Ann Dermatol.
2018 Jun;30(3):342-344. 10.5021/ad.2018.30.3.342.
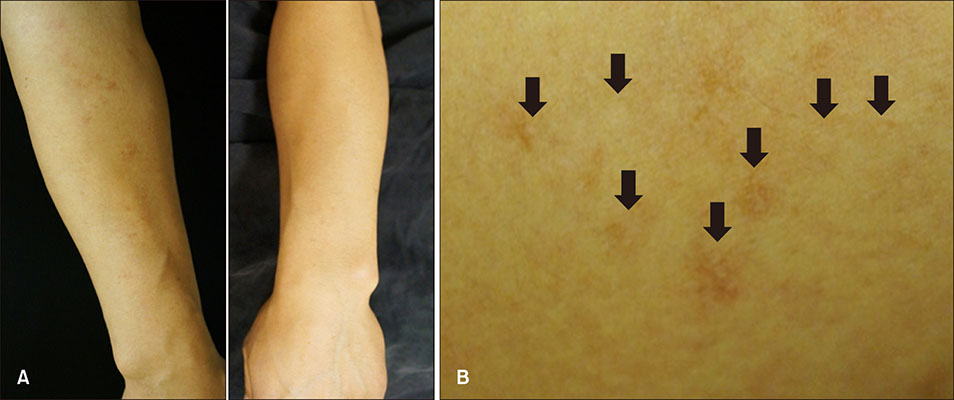
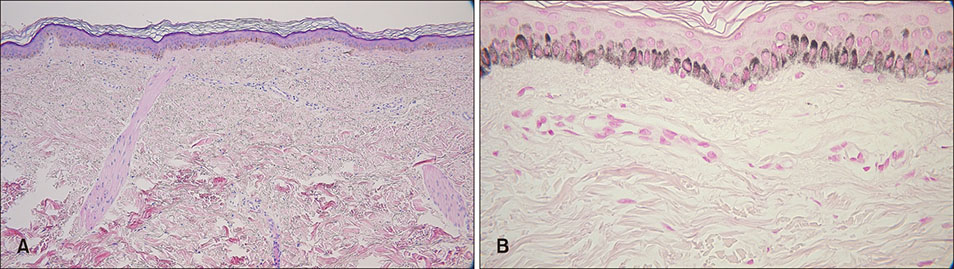
Acquired Brachial Cutaneous Dyschromatosis in a Middle Aged Male
- Affiliations
-
- 1Department of Dermatology, Ewha Womans University School of Medicine, Seoul, Korea. uwon313@ewha.ac.kr
- KMID: 2419177
- DOI: http://doi.org/10.5021/ad.2018.30.3.342
Abstract
- Acquired brachial cutaneous dyschromatosis (ABCD) is an acquired disorder of pigmentary change that presents as chronic, asymptomatic, geographic-shaped, gray-brown patches, consisting of mixed hyper and hypopigmented macules on the dorsal aspect of the forearms. We report a case of a 40-year-old male who presented with asymptomatic, multiple brown-colored macules on the outer aspects of both arms. He had no history of hypertension and had never taken angiotensin converting enzyme inhibitors. He also denied chronic sun exposure history. Histologic examination demonstrated epidermal atrophy, increased basal layer pigmentation, and several telangiectatic vessels in the upper dermis. Solar elastosis was not remarkable. The patient's clinical and histopathologic features were consistent with a diagnosis of ABCD. Poikiloderma of Civatte, melasma, acquired bilateral telangiectatic macules and other pigmentary disorders should be considered in the differential diagnosis of ABCD. Herein, we report a case of ABCD in a middle-aged male without hypertension and medication.
MeSH Terms
Figure
Reference
-
1. Rongioletti F, Rebora A. Acquired brachial cutaneous dyschromatosis: a common pigmentary disorder of the arm in middle-aged women. J Am Acad Dermatol. 2000; 42:680–684.
Article2. Abidi N, Foering K, Sahu J. Acquired brachial cutaneous dyschromatosis in a 60-year-old male: a case report and review of the literature. Case Rep Dermatol Med. 2014; 2014:452720.
Article3. Hu SW, Chu J, Meehan S, Kamino H, Pomeranz MK. Acquired brachial cutaneous dyschromatosis. Dermatol Online J. 2011; 17:16.
Article4. Costa DLM, Moura HH, Rodrigues R, Pineiro-Maceira J, Ramos-e-Silva M. Telangiectasia macularis eruptive perstans. J Clin Aesthet Dermatol. 2011; 4:52–54.5. Park JH, Lee DJ, Lee YJ, Jang YH, Kang HY, Kim YC. Acquired bilateral telangiectatic macules: a distinct clinical entity. JAMA Dermatol. 2014; 150:974–977.6. Bhutani LK, Bedi TR, Pandhi RK, Nayak NC. Lichen planus pigmentosus. Dermatologica. 1974; 149:43–50.
Article7. Dereure O. Drug-induced skin pigmentation. Epidemiology, diagnosis and treatment. Am J Clin Dermatol. 2001; 2:253–262.8. Song HS, Kang HY. Imatinib mesylate-induced hyperpigmentation of the nose and palate. Ann Dermatol. 2014; 26:532–533.
Article