Diabetes Metab J.
2018 Aug;42(4):320-329. 10.4093/dmj.2017.0104.
Air Pollution Has a Significant Negative Impact on Intentional Efforts to Lose Weight: A Global Scale Analysis
- Affiliations
-
- 1Department of Medicine, Graduate School of Medicine, Kyung Hee University, Seoul, Korea.
- 2Department of Endocrinology and Metabolism, Kyung Hee University School of Medicine, Seoul, Korea. rheesy@khu.ac.kr
- KMID: 2418720
- DOI: http://doi.org/10.4093/dmj.2017.0104
Abstract
- BACKGROUND
Air pollution causes many diseases and deaths. It is important to see how air pollution affects obesity, which is common worldwide. Therefore, we analyzed data from a smartphone application for intentional weight loss, and then we validated them.
METHODS
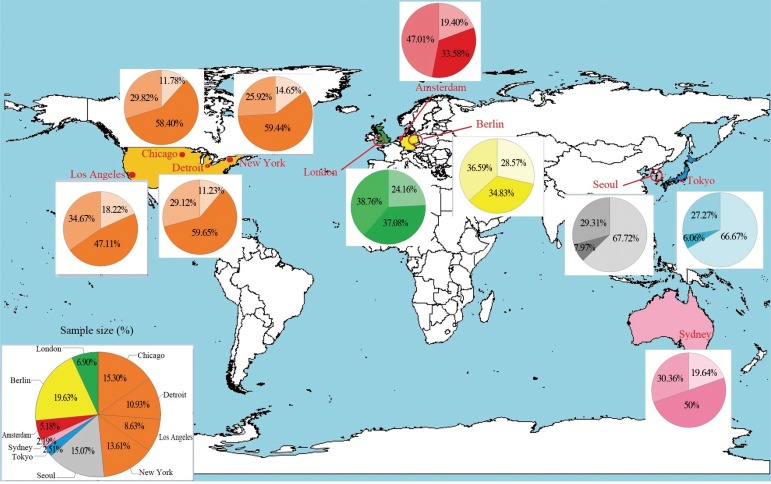
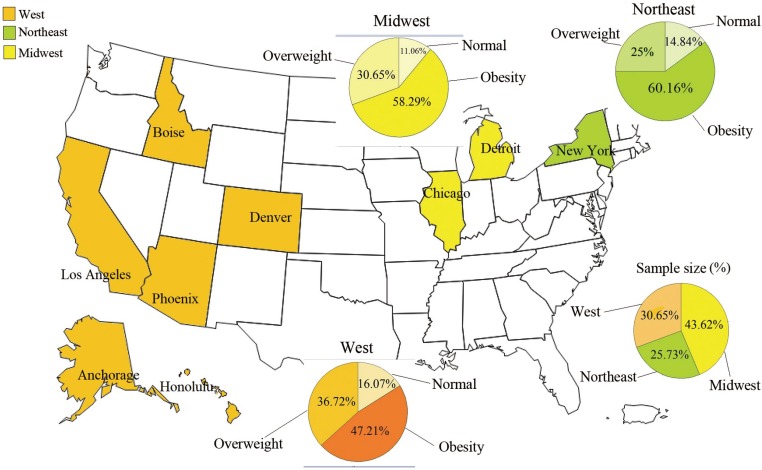
Our analysis was structured in two parts. We analyzed data from a cohort registered to a smartphone application in 10 large cities of the world and matched it with the annual pollution values. We validated these results using daily pollution data in United States and matching them with user information. Body mass index (BMI) variation between final and initial login time was considered as outcome in the first part, and daily BMI in the validation. We analyzed: daily calories intake, daily weight, daily physical activity, geographical coordinates, seasons, age, gender. Weather Underground application programming interface provided daily climatic values. Annual and daily values of particulate matter PM10 and PM2.5 were extracted. In the first part of the analysis, we used 2,608 users and then 995 users located in United States.
RESULTS
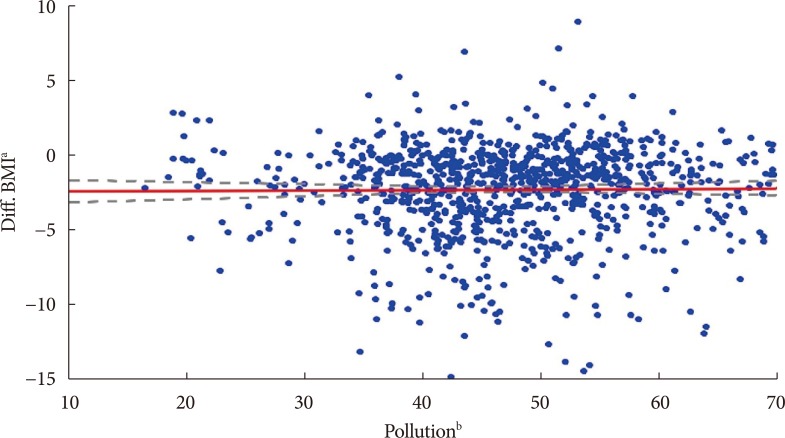
Air pollution was highest in Seoul and lowest in Detroit. Users decreased BMI by 2.14 kg/m2 in average (95% confidence interval, −2.26 to −2.04). From a multilevel model, PM10 (β=0.04, P=0.002) and PM2.5 (β=0.08, P < 0.001) had a significant negative effect on weight loss when collected per year. The results were confirmed with the validation (βAQI*time=1.5×10-5; P < 0.001) by mixed effects model.
CONCLUSION
This is the first study that shows how air pollution affects intentional weight loss applied on wider area of the world.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Can Air Pollution Biologically Hinder Efforts to Lose Body Weight?
Duk-Hee Lee
Diabetes Metab J. 2018;42(4):282-284. doi: 10.4093/dmj.2018.0139.
Reference
-
1. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, Abraham JP, Abu-Rmeileh NM, Achoki T, AlBuhairan FS, Alemu ZA, Alfonso R, Ali MK, Ali R, Guzman NA, Ammar W, Anwari P, Banerjee A, Barquera S, Basu S, Bennett DA, Bhutta Z, Blore J, Cabral N, Nonato IC, Chang JC, Chowdhury R, Courville KJ, Criqui MH, Cundiff DK, Dabhadkar KC, Dandona L, Davis A, Dayama A, Dharmaratne SD, Ding EL, Durrani AM, Esteghamati A, Farzadfar F, Fay DF, Feigin VL, Flaxman A, Forouzanfar MH, Goto A, Green MA, Gupta R, Hafezi-Nejad N, Hankey GJ, Harewood HC, Havmoeller R, Hay S, Hernandez L, Husseini A, Idrisov BT, Ikeda N, Islami F, Jahangir E, Jassal SK, Jee SH, Jeffreys M, Jonas JB, Kabagambe EK, Khalifa SE, Kengne AP, Khader YS, Khang YH, Kim D, Kimokoti RW, Kinge JM, Kokubo Y, Kosen S, Kwan G, Lai T, Leinsalu M, Li Y, Liang X, Liu S, Logroscino G, Lotufo PA, Lu Y, Ma J, Mainoo NK, Mensah GA, Merriman TR, Mokdad AH, Moschandreas J, Naghavi M, Naheed A, Nand D, Narayan KM, Nelson EL, Neuhouser ML, Nisar MI, Ohkubo T, Oti SO, Pedroza A, Prabhakaran D, Roy N, Sampson U, Seo H, Sepanlou SG, Shibuya K, Shiri R, Shiue I, Singh GM, Singh JA, Skirbekk V, Stapelberg NJ, Sturua L, Sykes BL, Tobias M, Tran BX, Trasande L, Toyoshima H, van de Vijver S, Vasankari TJ, Veerman JL, Velasquez-Melendez G, Vlassov VV, Vollset SE, Vos T, Wang C, Wang X, Weiderpass E, Werdecker A, Wright JL, Yang YC, Yatsuya H, Yoon J, Yoon SJ, Zhao Y, Zhou M, Zhu S, Lopez AD, Murray CJ, Gakidou E. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014; 384:766–781. PMID: 24880830.
Article2. Davis B, Wansink B. Fifty years of fat: news coverage of trends that predate obesity prevalence. BMC Public Health. 2015; 15:629. PMID: 26156027.
Article3. Son YJ, Kim J, Park HJ, Park SE, Park CY, Lee WY, Oh KW, Park SW, Rhee EJ. Association of waist-height ratio with diabetes risk: a 4-year longitudinal retrospective study. Endocrinol Metab (Seoul). 2016; 31:127–133. PMID: 26754587.
Article4. Way KL, Hackett DA, Baker MK, Johnson NA. The effect of regular exercise on insulin sensitivity in type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Metab J. 2016; 40:253–271. PMID: 27535644.
Article5. Patterson RE, Frank LL, Kristal AR, White E. A comprehensive examination of health conditions associated with obesity in older adults. Am J Prev Med. 2004; 27:385–390. PMID: 15556738.
Article6. Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003; 289:76–79. PMID: 12503980.
Article7. Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005; 6:67–85. PMID: 15655039.
Article8. Kim SH, Plutzky J. Brown fat and browning for the treatment of obesity and related metabolic disorders. Diabetes Metab J. 2016; 40:12–21. PMID: 26912151.
Article9. Tucker P, Gilliland J. The effect of season and weather on physical activity: a systematic review. Public Health. 2007; 121:909–922. PMID: 17920646.
Article10. O'Hare C, O'Sullivan V, Flood S, Kenny RA. Seasonal and meteorological associations with depressive symptoms in older adults: a geo-epidemiological study. J Affect Disord. 2016; 191:172–179. PMID: 26655862.11. Lewis LK, Maher C, Belanger K, Tremblay M, Chaput JP, Olds T. At the mercy of the gods: associations between weather, physical activity, and sedentary time in children. Pediatr Exerc Sci. 2016; 28:152–163. PMID: 26098393.
Article12. Chin SO, Keum C, Woo J, Park J, Choi HJ, Woo JT, Rhee SY. Successful weight reduction and maintenance by using a smartphone application in those with overweight and obesity. Sci Rep. 2016; 6:34563. PMID: 27819345.
Article13. Ustulin M, Keum C, Woo J, Woo JT, Rhee SY. Effects of climatic variables on weight loss: a global analysis. Sci Rep. 2017; 7:40708. PMID: 28106167.
Article14. Pagoto S, Schneider K, Jojic M, DeBiasse M, Mann D. Evidence-based strategies in weight-loss mobile apps. Am J Prev Med. 2013; 45:576–582. PMID: 24139770.
Article15. Patel R, Sulzberger L, Li G, Mair J, Morley H, Shing MN, O'Leary C, Prakash A, Robilliard N, Rutherford M, Sharpe C, Shie C, Sritharan L, Turnbull J, Whyte I, Yu H, Cleghorn C, Leung W, Wilson N. Smartphone apps for weight loss and smoking cessation: quality ranking of 120 apps. N Z Med J. 2015; 128:73–76.16. World Health Organization. Air pollution. cited 2018 Mar 27. Available from: http://www.who.int/topics/air_pollution/en.17. AirNow. Air quality index (AQI) basics. cited 2018 Mar 27. Available from: https://www.airnow.gov/index.cfm?action=aqibasics.aqi.18. The Weather Company. A weather API designed for developers. cited 2018 Mar 27. Available from: https://www.wunderground.com/weather/api.19. Jacob DJ, Winner DA. Effect of climate change on air quality. Atmos Environ. 2009; 43:51–63.
Article20. Peng RD, Dominici F, Pastor-Barriuso R, Zeger SL, Samet JM. Seasonal analyses of air pollution and mortality in 100 US cities. Am J Epidemiol. 2005; 161:585–594. PMID: 15746475.
Article21. Ridgers ND, Salmon J, Timperio A. Too hot to move? Objectively assessed seasonal changes in Australian children's physical activity. Int J Behav Nutr Phys Act. 2015; 12:77. PMID: 26088561.
Article22. Klenk J, Buchele G, Rapp K, Franke S, Peter R. ActiFE Study Group. Walking on sunshine: effect of weather conditions on physical activity in older people. J Epidemiol Community Health. 2012; 66:474–476. PMID: 21325149.23. Jerrett M, McConnell R, Chang CC, Wolch J, Reynolds K, Lurmann F, Gilliland F, Berhane K. Automobile traffic around the home and attained body mass index: a longitudinal cohort study of children aged 10-18 years. Prev Med. 2010; 50(Suppl 1):S50–S58. PMID: 19850068.
Article24. Rundle A, Hoepner L, Hassoun A, Oberfield S, Freyer G, Holmes D, Reyes M, Quinn J, Camann D, Perera F, Whyatt R. Association of childhood obesity with maternal exposure to ambient air polycyclic aromatic hydrocarbons during pregnancy. Am J Epidemiol. 2012; 175:1163–1172. PMID: 22505764.
Article25. Wei Y, Zhang JJ, Li Z, Gow A, Chung KF, Hu M, Sun Z, Zeng L, Zhu T, Jia G, Li X, Duarte M, Tang X. Chronic exposure to air pollution particles increases the risk of obesity and metabolic syndrome: findings from a natural experiment in Beijing. FASEB J. 2016; 30:2115–2122. PMID: 26891735.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Can Air Pollution Biologically Hinder Efforts to Lose Body Weight?
- Air pollution and climate change: Effects on asthmatic patients
- Effect of air pollution on acute exacerbation of adult asthma in Seoul, Korea
- Air pollution and childhood obesity
- Epidemiologic Methods and Study Designs for Investigating Adverse Health Effects of Ambient Air Pollution