 cases). The average differences regarding the angle of each level were 1.69°±1.34° in L2 (7 cases), 2.03°±5.35° in L3 (25 cases), 1.49°±3.42° in L4 (93 cases), −1.55°±3.67° in L5 (141 cases), and 1.86°±4.83° in S1 (66 cases). All measurements followed a normal distribution (p < 0.05), showing statistical correlation without significant difference (p < 0.05).
CONCLUSION
After measuring each level using an MRI prior to performing the procedure, a sono-guided lumbar medial branch nerve block can be performed with greater safety and efficacy, especially for beginners.
MeSH Terms
Figure
Reference
-
1. Mooney V, Robertson J. The facet syndrome. Clin Orthop Relat Res. 1976; (115):149–156.
Article2. Frymoyer JW. Back pain and sciatica. N Engl J Med. 1988; 318:291–300.
Article3. Bogduk N. International spinal injection society guidelines for the performance of spinal injection procedures. Part 1: zygapophysial joint blocks. Clin J Pain. 1997; 13:285–302.4. Gangi A, Dietemann JL, Mortazavi R, Pfleger D, Kauff C, Roy C. CT-guided interventional procedures for pain management in the lumbosacral spine. Radiographics. 1998; 18:621–633.
Article5. Saal JS. General principles of diagnostic testing as related to painful lumbar spine disorders: a critical appraisal of current diagnostic techniques. Spine (Phila Pa 1976). 2002; 27:2538–2545.6. Saranteas T, Paraskeuopoulos T, Anagnostopoulou S, Kanellopoulos I, Mastoris M, Kostopanagiotou G. Ultrasound anatomy of the cervical paravertebral space: a preliminary study. Surg Radiol Anat. 2010; 32:617–622.
Article7. Ha DH, Shim DM, Kim TK, Kim YM, Choi SS. Comparison of ultrasonography- and fluoroscopy-guided facet joint block in the lumbar spine. Asian Spine J. 2010; 4:15–22.
Article8. Shim JK, Moon JC, Yoon KB, Kim WO, Yoon DM. Ultrasound-guided lumbar medial-branch block: a clinical study with fluoroscopy control. Reg Anesth Pain Med. 2006; 31:451–454.
Article9. Pedersen HE, Blunck CF, Gardner E. The anatomy of lumbosacral posterior rami and meningeal branches of spinal nerve (sinu-vertebral nerves); with an experimental study of their functions. J Bone Joint Surg Am. 1956; 38:377–391.10. Hirsch C, Ingelmark BE, Miller M. The anatomical basis for low back pain. Studies on the presence of sensory nerve endings in ligamentous, capsular and intervertebral disc structures in the human lumbar spine. Acta Orthop Scand. 1963; 33:1–17.
Article11. Kellgren JH. Referred pains from muscle. Br Med J. 1938; 1:325–327.
Article12. Mooney V. The syndromes of low back disease. Orthop Clin North Am. 1983; 14:505–515.
Article13. Rees WS. Rhysolysis of the nerves of the zygoapophyseal joints. Spine (Phila Pa 1976). 1983; 8:118–120.14. Shealy CN. Facet denervation in the management of back and sciatic pain. Clin Orthop Relat Res. 1976; 115:157–164.
Article15. Silvers HR. Lumbar percutaneous facet rhizotomy. Spine (Phila Pa 1976). 1990; 15:36–40.
Article16. Alhelail M, Al-Salamah M, Al-Mulhim M, Al-Hamid S. Comparison of bupivacaine and lidocaine with epinephrine for digital nerve blocks. Emerg Med J. 2009; 26:347–350.
Article17. Birkenmaier C, Veihelmann A, Trouillier HH, Hausdorf J, von Schulze Pellengahr C. Medial branch blocks versus pericapsular blocks in selecting patients for percutaneous cryodenervation of lumbar facet joints. Reg Anesth Pain Med. 2007; 32:27–33.
Article18. Jeon CH, Lee WI, Kang SY. Intra and extraspinal infected synovial cyst of the lumbar spine: case report. J Korean Soc Spine Surg. 1997; 4:357–364.19. Moon SH, Lee S, Kim KH, et al. Effect of ultrasound-guided lumbar medial branch block in chronic low back pain. J Korean Orthop Res Soc. 2012; 15:54–61.20. Greher M, Scharbert G, Kamolz LP, et al. Ultrasound-guided lumbar facet nerve block: a sonoanatomic study of a new methodologic approach. Anesthesiology. 2004; 100:1242–1248.21. Galiano K, Obwegeser AA, Walch C, Schatzer R, Ploner F, Gruber H. Ultrasound-guided versus computed tomography-controlled facet joint injections in the lumbar spine: a prospective randomized clinical trial. Reg Anesth Pain Med. 2007; 32:317–322.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-guided Distance Measurements of Vertebral Structures for Lumbar Medial Branch Block
- Phantom Study of a New Laser-Etched Needle for Improving Visibility During Ultrasonography-Guided Lumbar Medial Branch Access With Novices
- Ultrasonography for lumbar neuraxial block
- Transverse Process and Needles of Medial Branch Block to Facet Joint as Landmarks for Ultrasound-Guided Selective Nerve Root Block
- Relationship between needle depth for lumbar transforaminal epidural injection and patients’ height and weight using magnetic resonance imaging