Yonsei Med J.
2017 Nov;58(6):1128-1134. 10.3349/ymj.2017.58.6.1128.
Subsequent Thrombotic Outcomes in Patients with Ischemic Stroke with Antiphospholipid Antibody Positivity
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. yongbpark@yuhs.ac
- KMID: 2418894
- DOI: http://doi.org/10.3349/ymj.2017.58.6.1128
Abstract
- PURPOSE
International consensus criteria for antiphospholipid syndrome (APS) require persistently positive antiphospholipid antibodies (aPL) and medium or high titers in association with clinical manifestations. However, the clinical relevance of persistence and titers of aPL in patients with stroke has not been identified. We aimed to investigate the risk of subsequent thrombotic events in patients with ischemic stroke with aPL positivity in terms of aPL status.
MATERIALS AND METHODS
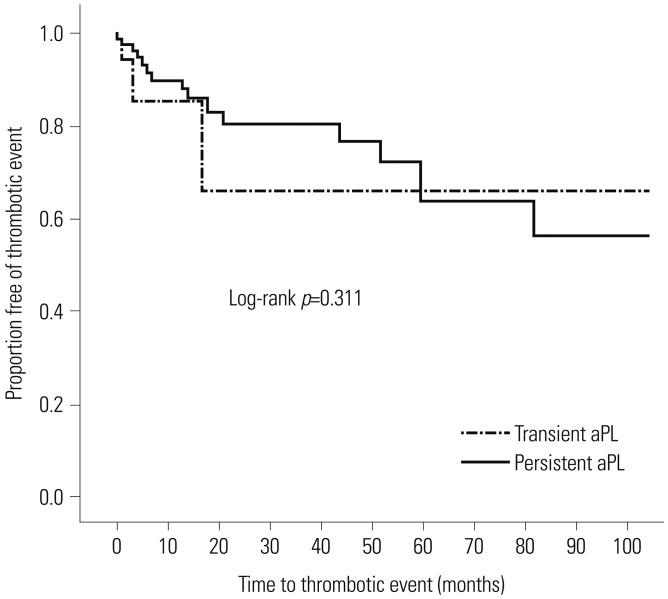
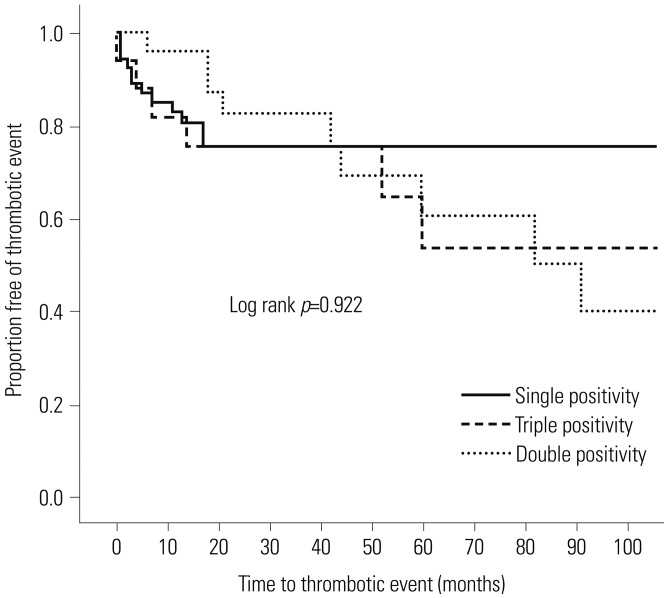
We reviewed the medical records of 99 patients with ischemic stroke with at least one or more aPL-positivity (i.e., positivity for aCL, anti-β2-glycoprotein-1, and/or lupus anticoagulants). The patients were divided into two groups: "definite APS" who fulfilled the laboratory criteria and "indefinite APS" who fell short of the criteria. We compared the risk of subsequent thrombotic events between the two groups. Cox proportional hazards model and Kaplan-Meier survival curves were used for the analyses.
RESULTS
Of the 99 patients, 46 (46%) were classified as having definite APS and 53 (54%) as having indefinite APS. The mean follow-up was 51.6 months. Overall event numbers were 14 (30.4%) in definite APS and 16 (30.2%) in indefinite APS. Increased subsequent thrombotic events (hazard ratio 1.039; 95% confidence interval 0.449-2.404; p=0.930) and decreased time to thrombotic events (log-rank p=0.321) were not associated with aPL status.
CONCLUSION
There was no increased risk of subsequent thrombotic events in ischemic stroke patients with definite APS, compared with those with indefinite APS.
Keyword
MeSH Terms
-
Antibodies, Antiphospholipid/*blood/*immunology
Antiphospholipid Syndrome/complications/immunology
Female
Humans
Kaplan-Meier Estimate
Lupus Coagulation Inhibitor/blood
Male
Middle Aged
Proportional Hazards Models
Recurrence
Stroke/complications/*epidemiology/immunology/prevention & control
Thrombosis/complications/*immunology/prevention & control
beta 2-Glycoprotein I/immunology
Antibodies, Antiphospholipid
Lupus Coagulation Inhibitor
beta 2-Glycoprotein I
Figure
Reference
-
1. Krnic-Barrie S, O'Connor CR, Looney SW, Pierangeli SS, Harris EN. A retrospective review of 61 patients with antiphospholipid syndrome. Analysis of factors influencing recurrent thrombosis. Arch Intern Med. 1997; 157:2101–2108. PMID: 9382667.
Article2. Shah NM, Khamashta MA, Atsumi T, Hughes GR. Outcome of patients with anticardiolipin antibodies: a 10 year follow-up of 52 patients. Lupus. 1998; 7:3–6. PMID: 9493141.
Article3. Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. 2006; 4:295–306. PMID: 16420554.
Article4. Shi W, Krilis SA, Chong BH, Gordon S, Chesterman CN. Prevalence of lupus anticoagulant and anticardiolipin antibodies in a healthy population. Aust N Z J Med. 1990; 20:231–236. PMID: 2115326.
Article5. Vila P, Hernández MC, López-Fernández MF, Batlle J. Prevalence, follow-up and clinical significance of the anticardiolipin antibodies in normal subjects. Thromb Haemost. 1994; 72:209–213. PMID: 7831653.
Article6. Male C, Foulon D, Hoogendoorn H, Vegh P, Silverman E, David M, et al. Predictive value of persistent versus transient antiphospholipid antibody subtypes for the risk of thrombotic events in pediatric patients with systemic lupus erythematosus. Blood. 2005; 106:4152–4158. PMID: 16144797.
Article7. Levine SR, Salowich-Palm L, Sawaya KL, Perry M, Spencer HJ, Winkler HJ, et al. IgG anticardiolipin antibody titer > 40 GPL and the risk of subsequent thrombo-occlusive events and death. A prospective cohort study. Stroke. 1997; 28:1660–1665. PMID: 9303006.8. Ruffatti A, Del Ross T, Ciprian M, Nuzzo M, Rampudda M, Bertero MT, et al. Risk factors for a first thrombotic event in antiphospholipid antibody carriers. A multicentre, retrospective follow-up study. Ann Rheum Dis. 2009; 68:397–399. PMID: 18812393.
Article9. Erkan D, Barbhaiya M, George D, Sammaritano L, Lockshin M. Moderate versus high-titer persistently anticardiolipin antibody positive patients: are they clinically different and does high-titer anti-β2-glycoprotein-I antibody positivity offer additional predictive information? Lupus. 2010; 19:613–619. PMID: 19934177.
Article10. Ofer-Shiber S, Molad Y. Frequency of vascular and pregnancy morbidity in patients with low vs. moderate-to-high titers of antiphospholipid antibodies. Blood Coagul Fibrinolysis. 2015; 26:261–266. PMID: 25526601.
Article11. Stojanovich L, Markovic O, Marisavljevic D, Elezovic I, Ilijevski N, Stanisavljevic N. Influence of antiphospholipid antibody levels and type on thrombotic manifestations: results from the Serbian National Cohort Study. Lupus. 2012; 21:338–345. PMID: 21993381.
Article12. Espinosa G, Cervera R. Current treatment of antiphospholipid syndrome: lights and shadows. Nat Rev Rheumatol. 2015; 11:586–596. PMID: 26122952.
Article13. Sciascia S, Sanna G, Khamashta MA, Cuadrado MJ, Erkan D, Andreoli L, et al. The estimated frequency of antiphospholipid antibodies in young adults with cerebrovascular events: a systematic review. Ann Rheum Dis. 2015; 74:2028–2033. PMID: 24942381.
Article14. Lim W. Antiphospholipid antibody syndrome. Hematology Am Soc Hematol Educ Program. 2009; 233–239. PMID: 20008203.
Article15. Levine SR, Brey RL, Tilley BC, Thompson JL, Sacco RL, Sciacca RR, et al. Antiphospholipid antibodies and subsequent thrombo-occlusive events in patients with ischemic stroke. JAMA. 2004; 291:576–584. PMID: 14762036.
Article16. Lim W, Crowther MA, Eikelboom JW. Management of antiphospholipid antibody syndrome: a systematic review. JAMA. 2006; 295:1050–1057. PMID: 16507806.17. Amory CF, Levine SR, Brey RL, Gebregziabher M, Tuhrim S, Tilley BC, et al. Antiphospholipid antibodies and recurrent thrombotic events: persistence and portfolio. Cerebrovasc Dis. 2015; 40:293–300. PMID: 26513489.
Article18. Brey RL, Abbott RD, Curb JD, Sharp DS, Ross GW, Stallworth CL, et al. β2-Glycoprotein 1-dependent anticardiolipin antibodies and risk of ischemic stroke and myocardial infarction: the honolulu heart program. Stroke. 2001; 32:1701–1706. PMID: 11486093.19. Pezzini A, Grassi M, Lodigiani C, Patella R, Gandolfo C, Zini A, et al. Predictors of long-term recurrent vascular events after ischemic stroke at young age: the Italian project on stroke in young adults. Circulation. 2014; 129:1668–1676. PMID: 24508827.20. Forastiero R, Martinuzzo M, Pombo G, Puente D, Rossi A, Celebrin L, et al. A prospective study of antibodies to β2-glycoprotein I and prothrombin, and risk of thrombosis. J Thromb Haemost. 2005; 3:1231–1238. PMID: 15946213.
Article21. Lanthier S, Kirkham FJ, Mitchell LG, Laxer RM, Atenafu E, Male C, et al. Increased anticardiolipin antibody IgG titers do not predict recurrent stroke or TIA in children. Neurology. 2004; 62:194–200. PMID: 14745053.
Article22. Rajamani K, Chaturvedi S, Jin Z, Homma S, Brey RL, Tilley BC, et al. Patent foramen ovale, cardiac valve thickening, and antiphospholipid antibodies as risk factors for subsequent vascular events: the PICSS-APASS study. Stroke. 2009; 40:2337–2342. PMID: 19498198.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recurrent Ischemic Stroke by Carotid Free-Floating Thrombus in Patient with Antiphospholipid Antibody Syndrome
- Hepatic infarction in a pregnant woman with antiphospholipid syndrome and triple antibody positivity: A case report focusing on catastrophic antiphospholipid syndrome
- A Case of Antiphospholipid Antibody Syndrome with AhA Nephropathy
- A Case of Refractory Headache with Antiphospholipid Antibody Syndrome Improved by High-Intensity Warfarin Medication
- Successful Graft Recovery from Thrombotic Acute Kidney Injury in a Kidney Transplant Patient with Antiphospholipid Syndrome