J Korean Orthop Assoc.
2018 Aug;53(4):341-349. 10.4055/jkoa.2018.53.4.341.
The Influence of Initial Magnetic Resonance Imaging Findings on the Compression Rate of Thoracolumbar Osteoporotic Vertebral Compression Fracture
- Affiliations
-
- 1Department of Orthopedic Surgery, Sung-Ae Hospital, Seoul, Korea. arcseo@hanmail.net
- KMID: 2419470
- DOI: http://doi.org/10.4055/jkoa.2018.53.4.341
Abstract
- PURPOSE
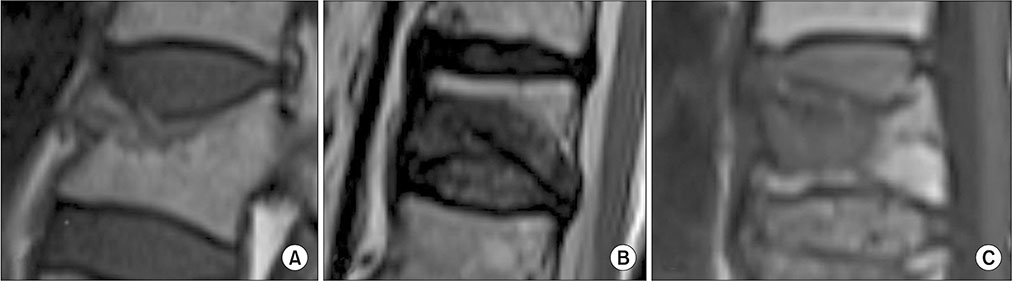
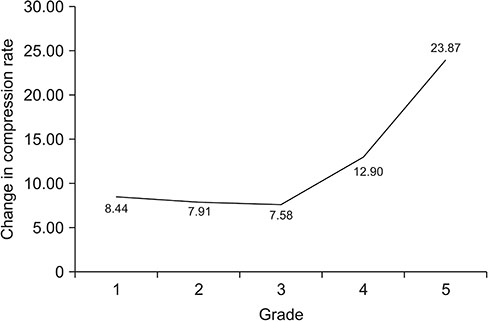
To investigate the influence of the size of low intensity zone (LIZ) (T1 image) on the vertebral body and the increase in the compression rate in patients with osteoporotic vertebral compression fracture.
MATERIALS AND METHODS
In a retrospective study, 187 patients (198 segments) who were followed-up for at least 3 months and diagnosed with thoracolumbar vertebral compression fracture between October 2011 and October 2016, and treated with conservative therapies, such as bed rest and thoraco-lumbar-sacral orthosis. We measured the size of the vertebral LIZ, and fractures on the upper and lower endplates were observed on the initial magnetic resonance imaging. We analyzed the correlation with the increase in compression rate at the last follow-up. Comparisons of the increase in the compression rate were analyzed through a correlation analysis.
RESULTS
The larger the size of the LIZ the greater the difference in the increase of the compression rate. The group with the initially LIZ (80%-100%) was significantly increased to 23.87%±17.90% (p=0.007). In case of fracture of upper and lower endplates, an increase in the compression rate was 19.39%±12.59% in the upper endplate fracture, which was significantly higher than that in the absence of endplate fracture (p=0.002).
CONCLUSION
The larger the size of the LIZ (T1 image) and superior endplate fracture observed on the initial magnetic resonance imaging after fracture, the greater the increase in the compression rate. In particular, when the size of the LIZ is greater than 80%, the compression rate was significantly increased.
Keyword
MeSH Terms
Figure
Reference
-
1. Melton LJ 3rd. Epidemiology of spinal osteoporosis. Spine (Phila Pa 1976). 1997; 22:2S–11S.
Article2. Francis RM, Aspray TJ, Hide G, Sutcliffe AM, Wilkinson P. Back pain in osteoporotic vertebral fractures. Osteoporos Int. 2008; 19:895–903.
Article3. Ehsanbakhsh AR, Akhbari H, Iraee MB, et al. The prevalence of undetected vertebral fracture in patients with back pain by dual-energy X-ray absorptiometry (DXA) of the lateral thoracic and lumbar spine. Asian Spine J. 2011; 5:139–145.
Article4. Prather H, Watson JO, Gilula LA. Nonoperative management of osteoporotic vertebral compression fractures. Injury. 2007; 38:Suppl 3. S40–S48.
Article5. Sugita M, Watanabe N, Mikami Y, Hase H, Kubo T. Classification of vertebral compression fractures in the osteoporotic spine. J Spinal Disord Tech. 2005; 18:376–381.
Article6. Eastell R, Cedel SL, Wahner HW, Riggs BL, Melton LJ 3rd. Classification of vertebral fractures. J Bone Miner Res. 1991; 6:207–215.
Article7. Koh YD, Yoon JS, Hwang JY, Park HS. The relationship between progression of body collapse and MRI findings in osteoporotic stable thoracolumbar fractures. J Korean Fract Soc. 2008; 21:304–311.
Article8. Lau E, Ong K, Kurtz S, Schmier J, Edidin A. Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am. 2008; 90:1479–1486.
Article9. Bengnér U, Johnell O, Redlund-Johnell I. Changes in incidence and prevalence of vertebral fractures during 30 years. Calcif Tissue Int. 1988; 42:293–296.
Article10. Park JH, Kang KC, Shin DE, Koh YG, Son JS, Kim BH. Preventive effects of conservative treatment with short-term teriparatide on the progression of vertebral body collapse after osteoporotic vertebral compression fracture. Osteoporos Int. 2014; 25:613–618.
Article11. Sohn JM, Kim KW, Ha KY, Ha NK, Kim YH, Kim JH. Risk factors for the progressive osteoporotic spinal fracture. J Korean Soc Spine Surg. 2009; 16:153–159.
Article12. Kim WJ, Kang JW, Park KY, Park JG, Jung SH, Choy WS. Clinical outcome of conservative treatment for osteoporotic compression fractures in thoracolumbar junction. J Korean Soc Spine Surg. 2006; 13:240–246.
Article13. Koh YD, Kim JO. Risk factors in progression of deformity in compression fracture of thoracolumbar junction. J Korean Soc Fract. 1999; 12:372–378.
Article14. Jun DS, Shin WJ, An BK, Paik JW, Park MH. The relationship between the progression of kyphosis in stable thoracolumbar fractures and magnetic resonance imaging findings. Asian Spine J. 2015; 9:170–177.
Article15. Theodorou DJ. The intravertebral vacuum cleft sign. Radiology. 2001; 221:787–788.
Article16. Ratcliffe JF. The arterial anatomy of the adult human lumbar vertebral body: a microarteriographic study. J Anat. 1980; 131:57–79.17. Bhalla S, Reinus WR. The linear intravertebral vacuum: a sign of benign vertebral collapse. AJR Am J Roentgenol. 1998; 170:1563–1569.
Article18. Mosekilde L. Normal age-related changes in bone mass, structure, and strength: consequences of the remodelling process. Dan Med Bull. 1993; 40:65–83.19. Mosekilde L. The effect of modelling and remodelling on human vertebral body architecture. Technol Health Care. 1998; 6:287–297.
Article20. D'Ippolito G, Schiller PC, Ricordi C, Roos BA, Howard GA. Age-related osteogenic potential of mesenchymal stromal stem cells from human vertebral bone marrow. J Bone Miner Res. 1999; 14:1115–1122.21. Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology. 1978; 129:23–29.
Article22. Sarli M, Pérez Manghi FC, Gallo R, Zanchetta JR. The vacuum cleft sign: an uncommon radiological sign. Osteoporos Int. 2005; 16:1210–1214.
Article23. Wu AM, Chi YL, Ni WF. Vertebral compression fracture with intravertebral vacuum cleft sign: pathogenesis, image, and surgical intervention. Asian Spine J. 2013; 7:148–155.
Article24. Pfeifer M, Begerow B, Minne HW. Effects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2004; 83:177–186.25. Koh YD, Park JS. Progression of compression and related factors in conservative management of osteoporotic vertebral compression fractures. J Korean Fract Soc. 2015; 28:132–138.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Factors between the Progression of the Compression Rate and Magnetic Resonance Imaging Findings in Osteoporotic Vertebral Fracture Patients Treated with Teriparatide
- Influence of Compression Ratio Differences between Magnetic Resonance Images and Simple Radiographs on Osteoporotic Vertebral Compression Fracture Prognosis after Vertebroplasty
- Correlation between Progression of Compression and Bone Densiometry Index in Osteoporotic Compression Fracture of Thoracolumbar Spine
- Intraspinal Extradural Cyst Subsequent to a Vertebral Compression Fracture - A Case Report -
- Relationship between the Progression of Kyphosis in Thoracolumbar Osteoporotic Vertebral Compression Fractures and Magnetic Resonance Imaging Findings