Korean J Pain.
2018 Jul;31(3):206-214. 10.3344/kjp.2018.31.3.206.
The impact of caudally administrated tramadol on immune response and analgesic efficacy for pediatric patients: a comparative randomized clinical trial
- Affiliations
-
- 1Department of Anesthesia, College of Medicine, Assiut University, Assiut, Egypt. sayed_k_72@yahoo.com
- 2Department of Pediatric, College of Medicine, Assiut University, Assiut, Egypt.
- 3Department of Clinical Pathology, College of Medicine, Assiut University, Assiut, Egypt.
- 4Department of Critical Care and Emergency Nursing, Faculty of Nursing, Assiut University, Assiut, Egypt.
- KMID: 2417959
- DOI: http://doi.org/10.3344/kjp.2018.31.3.206
Abstract
- BACKGROUND
Immune responses appear to be affected by anesthetics and analgesics. We investigated the effects of caudal tramadol on the postoperative immune response and pain management in pediatric patients.
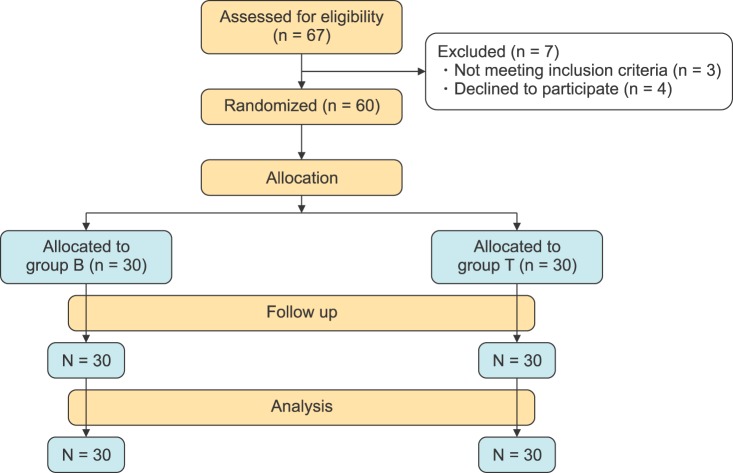
METHODS
Sixty ASA-I pediatric patients aged 3-10 years undergoing lower abdominal surgery. Patients were randomly assigned either to a caudal bupivacaine (0.25%) group (group B), or a group that received caudal tramadol (1 mg/kg) added to the bupivacaine (0.25%) (group T). Both were diluted in a 0.9% NaCl solution to a total volume of 1ml/kg. The systemic immune response was measured by collecting blood samples preoperatively, at the end of anesthesia, and at 24 and 72 hours postoperatively, and studied for interleukin IL-6, C-reactive proteins (CRP) cortisol levels, and leucocytes with its differential count. Postoperative pain was assessed along with sedation scales.
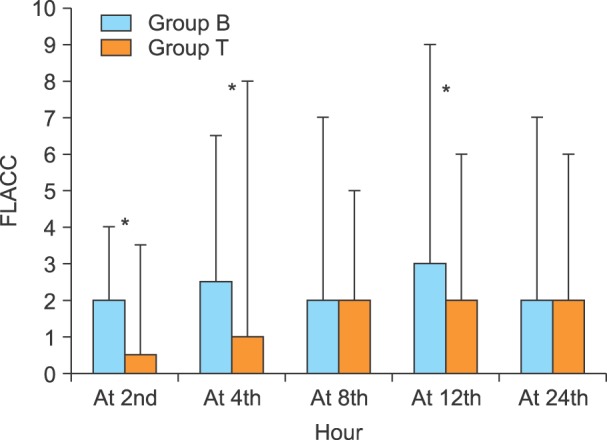
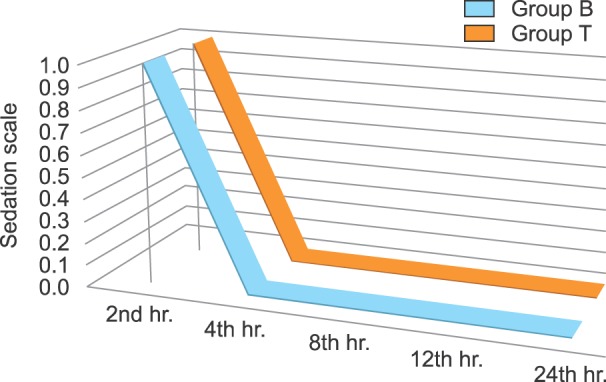
RESULTS
Postoperative production of IL-6 was significantly higher in group B at the end of anesthesia, than at the 24th hour, and at the 72nd hour in group B and group T, respectively. The immune response showed leukocytosis with increased percentages of neutrophil and monocytes, and a decreased lymphocyte response rate within both groups with no significant differences between the groups. Cortisol and CRP were significantly higher in group B.
CONCLUSIONS
Adding tramadol to a caudal bupivacaine block can attenuate the pro-inflammatory cytokine response, Cortisol, and CRP in children undergoing lower abdominal surgery.
Keyword
MeSH Terms
-
Abdomen
Analgesics
Anesthesia
Anesthesia, Caudal
Anesthetics
Bupivacaine
C-Reactive Protein
Child
Humans
Hydrocortisone
Interleukin-6
Interleukins
Leukocyte Count
Leukocytes
Leukocytosis
Lymphocytes
Monocytes
Neutrophils
Pain Management
Pain, Postoperative
Pediatrics
Tramadol*
Weights and Measures
Analgesics
Anesthetics
Bupivacaine
C-Reactive Protein
Hydrocortisone
Interleukin-6
Interleukins
Tramadol
Figure
Reference
-
1. Khan S, Memon MI. Comparison of caudal bupivacaine and bupivacaine-tramadol for postoperative analgesia in children with hypospadias repair. J Coll Physicians Surg Pak. 2008; 18:601–604. PMID: 18940114.2. Stefano GB, Scharrer B, Smith EM, Hughes TK Jr, Magazine HI, Bilfinger TV, et al. Opioid and opiate immunoregulatory processes. Crit Rev Immunol. 1996; 16:109–144. PMID: 8879941.
Article3. Webster NR. Opioids and the immune system. Br J Anaesth. 1998; 81:835–836. PMID: 10211004.
Article4. Carli F, Mayo N, Klubien K, Schricker T, Trudel J, Belliveau P. Epidural analgesia enhances functional exercise capacity and health-related quality of life after colonic surgery: results of a randomized trial. Anesthesiology. 2002; 97:540–549. PMID: 12218518.
Article5. Hole A, Unsgaard G, Breivik H. Monocyte functions are depressed during and after surgery under general anaesthesia but not under epidural anaesthesia. Acta Anaesthesiol Scand. 1982; 26:301–307. PMID: 7124304.
Article6. Hashimoto T, Hashimoto S, Hori Y, Nakagawa H, Hosokawa T. Epidural anaesthesia blocks changes in peripheral lymphocytes subpopulation during gastrectomy for stomach cancer. Acta Anaesthesiol Scand. 1995; 39:294–298. PMID: 7793203.
Article7. Fan S, Zhong JL, Chen WX, Chen WL, Li QX, Wang YY, et al. Postoperative immune response and surgical stress in selective neck dissection: Comparison between endoscopically assisted dissection and open techniques in cT1-2N0 oral squamous cell carcinoma. J Craniomaxillofac Surg. 2017; 45:1112–1116. PMID: 28679471.
Article8. Shakhar G, Ben-Eliyahu S. Potential prophylactic measures against postoperative immunosuppression: could they reduce recurrence rates in oncological patients? Ann Surg Oncol. 2003; 10:972–992. PMID: 14527919.
Article9. Raghavan S, Harvey AD, Humble SR. New opioid side effects and implications for long-term therapy. Trends Anaesth Crit Care. 2011; 1:18–21.
Article10. Volk T, Schenk M, Voigt K, Tohtz S, Putzier M, Kox WJ. Postoperative epidural anesthesia preserves lymphocyte, but not monocyte, immune function after major spine surgery. Anesth Analg. 2004; 98:1086–1092. PMID: 15041604.
Article11. Lönnqvist PA, Ivani G, Moriarty T. Use of caudal- epidural opioids in children: still state of the art or the beginning of the end. Paediatr Anaesth. 2002; 12:747–749. PMID: 12519132.12. Snyder GL, Greenberg S. Effect of anaesthetic technique and other perioperative factors on cancer recurrence. Br J Anaesth. 2010; 105:106–115. PMID: 20627881.
Article13. Jensen KB, Lonsdorf TB, Schalling M, Kosek E, Ingvar M. Increased sensitivity to thermal pain following a single opiate dose is influenced by the COMT val (158)met polymorphism. PLoS One. 2009; 4:e6016. PMID: 19547755.14. Niesters M, Proto PL, Aarts L, Sarton EY, Drewes AM, Dahan A. Tapentadol potentiates descending pain inhibition in chronic pain patients with diabetic polyneuropathy. Br J Anaesth. 2014; 113:148–156. PMID: 24713310.
Article15. Merkel SI, Voepel-Lewis T, Shayevitz JR, Malviya S. The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurs. 1997; 23:293–297. PMID: 9220806.16. Liu YM, Zhu SM, Wang KR, Feng ZY, Chen QL. Effect of tramadol on immune responses and nociceptive thresholds in a rat model of incisional pain. J Zhejiang Univ Sci B. 2008; 9:895–902. PMID: 18988309.
Article17. Zhou LW, Ding HL, Li MQ, Jin S, Wang XS, Ji LJ. Effect of tramadol on perioperative immune function in patients undergoing gastric cancer surgeries. Anesth Essays Res. 2013; 7:54–57. PMID: 25885721.
Article18. Sacerdote P, Bianchi M, Gaspani L, Manfredi B, Maucione A, Terno G, et al. The effects of tramadol and morphine on immune responses and pain after surgery in cancer patients. Anesth Analg. 2000; 90:1411–1414. PMID: 10825330.
Article19. Liu Z, Gao F, Tian Y. Effects of morphine, fentanyl and tramadol on human immune response. J Huazhong Univ Sci Technolog Med Sci. 2006; 26:478–481. PMID: 17120754.
Article20. Watkins LR, Maier SF, Goehler LE. Immune activation: the role of pro-inflammatory cytokines in inflammation, illness responses and pathological pain states. Pain. 1995; 63:289–302. PMID: 8719529.
Article21. Senel AC, Akyol A, Dohman D, Solak M. Caudal bupivacaine-tramadol combination for postoperative analgesia in pediatric herniorrhaphy. Acta Anaesthesiol Scand. 2001; 45:786–789. PMID: 11421842.
Article22. Prakash S, Tyagi R, Gogia AR, Singh R, Prakash S. Efficacy of three doses of tramadol with bupivacaine for caudal analgesia in paediatric inguinal herniotomy. Br J Anaesth. 2006; 97:385–388. PMID: 16798773.
Article23. Lloyd-Thomas AR. Pain management in paediatric patients. Br J Anaesth. 1990; 64:85–104. PMID: 2405898.
Article24. Wolf AR, Hughes D, Wade A, Mather SJ, Prys-Roberts C. Postoperative analgesia after paediatric orchidopexy: evaluation of a bupivacaine-morphine mixture. Br J Anaesth. 1990; 64:430–435. PMID: 1970738.
Article25. de Beer DA, Thomas ML. Caudal additives in children-solutions or problems? Br J Anaesth. 2003; 90:487–498. PMID: 12644422.
Article26. Kumar P, Rudra A, Pan AK, Acharya A. Caudal additives in pediatrics: a comparison among midazolam, ketamine, and neostigmine coadministered with bupivacaine. Anesth Analg. 2005; 101:69–73. PMID: 15976208.
Article27. Girwalkar-Bagle A, Thatte W, Choudhari S. Preemptive caudal anaesthesia in children with bupivacaine- tramadol and levobupivacaine-tramadol: a randomized, double-blind, prospective study. Anaesth Pain Intensive Care. 2015; 19:13–19.28. Güneş Y, Gündüz M, Unlügenç H, Ozalevli M, Ozcengiz D. Comparison of caudal vs intravenous tramadol administered either preoperatively or postoperatively for pain relief in boys. Paediatr Anaesth. 2004; 14:324–328. PMID: 15078378.
Article29. Prosser DP, Davis A, Booker PD, Murray A. Caudal tramadol for postoperative analgesia in pediatric hypospadias surgery. Br J Anaesth. 1997; 79:293–296. PMID: 9389843.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pre-emptive analgesia efficacy of piroxicam versus tramadol in oral surgery
- Comparison of tramadol/acetaminophen and codeine/acetaminophen/ibuprofen in onset of analgesia and analgesic efficacy for postoperative acute pain
- Comparative Study of the Safety and Effectiveness of Tramadol 37.5 mg/Acetaminophen 325 mg Combined Tablets and Cyclo-Oxygenase-2 (Celecoxib) Inhibitor for the Treatment of Chronic Low Back Pain: A Multicenter, Randomized, Comparative Clinical Study
- Continuous Epidural Infusion of Bupivacaine with Tramadol for Post - Cesarean Analgesia
- Comparison of single-dose nalbuphine versus tramadol for postoperative pain management in children: a randomized, controlled trial