Yonsei Med J.
2018 Mar;59(2):265-272. 10.3349/ymj.2018.59.2.265.
Impact of Ambulatory Blood Pressure on Early Cardiac and Renal Dysfunction in Hypertensive Patients without Clinically Apparent Target Organ Damage
- Affiliations
-
- 1Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. cysprs@yuhs.ac
- KMID: 2418790
- DOI: http://doi.org/10.3349/ymj.2018.59.2.265
Abstract
- PURPOSE
Impaired left ventricular (LV) global longitudinal strain (GLS) and the presence of microalbuminuria indicate early cardiac and renal dysfunction. We aimed to determine the relationships among 24-h ambulatory blood pressure (BP) variables, LV GLS, and urine albumin creatinine ratio (UACR) in hypertensive patients.
MATERIALS AND METHODS
A total of 130 hypertensive patients (mean age 53 years; 59 men) underwent 24-h ambulatory BP monitoring, measurements of peripheral and central BPs, and transthoracic echocardiography. Patients with apparent LV systolic dysfunction (LV ejection fraction < 50%) or chronic kidney disease were not included. LV GLS was calculated using two-dimensional speckle tracking, and UACR was analyzed from spot urine samples.
RESULTS
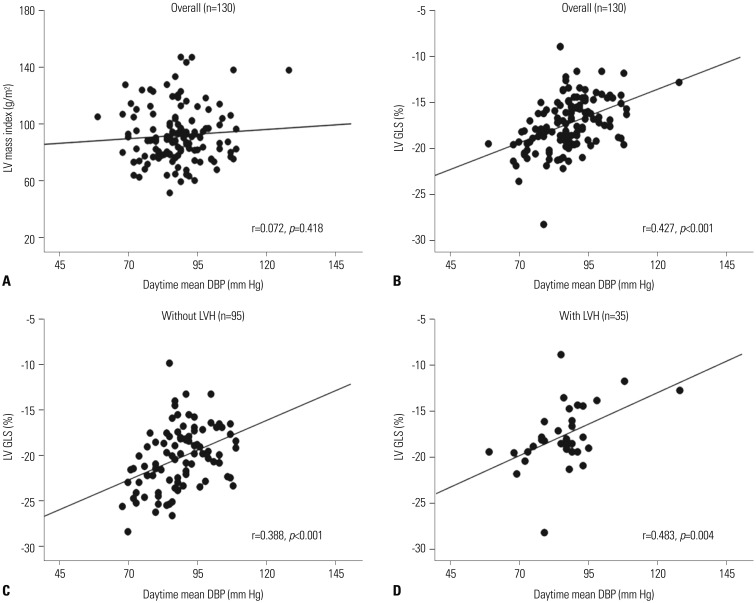
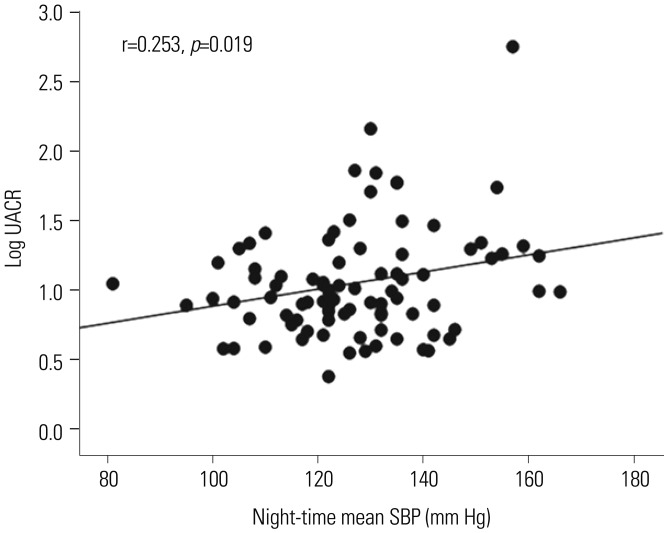
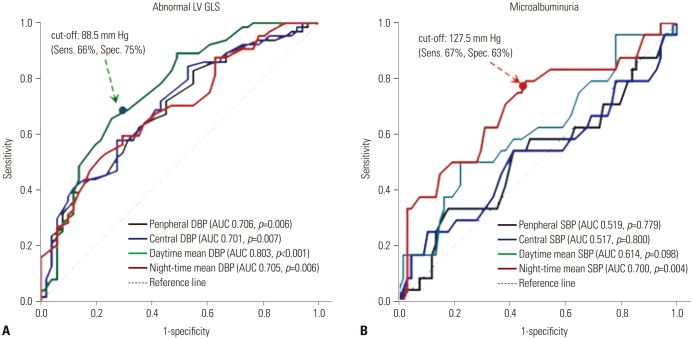
In simple correlation analysis, LV GLS showed the most significant correlation with mean daytime diastolic BP (DBP) (r=0.427, p < 0.001) among the various BP variables analyzed. UACR revealed a significant correlation only with night-time mean systolic BP (SBP) (r=0.253, p=0.019). In multiple regression analysis, daytime mean DBP and night-time mean SBP were independent determinants for LV GLS (β=0.35, p=0.028) and log UACR (β=0.49, p=0.007), respectively, after controlling for confounding factors. Daytime mean DBP showed better diagnostic performance for impaired LV GLS than did peripheral or central DBPs, which were not diagnostic. Night-time mean SBP showed satisfactory diagnostic performance for microalbuminuria.
CONCLUSION
There are different associations for daytime and night-time BP with early cardiac and renal dysfunction. Ambulatory BP monitoring provides more relevant BP parameters than do peripheral or central BPs regarding early cardiac and renal dysfunction in hypertensive patients.
MeSH Terms
-
Blood Pressure/physiology
*Blood Pressure Monitoring, Ambulatory
Echocardiography
Female
Heart/*physiopathology
Humans
Hypertension/diagnostic imaging/*physiopathology
Kidney/*physiopathology
Kidney Function Tests
Male
Middle Aged
Regression Analysis
Systole/physiology
Ventricular Dysfunction, Left/physiopathology
Ventricular Function, Left/physiology
Figure
Reference
-
1. Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burnier M, Caulfield MJ, et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. Blood Press. 2009; 18:308–347. PMID: 20001654.
Article2. Tocci G, Sciarretta S, Volpe M. Development of heart failure in recent hypertension trials. J Hypertens. 2008; 26:1477–1486. PMID: 18551026.
Article3. Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez DA, Fagard RH, et al. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med. 2003; 348:2407–2415. PMID: 12802026.
Article4. Dolan E, Stanton A, Thijs L, Hinedi K, Atkins N, McClory S, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005; 46:156–161. PMID: 15939805.5. Wei FF, Li Y, Zhang L, Xu TY, Ding FH, Staessen JA, et al. Association of target organ damage with 24-hour systolic and diastolic blood pressure levels and hypertension subtypes in untreated Chinese. Hypertension. 2014; 63:222–228. PMID: 24246384.
Article6. Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp-Pedersen C. Ambulatory blood pressure monitoring and risk of cardiovascular disease: a population based study. Am J Hypertens. 2006; 19:243–250. PMID: 16500508.
Article7. Mancia G, Parati G. Ambulatory blood pressure monitoring and organ damage. Hypertension. 2000; 36:894–900. PMID: 11082163.
Article8. Palatini P, Graniero GR, Canali C, Santonastaso M, Mos L, Piccolo D, et al. Relationship between albumin excretion rate, ambulatory blood pressure and left ventricular hypertrophy in mild hypertension. J Hypertens. 1995; 13(12 Pt 2):1796–1800. PMID: 8903654.
Article9. Manyari DE. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990; 323:1706–1707. PMID: 2146505.
Article10. Kalam K, Otahal P, Marwick TH. Prognostic implications of global LV dysfunction: a systematic review and meta-analysis of global longitudinal strain and ejection fraction. Heart. 2014; 100:1673–1680. PMID: 24860005.
Article11. Kraigher-Krainer E, Shah AM, Gupta DK, Santos A, Claggett B, Pieske B, et al. Paramount Investigators. Impaired systolic function by strain imaging in heart failure with preserved ejection fraction. J Am Coll Cardiol. 2014; 63:447–456. PMID: 24184245.
Article12. Na HM, Cho GY, Lee JM, Cha MJ, Yoon YE, Lee SP, et al. Echocardiographic predictors for left ventricular remodeling after acute ST elevation myocardial infarction with low risk group: speckle tracking analysis. J Cardiovasc Ultrasound. 2016; 24:128–134. PMID: 27358705.
Article13. Pontremoli R, Nicolella C, Viazzi F, Ravera M, Sofia A, Berruti V, et al. Microalbuminuria is an early marker of target organ damage in essential hypertension. Am J Hypertens. 1998; 11(4 Pt 1):430–438. PMID: 9607381.
Article14. Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, BÖhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013; 31:1281–1357. PMID: 23817082.15. Weber T, O'Rourke MF, Ammer M, Kvas E, Punzengruber C, Eber B. Arterial stiffness and arterial wave reflections are associated with systolic and diastolic function in patients with normal ejection fraction. Am J Hypertens. 2008; 21:1194–1202. PMID: 18787521.
Article16. Weber T, Auer J, O'Rourke MF, Kvas E, Lassnig E, Berent R, et al. Arterial stiffness, wave reflections, and the risk of coronary artery disease. Circulation. 2004; 109:184–189. PMID: 14662706.
Article17. Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003; 107:1401–1406. PMID: 12642361.18. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Chamber Quantification Writing Group. American Society of Echocardiography's Guidelines and Standards Committee. European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463. PMID: 16376782.
Article19. Mattix HJ, Hsu CY, Shaykevich S, Curhan G. Use of the albumin/creatinine ratio to detect microalbuminuria: implications of sex and race. J Am Soc Nephrol. 2002; 13:1034–1039. PMID: 11912263.
Article20. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015; 16:233–270. PMID: 25712077.
Article21. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–845. PMID: 3203132.
Article22. Park S, Kario K, Park CG, Huang QF, Cheng HM, Hoshide S, et al. Characteristics On the ManagEment of Hypertension in Asia-Morning Hypertension Discussion Group (COME Asia MHDG). Target blood pressure in patients with diabetes: Asian perspective. Yonsei Med J. 2016; 57:1307–1311. PMID: 27593856.
Article23. Armstrong AC, Gidding S, Gjesdal O, Wu C, Bluemke DA, Lima JA. LV mass assessed by echocardiography and CMR, cardiovascular outcomes, and medical practice. JACC Cardiovasc Imaging. 2012; 5:837–848. PMID: 22897998.
Article24. Asselbergs FW, Diercks GF, Hillege HL, van Boven AJ, Janssen WM, Voors AA, et al. Prevention of Renal and Vascular Endstage Disease Intervention Trial (PREVEND IT) Investigators. Effects of fosinopril and pravastatin on cardiovascular events in subjects with microalbuminuria. Circulation. 2004; 110:2809–2816. PMID: 15492322.
Article25. de Zeeuw D, Remuzzi G, Parving HH, Keane WF, Zhang Z, Shahinfar S, et al. Albuminuria, a therapeutic target for cardiovascular protection in type 2 diabetic patients with nephropathy. Circulation. 2004; 110:921–927. PMID: 15302780.
Article26. Saito M, Khan F, Stoklosa T, Iannaccone A, Negishi K, Marwick TH. Prognostic implications of LV strain risk score in asymptomatic patients with hypertensive heart disease. JACC Cardiovasc Imaging. 2016; 9:911–921. PMID: 27344417.27. Narayanan A, Aurigemma GP, Chinali M, Hill JC, Meyer TE, Tighe DA. Cardiac mechanics in mild hypertensive heart disease: a speckle-strain imaging study. Circ Cardiovasc Imaging. 2009; 2:382–390. PMID: 19808626.28. Imbalzano E, Zito C, Carerj S, Oreto G, Mandraffino G, Cusmà-Piccione M, et al. Left ventricular function in hypertension: new insight by speckle tracking echocardiography. Echocardiography. 2011; 28:649–657. PMID: 21676016.
Article29. Mizuguchi Y, Oishi Y, Miyoshi H, Iuchi A, Nagase N, Oki T. Concentric left ventricular hypertrophy brings deterioration of systolic longitudinal, circumferential, and radial myocardial deformation in hypertensive patients with preserved left ventricular pump function. J Cardiol. 2010; 55:23–33. PMID: 20122545.
Article30. Cheng S, Shah AM, Albisu JP, Desai AS, Hilkert RJ, Izzo J, et al. Reversibility of left ventricular mechanical dysfunction in patients with hypertensive heart disease. J Hypertens. 2014; 32:2479–2486. PMID: 25232755.
Article31. Khattar RS, Swales JD, Dore C, Senior R, Lahiri A. Effect of aging on the prognostic significance of ambulatory systolic, diastolic, and pulse pressure in essential hypertension. Circulation. 2001; 104:783–789. PMID: 11502703.
Article32. Kannel WB, Gordon T, Schwartz MJ. Systolic versus diastolic blood pressure and risk of coronary heart disease. The Framingham study. Am J Cardiol. 1971; 27:335–346. PMID: 5572576.33. Franklin SS, Gustin W 4th, Wong ND, Larson MG, Weber MA, Kannel WB, et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation. 1997; 96:308–315. PMID: 9236450.34. Sera F, Jin Z, Russo C, Lee ES, Schwartz JE, Rundek T, et al. Relationship of office and ambulatory blood pressure with left ventricular global longitudinal strain. Am J Hypertens. 2016; 29:1261–1267.
Article35. Eguchi K, Pickering TG, Hoshide S, Ishikawa J, Ishikawa S, Schwartz JE, et al. Ambulatory blood pressure is a better marker than clinic blood pressure in predicting cardiovascular events in patients with/without type 2 diabetes. Am J Hypertens. 2008; 21:443–450. PMID: 18292756.
Article36. Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA. Predictive role of the nighttime blood pressure. Hypertension. 2011; 57:3–10. PMID: 21079049.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of Urinary Microalbuminuria in Normal and Hypertensive Koreans and Its Correlation with Blood Pressure Measured by 24 Hours Ambulatory Blood Pressure Monitoring
- 24 hour circadian pattern of blood pressure and its related target organ damage in hypertensive subjects
- Hypertensive Retinopathy and Associated Target Organ Damage in Korean Hypertensive Patients
- Prevalence of early renal damage between dippers and non-dippers in mild to moderate Korean hypertensives
- Arterial stiffness and hypertension