Pediatr Infect Vaccine.
2018 Aug;25(2):61-71. 10.14776/piv.2018.25.e1.
Characteristics and Clinical Correlations of Staphylococcus aureus Discovered in Stools from Children Hospitalized at a Secondary Hospital
- Affiliations
-
- 1Department of Pediatrics, Eulji University Eulji Hospital, Seoul, the Republic of Korea. acet0125@eulji.ac.kr
- 2Department of Pediatrics, Eulji University School of Medicine, Daejeon, the Republic of Korea.
- 3Infectious Disease Team, Seoul Metropolitan Government Research Institute of Public Health and Environment, Seoul, the Republic of Korea.
- KMID: 2418538
- DOI: http://doi.org/10.14776/piv.2018.25.e1
Abstract
- PURPOSE
Research on the clinical role of Staphylococcus aureus as a pathogen in acute gastroenteritis (AGE) in children has been scarce. This study aimed to clarify the prevalence and clinical correlation of S. aureus detection in children with AGE.
METHODS
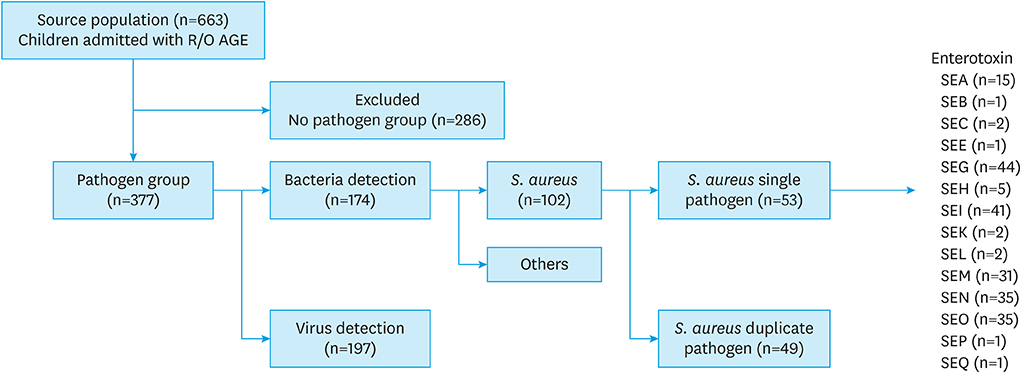
Fecal samples were collected from children with symptoms of AGE who visited a secondary hospital between January 2012 and December 2015. The samples were sent to the Seoul Metropolitan Government Research Institute of Public Health and Environment to test for pathogenic organisms. Clinical patterns were analyzed through medical record review.
RESULTS
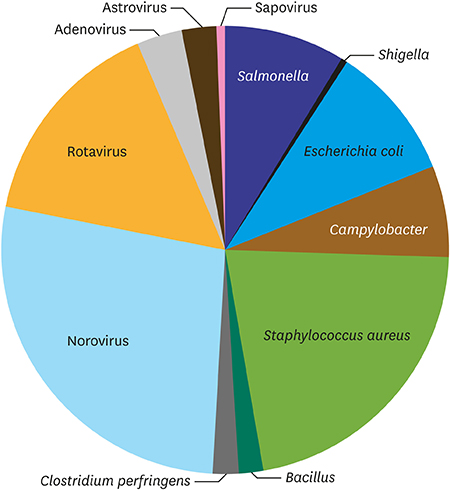
Among the 663 participants, the bacteria detection rate was 26.2% (n=174), the virus detection rate was 29.7% (n=197), and the non-detection rate was 43.1% (n=286). S. aureus was tested positive from 102 cases and was confirmed as a single pathogen in 53 cases. It was the third most common pathogen. The prevalence by age was highest (45.3%) in 0-2 year-olds. Most cases occurred in summer. Symptoms included diarrhea (71.7%), vomiting (67.9%), fever (49.1%), and abdominal pain (37.7%). Only vomiting showed a significant difference between the S. aureus group and the non-detection group (67.9% vs. 43.0%; P=0.001). Among enterotoxins, the higher incidence of vomiting was associated with classical staphylococcal enterotoxins (SEA, SEB, SEC, SED, and SEE) and SEH (P=0.027).
CONCLUSIONS
S. aureus was the bacteria commonly isolated from children with AGE. Our study identified cases of staphylococcal AGE in children based on fecal samples and confirmed the characteristic symptoms, affected age groups, seasonal distribution, and correlation with enterotoxins.
Keyword
MeSH Terms
Figure
Reference
-
1. Bhutta ZA. Acute gastroenteritis in children. In : Kliegman RM, Stanton BF, St Geme JW, Schor NF, editors. Nelson textbook of pediatrics. 20th ed. Philadelphia (PA): Elsevier;2016. p. 1854–1857.2. Le Loir Y, Baron F, Gautier M. Staphylococcus aureus and food poisoning. Genet Mol Res. 2003; 2:63–76.3. Ochoa TJ, Chea-Woo E. Approach to patients with gastrointestinal tract infections and food poisoning. In : Cherry JD, Harrison GJ, Kaplan SL, Steinbach WJ, Hotez PJ, editors. Feigin and Cherry's textbook of pediatric infectious diseases. 8th ed. Philadelphia (PA): Elsevier;2018. p. 450–451.4. Lee JI, Park SH, Kim MS, Oh YH, Yu IS, Choi BH, et al. Surveillance of acute gastroenteritis in Seoul, Korea, during May 2004 and June 2007. J Bacteriol Virol. 2009; 39:363–371.
Article5. Kwun JW, Lee CH. Trends of recent food-borne disease outbreaks in Korea. J Korean Med Assoc. 2007; 50:573–581.
Article6. National Institute of Food and Drug Safety Evaluation (KR). Risk assessment of Staphylococcus aureus and Clostridium perfringens in processed egg products [Internet]. Cheongju: National Institute of Food and Drug Safety Evaluation;2017. cited 2018 Jan 15. Available from: http://www.nifds.go.kr/nifds/02_research/sub_09_10.jsp?mode=view&board_no=197&article_no=11533.7. Kang Y, Yoon S, Jwa S, Lee D, Woo GJ, Park Y, et al. Prevalence of Staphylococcus aureus in Kimbab. J Food Hyg Saf. 2002; 17:31–35.8. Hennekinne JA, De Buyser ML, Dragacci S. Staphylococcus aureus and its food poisoning toxins: characterization and outbreak investigation. FEMS Microbiol Rev. 2012; 36:815–836.
Article9. Pinchuk IV, Beswick EJ, Reyes VE. Staphylococcal enterotoxins. Toxins (Basel). 2010; 2:2177–2197.
Article10. Song JH, Sun DS, Park JS, Choi YJ, Nam HS, Kim YB, et al. Comparison of clinical features of norovirus and rotavirus gastroenteritis in hospitalized children and norovirus genotype analysis. Infect Chemother. 2010; 42:143–148.
Article11. Kim SY, Kim HJ, Shin EH, Eun BW, Ahn YM, Song MO. Etiology and clinical features of acute bacterial gastroenteritis in children managed at a secondary hospital. Pediatr Infect Vaccine. 2017; 24:95–101.
Article12. Chiang YC, Liao WW, Fan CM, Pai WY, Chiou CS, Tsen HY. PCR detection of staphylococcal enterotoxins (SEs) N, O, P, Q, R, U, and survey of SE types in Staphylococcus aureus isolates from food-poisoning cases in Taiwan. Int J Food Microbiol. 2008; 121:66–73.
Article13. Omoe K, Imanishi K, Hu DL, Kato H, Fugane Y, Abe Y, et al. Characterization of novel staphylococcal enterotoxin-like toxin type P. Infect Immun. 2005; 73:5540–5546.
Article14. Dinges MM, Orwin PM, Schlievert PM. Exotoxins of Staphylococcus aureus. Clin Microbiol Rev. 2000; 13:16–34.15. Lin Z, Kotler DP, Schlievert PM, Sordillo EM. Staphylococcal enterocolitis: forgotten but not gone? Dig Dis Sci. 2010; 55:1200–1207.
Article16. Park HS, Han DS. Management of antibiotics-associated diarrhea. Korean J Gastroenterol. 2009; 54:5–12.
Article17. Asha NJ, Tompkins D, Wilcox MH. Comparative analysis of prevalence, risk factors, and molecular epidemiology of antibiotic-associated diarrhea due to Clostridium difficile, Clostridium perfringens, and Staphylococcus aureus . J Clin Microbiol. 2006; 44:2785–2791.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Clinical Study of Staphylococcus Aureus Infection in Children
- Emergence of Superbacteria, Vancomycin-Resistant Staphylococcus Aureus
- Detection of Multidrug Resistant Patterns and Associated - genes of Methicillin Resistant Staphylococcus aureus ( MRSA ) Isolated from Clinical Specimens
- Toxic-Shock Syndrome Toxin in Staphylococcus aureus
- Identification and antimicrobial susceptibility aspects of pathogenic staphylococcus aureus: identification of MRSA by PCR