World J Mens Health.
2018 Sep;36(3):239-247. 10.5534/wjmh.180014.
Abnormal Human Sperm Parameters Contribute to Sperm DNA Fragmentation in Men with Varicocele
- Affiliations
-
- 1Laboratory of Reproductive Medicine, Cheil General Hospital and Women's Healthcare Center, Dankook University College of Medicine, Seoul, Korea.
- 2Department of Urology, Cheil General Hospital and Women's Healthcare Center, Dankook University College of Medicine, Seoul, Korea. jtandro@cgh.co.kr
- 3Division of Developmental Biology and Physiology, School of Biosciences and Chemistry, Sungshin Women's University, Seoul, Korea.
- KMID: 2419324
- DOI: http://doi.org/10.5534/wjmh.180014
Abstract
- PURPOSE
This study was performed to evaluate and compare threshold sperm parameters and sperm DNA fragmentation index (DFI), and further analyzed whether sperm DFI could be predicted from sperm parameters in men with varicocele.
MATERIALS AND METHODS
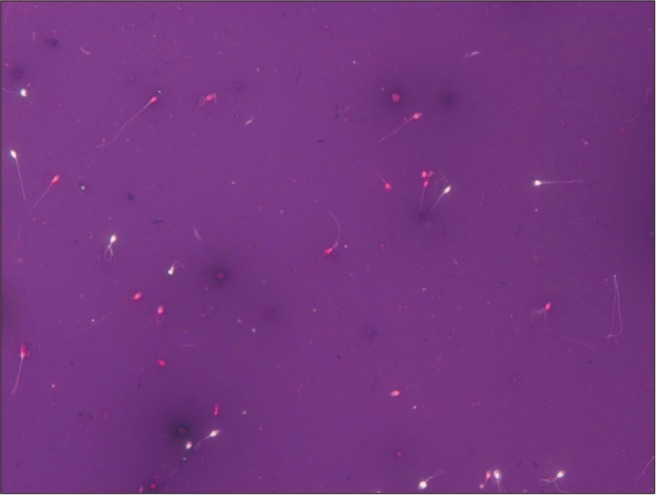
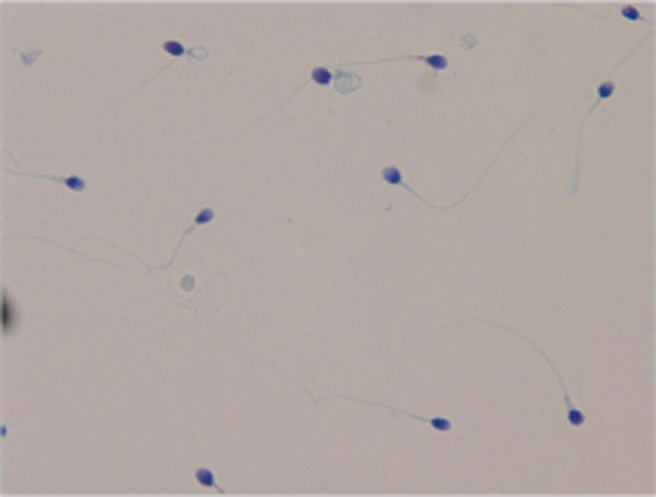
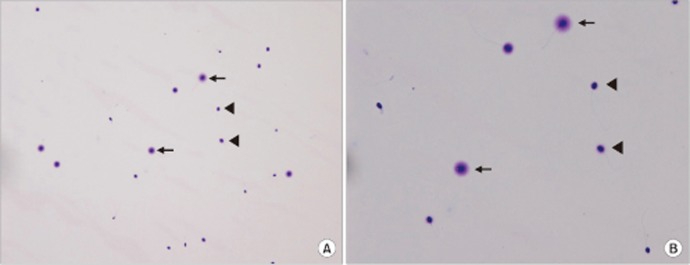
A total of 157 semen samples underwent both semen analysis and sperm DNA fragmentation (SDF) testing in men with varicocele. Sperm parameters were assessed using the World Health Organization guidelines. SDF testing was performed using the Halosperm kit. Sperm parameters and sperm DFI results were compared.
RESULTS
The overall sperm parameter results and sperm DFI showed normal values; however, the morphology value was at the lower limit of normal. High sperm DFI was associated with significantly lower motility and viability (p < 0.001, respectively). Sperm motility and morphology were significantly higher in the higher sperm count group compared to the lower sperm count group (p < 0.05), while sperm DFI was higher in the lower sperm count group (p < 0.05). Sperm count and viability and sperm DFI were significantly associated with the quality of sperm motility (p < 0.001). Sperm motility and sperm DFI were significantly different (p < 0.001) between normal and abnormal sperm viability groups. Between normal and abnormal sperm morphology groups, sperm count, motility, and sperm DFI showed significant differences (p < 0.001).
CONCLUSIONS
In this study, a correlation between SDF and sperm parameters was confirmed in men with varicocele. SDF may be contributing factors to sperm motility, viability, and morphology. Abnormal sperm count, motility, and viability showed high sperm DFI. Therefore, lower sperm parameters were indicative of increasing SDF in men with varicocele.
Keyword
MeSH Terms
Figure
Reference
-
1. Kohn TP, Kohn JR, Pastuszak AW. Varicocelectomy before assisted reproductive technology: are outcomes improved? Fertil Steril. 2017; 108:385–391. PMID: 28865536.
Article2. Gat Y, Bachar GN, Zukerman Z, Belenky A, Gornish M. Varicocele: a bilateral disease. Fertil Steril. 2004; 81:424–429. PMID: 14967384.
Article3. Dieamant F, Petersen CG, Mauri AL, Conmar V, Mattila M, Vagnini LD, et al. Semen parameters in men with varicocele: DNA fragmentation, chromatin packaging, mitochondrial membrane potential, and apoptosis. JBRA Assist Reprod. 2017; 21:295–301. PMID: 29068181.
Article4. World Health Organization. The influence of varicocele on parameters of fertility in a large group of men presenting to infertility clinics. Fertil Steril. 1992; 57:1289–1293. PMID: 1601152.5. Grober ED, O'brien J, Jarvi KA, Zini A. Preservation of testicular arteries during subinguinal microsurgical varicocelectomy: clinical considerations. J Androl. 2004; 25:740–743. PMID: 15292104.
Article6. Madgar I, Weissenberg R, Lunenfeld B, Karasik A, Goldwasser B. Controlled trial of high spermatic vein ligation for varicocele in infertile men. Fertil Steril. 1995; 63:120–124. PMID: 7805900.7. Onozawa M, Endo F, Suetomi T, Takeshima H, Akaza H. Clinical study of varicocele: statistical analysis and the results of long-term follow-up. Int J Urol. 2002; 9:455–461. PMID: 12225343.
Article8. Kamischke A, Nieschlag E. Varicocele treatment in the light of evidence-based andrology. Hum Reprod Update. 2001; 7:65–69. PMID: 11212077.
Article9. Zini A, Blumenfeld A, Libman J, Willis J. Beneficial effect of microsurgical varicocelectomy on human sperm DNA integrity. Hum Reprod. 2005; 20:1018–1021. PMID: 15608026.
Article10. Zini A, Kamal K, Phang D, Willis J, Jarvi K. Biologic variability of sperm DNA denaturation in infertile men. Urology. 2001; 58:258–261. PMID: 11489713.
Article11. Wu GJ, Chang FW, Lee SS, Cheng YY, Chen CH, Chen IC. Apoptosis-related phenotype of ejaculated spermatozoa in patients with varicocele. Fertil Steril. 2009; 91:831–837. PMID: 18314115.
Article12. García-Peiró A, Oliver-Bonet M, Navarro J, Abad C, Amengual MJ, López-Fernández C, et al. Differential clustering of sperm subpopulations in infertile males with clinical varicocele and carriers of rearranged genomes. J Androl. 2012; 33:361–367. PMID: 21835912.13. Esbert M, Pacheco A, Vidal F, Florensa M, Riqueros M, Ballesteros A, et al. Impact of sperm DNA fragmentation on the outcome of IVF with own or donated oocytes. Reprod Biomed Online. 2011; 23:704–710. PMID: 22019617.
Article14. Kruger TF, Acosta AA, Simmons KF, Swanson RJ, Matta JF, Oehninger S. Predictive value of abnormal sperm morphology in in vitro fertilization. Fertil Steril. 1988; 49:112–117. PMID: 3335257.
Article15. Brahem S, Jellad S, Ibala S, Saad A, Mehdi M. DNA fragmentation status in patients with necrozoospermia. Syst Biol Reprod Med. 2012; 58:319–323. PMID: 22871031.
Article16. World Health Organization. WHO laboratory manual for the examination and processing of human semen. 5th ed. Geneva: WHO;2010.17. Chohan KR, Griffin JT, Lafromboise M, De Jonge CJ, Carrell DT. Comparison of chromatin assays for DNA fragmentation evaluation in human sperm. J Androl. 2006; 27:53–59. PMID: 16400078.
Article18. Henkel R, Hajimohammad M, Stalf T, Hoogendijk C, Mehnert C, Menkveld R, et al. Influence of deoxyribonucleic acid damage on fertilization and pregnancy. Fertil Steril. 2004; 81:965–972. PMID: 15066449.
Article19. Dar S, Grover SA, Moskovtsev SI, Swanson S, Baratz A, Librach CL. In vitro fertilization-intracytoplasmic sperm injection outcome in patients with a markedly high DNA fragmentation index (>50%). Fertil Steril. 2013; 100:75–80. PMID: 23562046.20. Wang YJ, Zhang RQ, Lin YJ, Zhang RG, Zhang WL. Relationship between varicocele and sperm DNA damage and the effect of varicocele repair: a meta-analysis. Reprod Biomed Online. 2012; 25:307–314. PMID: 22809864.
Article21. Nasr Esfahani MH, Tavalaee M. Origin and role of DNA damage in varicocele. Int J Fertil Steril. 2012; 6:141–146. PMID: 24520431.22. Nasr-Esfahani MH, Abasi H, Razavi S, Ashrafi S, Tavalaee M. Varicocelectomy: semen parameters and protamine deficiency. Int J Androl. 2009; 32:115–122. PMID: 17971166.
Article23. Enciso M, Muriel L, Fernández JL, Goyanes V, Segrelles E, Marcos M, et al. Infertile men with varicocele show a high relative proportion of sperm cells with intense nuclear damage level, evidenced by the sperm chromatin dispersion test. J Androl. 2006; 27:106–111. PMID: 16400086.
Article24. Talebi AR, Moein MR, Tabibnejad N, Ghasemzadeh J. Effect of varicocele on chromatin condensation and DNA integrityof ejaculated spermatozoa using cytochemical tests. Andrologia. 2008; 40:245–251. PMID: 18727735.25. Evenson DP, Jost LK, Marshall D, Zinaman MJ, Clegg E, Purvis K, et al. Utility of the sperm chromatin structure assay as a diagnostic and prognostic tool in the human fertility clinic. Hum Reprod. 1999; 14:1039–1049. PMID: 10221239.
Article26. Sotolongo B, Huang TT, Isenberger E, Ward WS. An endogenous nuclease in hamster, mouse, and human spermatozoa cleaves DNA into loop-sized fragments. J Androl. 2005; 26:272–280. PMID: 15713834.
Article27. Fernández JL, Muriel L, Rivero MT, Goyanes V, Vazquez R, Alvarez JG. The sperm chromatin dispersion test: a simple method for the determination of sperm DNA fragmentation. J Androl. 2003; 24:59–66. PMID: 12514084.28. Fernández JL, Muriel L, Goyanes V, Segrelles E, Gosálvez J, Enciso M, et al. Simple determination of human sperm DNA fragmentation with an improved sperm chromatin dispersion test. Fertil Steril. 2005; 84:833–842. PMID: 16213830.29. Sellami A, Chakroun N, Ben Zarrouk S, Sellami H, Kebaili S, Rebai T, et al. Assessment of chromatin maturity in human spermatozoa: useful aniline blue assay for routine diagnosis of male infertility. Adv Urol. 2013; DOI: 10.1155/2013/578631.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Microsurgical Varicocelectomy on Human Sperm Nucleus DNA Integrity
- Correlations between abnormalities of morphological details and DNA fragmentation in human sperm
- Sperm DNA Fragmentation and Standard Semen Parameters in Algerian Infertile Male Partners
- What should be done for men with sperm DNA fragmentation?
- Standard Semen Parameters vs. Sperm Kinematics to Predict Sperm DNA Damage