Yonsei Med J.
2017 Sep;58(5):944-953. 10.3349/ymj.2017.58.5.944.
Healthcare Costs for Acute Hospitalized and Chronic Heart Failure in South Korea: A Multi-Center Retrospective Cohort Study
- Affiliations
-
- 1School of Pharmacy, Sungkyunkwan University, Suwon, Korea. ekyung@skku.edu
- 2Department of Cardiovascular Medicine, Gachon Cardiovascular Research Institute, Gachon University Gil Medical Center, Incheon, Korea.
- 3Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 4Division of Cardiology, Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 5Division of Cardiology, Department of Medicine, Heart Vascular Stroke Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 6Department of Cardiovascular Medicine, Dongtan Sacred Heart Hospital, College of Medicine, Hallym University, Hwaseong, Korea.
- 7Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. smkang@yumc.yonsei.ac.kr
- KMID: 2418929
- DOI: http://doi.org/10.3349/ymj.2017.58.5.944
Abstract
- PURPOSE
Although heart failure (HF) is recognized as a leading contributor to healthcare costs and a significant economic burden worldwide, studies of HF-related costs in South Korea are limited. This study aimed to estimate HF-related costs per Korean patient per year and per visit.
MATERIALS AND METHODS
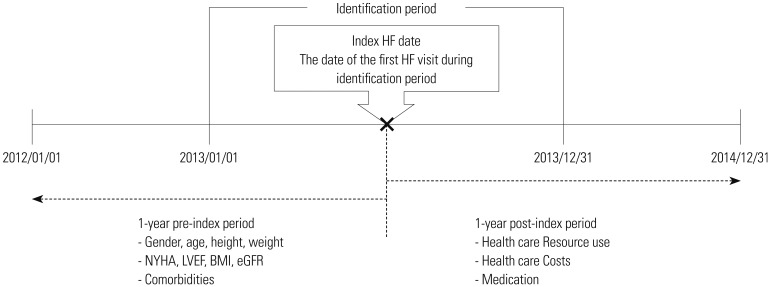
This retrospective cohort study analyzed data obtained from six hospitals in South Korea. Patients with HF who experienced ≥one hospitalization or ≥two outpatient visits between January 1, 2013 and December 31, 2013 were included. Patients were followed up for 1 year [in Korean won (KRW)].
RESULTS
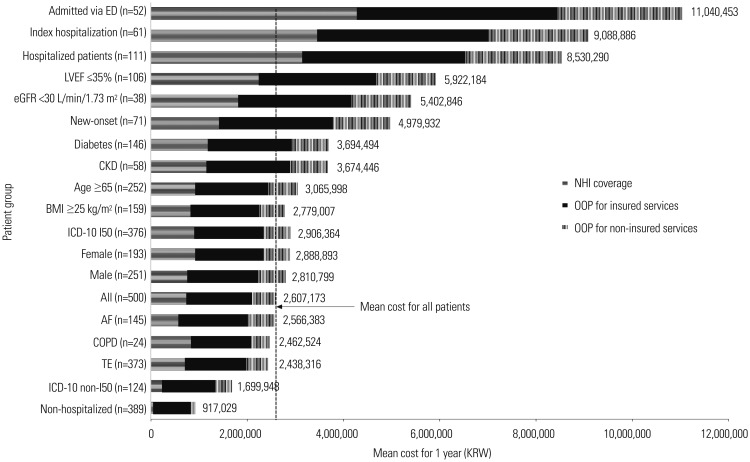
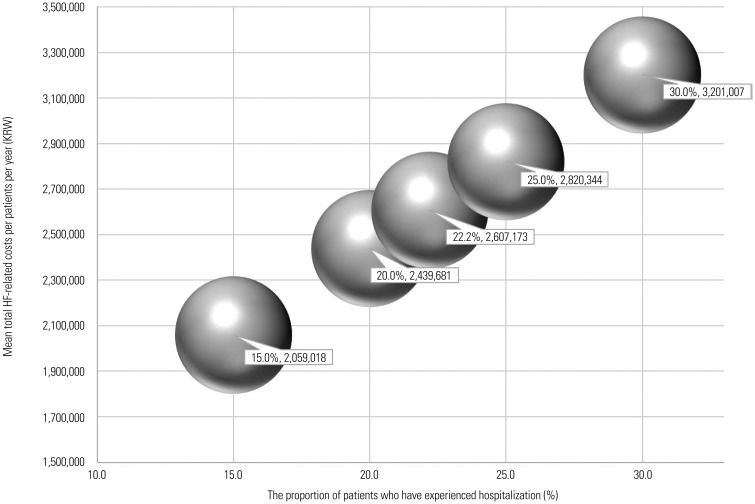
Among a total of 500 patients (mean age, 66.1 years; male sex, 54.4%), the mean 1-year HF-related cost per patient was KRW 2,607,173, which included both, outpatient care (KRW 952,863) and inpatient care (KRW 1,654,309). During the post-index period, 22.2% of patients had at least one hospitalization, and their 1-year costs per patient (KRW 8,530,290) were higher than those of patients who had only visited a hospital over a 12-month period (77.8%; KRW 917,029). Among 111 hospitalized patients, the 1-year costs were 1.7-fold greater in patients (n=52) who were admitted to the hospital via the emergency department (ED) than in those (n=59) who were not (KRW 11,040,453 vs. KRW 6,317,942; p<0.001).
CONCLUSION
The majority of healthcare costs for HF patients in South Korea was related to hospitalization, especially admissions via the ED. Appropriate treatment strategies including modification of risk factors to prevent or decrease hospitalization are needed to reduce the economic burden on HF patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Lee JH, Lim NK, Cho MC, Park HY. Epidemiology of heart failure in Korea: present and future. Korean Circ J. 2016; 46:658–664. PMID: 27721857.
Article2. Health Insurance Review & Assessment Service. National Health Insurance Statistical Yearbook. accessed on 2016 November 20. Available at: http://opendata.hira.or.kr.3. Liao L, Allen LA, Whellan DJ. Economic burden of heart failure in the elderly. Pharmacoeconomics. 2008; 26:447–462. PMID: 18489197.4. Braunschweig F, Cowie MR, Auricchio A. What are the costs of heart failure? Europace. 2011; 13(Suppl 2):ii13–ii17. PMID: 21518742.
Article5. Mpe MT, Klug EQ, Silwa KS, Hitzeroth J, Smith DA. Heart Failure Society of South Africa (HeFSSA) perspective on the European Society of Cardiology (ESC) 2012 chronic heart failure guideline. S Afr Med J. 2013; 103(9 Suppl 2):660–667. PMID: 24300688.
Article6. Stewart S, Jenkins A, Buchan S, McGuire A, Capewell S, McMurray JJ. The current cost of heart failure to the National Health Service in the UK. Eur J Heart Fail. 2002; 4:361–371. PMID: 12034163.
Article7. Lee WC, Chavez YE, Baker T, Luce BR. Economic burden of heart failure: a summary of recent literature. Heart Lung. 2004; 33:362–371. PMID: 15597290.
Article8. Stewart S, Carrington MJ, Marwick TH, Davidson PM, Macdonald P, Horowitz JD, et al. Impact of home versus clinic-based management of chronic heart failure: the WHICH? (Which Heart Failure Intervention Is Most Cost-Effective & Consumer Friendly in Reducing Hospital Care) multicenter, randomized trial. J Am Coll Cardiol. 2012; 60:1239–1248. PMID: 23017533.9. Lee SE, Cho HJ, Lee HY, Yang HM, Choi JO, Jeon ES, et al. A multicentre cohort study of acute heart failure syndromes in Korea: rationale, design, and interim observations of the Korean Acute Heart Failure (KorAHF) registry. Eur J Heart Fail. 2014; 16:700–708. PMID: 24797348.
Article10. National Institute for Health and Clinical Excellence. New NICE guidance will improve diagnosis and treatment of chronic heart failure. accessed on 2016 March 16. Available at: http://www.nice.org.uk/newsroom/pressreleases/chronicheartfailureguidance.jsp.11. The Cost of Heart Failure in Ireland, Social, Economic and Health Implications of heart failure in Ireland. accessed on 2013 March 16. Available at: http://docplayer.net/29464538-The-cost-of-heart-failure-in-ireland-the-social-economic-and-health-implications-of-heart-failure-in-ireland-supported-by.html.12. Correction to: 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2016; 134:e298. PMID: 27672202.13. National Clinical Guideline Centre (UK). Acute heart failure: diagnosing and managing acute heart failure in adults. London: National Institute for Health and Care Excellence (UK);2014.14. Choi DJ, Han S, Jeon ES, Cho MC, Kim JJ, Yoo BS, et al. Characteristics, outcomes and predictors of long-term mortality for patients hospitalized for acute heart failure: a report from the Korean heart failure registry. Korean Circ J. 2011; 41:363–371. PMID: 21860637.
Article15. Ahmed A, Campbell RC. Epidemiology of chronic kidney disease in heart failure. Heart Fail Clin. 2008; 4:387–399. PMID: 18760751.
Article16. McAlister FA, Ezekowitz J, Tonelli M, Armstrong PW. Renal insufficiency and heart failure: prognostic and therapeutic implications from a prospective cohort study. Circulation. 2004; 109:1004–1009. PMID: 14769700.17. Cleland JG, Carubelli V, Castiello T, Yassin A, Pellicori P, Antony R. Renal dysfunction in acute and chronic heart failure: prevalence, incidence and prognosis. Heart Fail Rev. 2012; 17:133–149. PMID: 22426973.
Article18. McClellan W, Warnock DG, McClure L, Campbell RC, Newsome BB, Howard V, et al. Racial differences in the prevalence of chronic kidney disease among participants in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Cohort Study. J Am Soc Nephrol. 2006; 17:1710–1715. PMID: 16641151.
Article19. Smith DH, Johnson ES, Blough DK, Thorp ML, Yang X, Petrik AF, et al. Predicting costs of care in heart failure patients. BMC Health Serv Res. 2012; 12:434. PMID: 23194470.
Article20. Metra M, Felker GM, Zacà V, Bugatti S, Lombardi C, Bettari L, et al. Acute heart failure: multiple clinical profiles and mechanisms require tailored therapy. Int J Cardiol. 2010; 144:175–179. PMID: 20537739.
Article21. Krum H, Jelinek MV, Stewart S, Sindone A, Atherton JJ, Hawkes AL. CHF Guidelines Core Writers. Guidelines for the prevention, detection and management of people with chronic heart failure in Australia 2006. Med J Aust. 2006; 185:549–557. PMID: 17115967.
Article22. Owan TE, Redfield MM. Epidemiology of diastolic heart failure. Prog Cardiovasc Dis. 2005; 47:320–332. PMID: 16003647.
Article23. Senni M, Tribouilloy CM, Rodeheffer RJ, Jacobsen SJ, Evans JM, Bailey KR, et al. Congestive heart failure in the community: a study of all incident cases in Olmsted County, Minnesota, in 1991. Circulation. 1998; 98:2282–2289. PMID: 9826315.24. Kupari M, Lindroos M, Iivanainen AM, Heikkilä J, Tilvis R. Congestive heart failure in old age: prevalence, mechanisms and 4-year prognosis in the Helsinki Ageing Study. J Intern Med. 1997; 241:387–394. PMID: 9183306.
Article25. Sun SX, Ye X, Lee KY, Dupclay L Jr, Plauschinat C. Retrospective claims database analysis to determine relationship between renin-angiotensin system agents, rehospitalization, and health care costs in patients with heart failure or myocardial infarction. Clin Ther. 2008; 30(Pt 2):2217–2227. PMID: 19281916.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Practical Way to Reduce Healthcare Costs in Patients With Heart Failure: Outpatient IV Diuretics Therapy
- Economic Burden of Heart Failure in Asian Countries with Different Healthcare Systems
- Optimal Management of Chronic Medical Conditions Through Digital Medicine
- Multi-Agent System as a New Approach to Effective Chronic Heart Failure Management: Key Considerations
- Effectiveness and Approach of Rehabilitation in Patients With Acute Heart Failure: A Review