Yonsei Med J.
2017 Jul;58(4):793-799. 10.3349/ymj.2017.58.4.793.
Administration of a High-Dose Erythropoietin-Stimulating Agent in Hemodialysis Patients is Associated with Late Arteriovenous Fistula Failure
- Affiliations
-
- 1Division of Nephrology, Department of Internal Medicine, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea. ysy0119@cha.ac.kr, dhyang@cha.ac.kr
- 2Division of Cardiology, Department of Internal Medicine, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea.
- KMID: 2419086
- DOI: http://doi.org/10.3349/ymj.2017.58.4.793
Abstract
- PURPOSE
Investigating the risk of vascular access failure is critical for maintenance hemodialysis (MHD) patients. Erythropoietin stimulating agents (ESA) typically used for anemia of chronic kidney disease (CKD) may also stimulate neointimal hyperplasia, which is the most important factor in late arteriovenous fistula (AVF) failure. The aim of this study was to investigate whether ESA treatment is associated with late AVF failure.
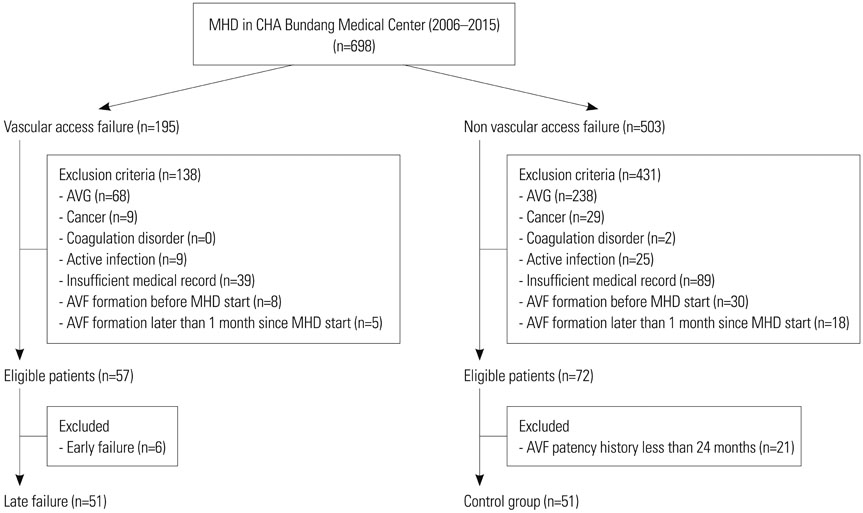
MATERIALS AND METHODS
The late AVF failure group comprised 51 patients who underwent percutaneous intervention or surgery for fistula revision after successful use for at least three months. There were 51 controls whose AVF had been patent for at least 24 months.
RESULTS
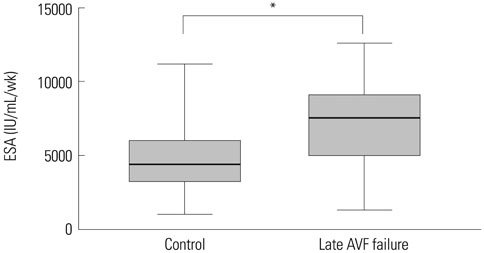
The mean time from the first cannulation to late loss of AVF patency was 8.4±4.2 months. The average weekly dose of ESA was significantly higher in patients with AVF failure (4782.2±2360.5 IU/mL/wk vs. 7161.8±2775.2 IU/mL/wk, p<0.001). The only independent predictor of late AVF failure in multivariate analysis was high average ESA dose (odds ratio=1.015, 95% confidence interval=1.002-1.028, p=0.022).
CONCLUSION
Patients with late AVF patency loss exhibit an association with a higher dose of ESA, although causality is unproven. Further study to elucidate potential mechanisms is warranted.
Keyword
MeSH Terms
Figure
Reference
-
1. Leermakers JJ, Bode AS, Vaidya A, van der Sande FM, Evers SM, Tordoir JH. Cost-effectiveness of vascular access for haemodialysis: arteriovenous fistulas versus arteriovenous grafts. Eur J Vasc Endovasc Surg. 2013; 45:84–92.
Article2. Rosas SE, Feldman HI. Synthetic vascular hemodialysis access versus native arteriovenous fistula: a cost-utility analysis. Ann Surg. 2012; 255:181–186.
Article3. Roy-Chaudhury P, Sukhatme VP, Cheung AK. Hemodialysis vascular access dysfunction: a cellular and molecular viewpoint. J Am Soc Nephrol. 2006; 17:1112–1127.
Article4. Beathard GA. Failure of the mature hemodialysis arteriovenous fistula. accessed on 2017 February 3. Available at: http://www.uptodate.com/contents/failure-of-the-mature-hemodialysis-arteriovenous-fistula.5. Lu FP, Liu LP, Lu ZX. One-year patency rate of native arteriovenous fistulas reconstructed by vascular stripping in hemodialysis patients with venous neointimal hyperplasia. J Vasc Surg. 2015; 61:192–196.
Article6. Liang A, Wang Y, Han G, Truong L, Cheng J. Chronic kidney disease accelerates endothelial barrier dysfunction in a mouse model of an arteriovenous fistula. Am J Physiol Renal Physiol. 2013; 304:F1413–F1420.
Article7. Babitt JL, Lin HY. Mechanisms of anemia in CKD. J Am Soc Nephrol. 2012; 23:1631–1634.
Article8. Akimoto T, Kusano E, Fujita N, Okada K, Saito O, Ono S, et al. Erythropoietin modulates angiotensin II- or noradrenaline-induced Ca(2+) mobilization in cultured rat vascular smooth-muscle cells. Nephrol Dial Transplant. 2001; 16:491–499.
Article9. Janmaat ML, Heerkens JL, de Bruin AM, Klous A, de Waard V, de Vries CJ. Erythropoietin accelerates smooth muscle cell-rich vascular lesion formation in mice through endothelial cell activation involving enhanced PDGF-BB release. Blood. 2010; 115:1453–1460.
Article10. De Marchi S, Cecchin E, Falleti E, Giacomello R, Stel G, Sepiacci G, et al. Long-term effects of erythropoietin therapy on fistula stenosis and plasma concentrations of PDGF and MCP-1 in hemodialysis patients. J Am Soc Nephrol. 1997; 8:1147–1156.
Article11. Aljama P, Bommer J, Canaud B, Carrera F, Eckardt KU, Hörl WH, et al. Practical guidelines for the use of NESP in treating renal anaemia. Nephrol Dial Transplant. 2001; 16:Suppl 3. 22–28.12. Locatelli F, Andrulli S, Memoli B, Maffei C, Del Vecchio L, Aterini S, et al. Nutritional-inflammation status and resistance to erythropoietin therapy in haemodialysis patients. Nephrol Dial Transplant. 2006; 21:991–998.
Article13. Agarwal R, Davis JL, Smith L. Serum albumin is strongly associated with erythropoietin sensitivity in hemodialysis patients. Clin J Am Soc Nephrol. 2008; 3:98–104.
Article14. Salmela B, Hartman J, Peltonen S, Albäck A, Lassila R. Thrombophilia and arteriovenous fistula survival in ESRD. Clin J Am Soc Nephrol. 2013; 8:962–968.
Article15. Sedlacek M, Teodorescu V, Falk A, Vassalotti JA, Uribarri J. Hemodialysis access placement with preoperative noninvasive vascular mapping: comparison between patients with and without diabetes. Am J Kidney Dis. 2001; 38:560–564.
Article16. Allon M, Litovsky S, Young CJ, Deierhoi MH, Goodman J, Hanaway M, et al. Medial fibrosis, vascular calcification, intimal hyperplasia, and arteriovenous fistula maturation. Am J Kidney Dis. 2011; 58:437–443.
Article17. Bashar K, Conlon PJ, Kheirelseid EA, Aherne T, Walsh SR, Leahy A. Arteriovenous fistula in dialysis patients: factors implicated in early and late AVF maturation failure. Surgeon. 2016; 14:294–300.
Article18. Grandaliano G, Teutonico A, Allegretti A, Losappio R, Mancini A, Gesualdo L, et al. The role of hyperparathyroidism, erythropoietin therapy, and CMV infection in the failure of arteriovenous fistula in hemodialysis. Kidney Int. 2003; 64:715–719.
Article19. Roozbeh J, Serati AR, Malekhoseini SA. Arteriovenous fistula thrombosis in patients on regular hemodialysis: a report of 171 patients. Arch Iran Med. 2006; 9:26–32.20. Ammarguellat F, Gogusev J, Drüeke TB. Direct effect of erythropoietin on rat vascular smooth-muscle cell via a putative erythropoietin receptor. Nephrol Dial Transplant. 1996; 11:687–692.
Article21. Skali H, Parving HH, Parfrey PS, Burdmann EA, Lewis EF, Ivanovich P, et al. Stroke in patients with type 2 diabetes mellitus, chronic kidney disease, and anemia treated with Darbepoetin Alfa: the trial to reduce cardiovascular events with Aranesp therapy (TREAT) experience. Circulation. 2011; 124:2903–2908.
Article22. Jelkmann W, Gross AJ. Erythropoietin. New York: Springer-Verlag Berlin Heidelberg;1989. p. 139–145.23. Irish A, Dogra G, Mori T, Beller E, Heritier S, Hawley C, et al. Preventing AVF thrombosis: the rationale and design of the Omega-3 fatty acids (Fish Oils) and Aspirin in Vascular access OUtcomes in REnal Disease (FAVOURED) study. BMC Nephrol. 2009; 10:1.
Article24. Unger EF, Thompson AM, Blank MJ, Temple R. Erythropoiesis-stimulating agents--time for a reevaluation. N Engl J Med. 2010; 362:189–192.
Article25. Malyszko J, Malyszko JS, Borawski J, Rydzewski A, Kalinowski M, Azzadin A, et al. A study of platelet functions, some hemostatic and fibrinolytic parameters in relation to serotonin in hemodialyzed patients under erythropoietin therapy. Thromb Res. 1995; 77:133–143.
Article26. Kooistra MP, van Es A, Marx JJ, Hertsig ML, Struyvenberg A. Low-dose aspirin does not prevent thrombovascular accidents in low-risk haemodialysis patients during treatment with recombinant human erythropoietin. Nephrol Dial Transplant. 1994; 9:1115–1120.
Article27. Wolf RF, Peng J, Friese P, Gilmore LS, Burstein SA, Dale GL. Erythropoietin administration increases production and reactivity of platelets in dogs. Thromb Haemost. 1997; 78:1505–1509.
Article28. Stohlawetz PJ, Dzirlo L, Hergovich N, Lackner E, Mensik C, Eichler HG, et al. Effects of erythropoietin on platelet reactivity and thrombopoiesis in humans. Blood. 2000; 95:2983–2989.
Article29. Dessypris E, Graber SE, Krantz SB, Stone WJ. Effects of recombinant erythropoietin on the concentration and cycling status of human marrow hematopoietic progenitor cells in vivo. Blood. 1988; 72:2060–2062.
Article30. Cases A, Escolar G, Reverter JC, Ordinas A, Lopez-Pedret J, Revert L, et al. Recombinant human erythropoietin treatment improves platelet function in uremic patients. Kidney Int. 1992; 42:668–672.
Article31. Smith KJ, Bleyer AJ, Little WC, Sane DC. The cardiovascular effects of erythropoietin. Cardiovasc Res. 2003; 59:538–548.
Article32. Roger SD, Fluck RJ, McMahon AC, Raine AE. Recombinant erythropoietin increases blood pressure in experimental hypertension and uraemia without change in vascular cytosolic calcium. Nephron. 1996; 73:212–218.
Article33. Noguchi K, Yamashiro S, Matsuzaki T, Sakanashi M, Nakasone J, Miyagi K, et al. Effect of 1-week treatment with erythropoietin on the vascular endothelial function in anaesthetized rabbits. Br J Pharmacol. 2001; 133:395–405.
Article34. Salmela B, Hartman J, Peltonen S, Albäck A, Lassila R. Thrombophilia and arteriovenous fistula survival in ESRD. Clin J Am Soc Nephrol. 2013; 8:962–968.
Article35. Xue H, Lacson E Jr, Wang W, Curhan GC, Brunelli SM. Choice of vascular access among incident hemodialysis patients: a decision and cost-utility analysis. Clin J Am Soc Nephrol. 2010; 5:2289–2296.
Article36. Ryu JH, Kim H, Kim KH, Hann HJ, Ahn HS, Lee S, et al. Improving survival rate of Korean patients initiating dialysis. Yonsei Med J. 2015; 56:666–675.
Article37. Feldman HI, Kobrin S, Wasserstein A. Hemodialysis vascular access morbidity. J Am Soc Nephrol. 1996; 7:523–535.
Article38. Vascular Access Work Group. Clinical practice guidelines for vascular access. Am J Kidney Dis. 2006; 48:Suppl 1. S248–S273.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- High-Output Cardiac Failure due to Expressive Arteriovenous Fistula Blood Flow in a Hemodialysis Patient
- Clinical Characteristics of Poor Responders to Erythropoietin among ESRD Patients Undergoing Hemodialysis
- Pseudo - Kaposi' s Sarcoma Developing After Placement of A - V Fistula for Hemodialysis
- Causes of Failed Internal Arteriovenous Fistula and Their Salvage Procedures
- Ulnobasilic Arteriovenous Fistula for Hemodialysis