Korean J Pain.
2018 Jul;31(3):191-198. 10.3344/kjp.2018.31.3.191.
Comparison of patient-controlled epidural analgesia with patient-controlled intravenous analgesia for laparoscopic radical prostatectomy
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, Biomedical Research Institute, Pusan National University Hospital, Busan, Korea. jykwon@pusan.ac.kr
- KMID: 2417957
- DOI: http://doi.org/10.3344/kjp.2018.31.3.191
Abstract
- BACKGROUND
Patient-controlled epidural analgesia (PCEA) is known to provide good postoperative analgesia in many types of surgery including laparoscopic surgery. However, no study has compared PCEA with patient-controlled intravascular analgesia (PCIA) in laparoscopic radical prostatectomy (LARP). In this study, the efficacy and side effects of PCEA and PCIA after LARP were compared.
METHODS
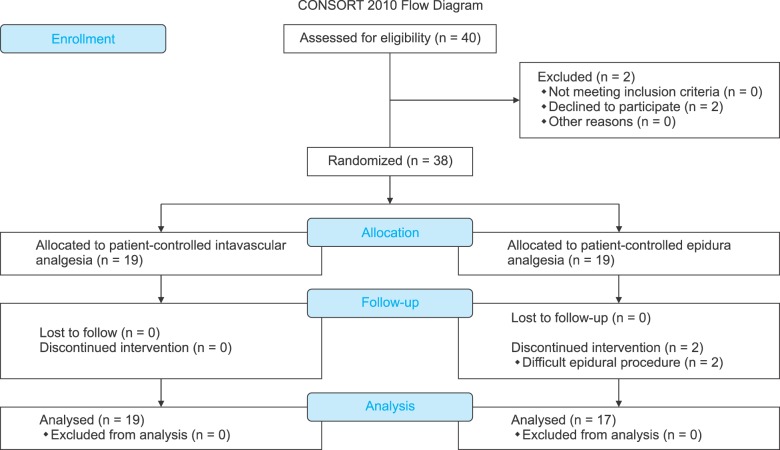
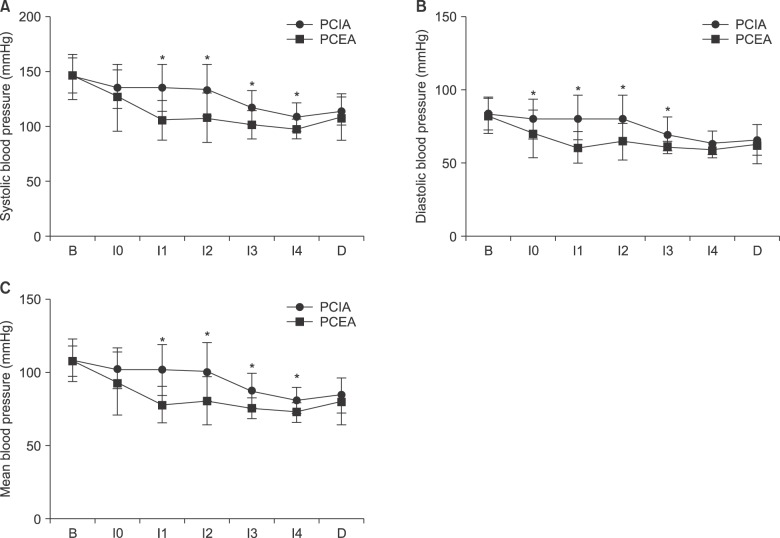
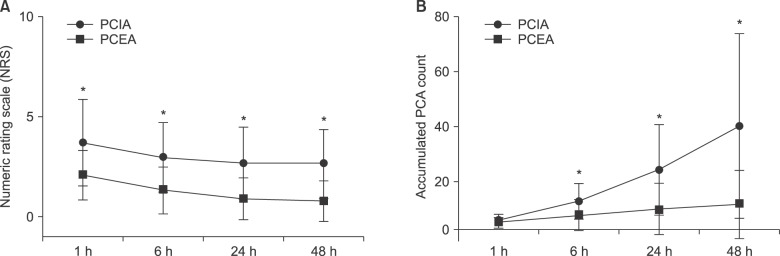
Forty patients undergoing LARP were randomly divided into two groups: 1) a PCEA group, treated with 0.2% ropivacaine 3 ml and 0.1 mg morphine in the bolus; and 2) a PCIA group, treated with oxycodone 1 mg and nefopam 1 mg in the bolus. After the operation, a blinded observer assessed estimated blood loss (EBL), added a dose of rocuronium, performed transfusion, and added analgesics. The numeric rating scale (NRS), infused PCA dose, and side effects were assessed at 1, 6, 24, and 48 h.
RESULTS
EBL, added rocuronium, and added analgesics in the PCEA group were less than those in the PCIA group. There were no significant differences in side-effects after the operation between the two groups. Patients were more satisfied with PCEA than with PCIA. The NRS and accumulated PCA count were lower in PCEA group.
CONCLUSIONS
Combined thoracic epidural anesthesia could induce less blood loss during operations. PCEA showed better postoperative analgesia and greater patient satisfaction than PCIA. Thus, PCEA may be a more useful analgesic method than PICA after LARP.
Keyword
MeSH Terms
-
Administration, Intravenous
Analgesia*
Analgesia, Epidural*
Analgesia, Patient-Controlled
Analgesics
Anesthesia, Epidural
Humans
Injections, Epidural
Laparoscopes
Laparoscopy
Methods
Morphine
Nefopam
Oxycodone
Pain Measurement
Pain, Postoperative
Passive Cutaneous Anaphylaxis
Patient Satisfaction
Pica
Prostatectomy*
Thoracic Vertebrae
Analgesics
Morphine
Nefopam
Oxycodone
Figure
Cited by 1 articles
-
The effect of atropine in preventing catheter-related pain and discomfort in patients undergoing transurethral resection due to bladder tumor; prospective randomized, controlled study
Yeliz Şahiner, Yeliz Şahiner, Arzu Akdağlı Ekici, Musa Ekici, Emre Demir
Korean J Pain. 2020;33(2):176-182. doi: 10.3344/kjp.2020.33.2.176.
Reference
-
1. Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011; 61:212–236. PMID: 21685461.2. Laufenberg-Feldmann R, Kappis B, Mauff S, Schmidtmann I, Ferner M. Prevalence of pain 6 months after surgery: a prospective observational study. BMC Anesthesiol. 2016; 16:91. PMID: 27724844.
Article3. Chen K, Xu XW, Zhang RC, Pan Y, Wu D, Mou YP. Systematic review and meta-analysis of laparoscopy-assisted and open total gastrectomy for gastric cancer. World J Gastroenterol. 2013; 19:5365–5376. PMID: 23983442.
Article4. Bisgaard T, Klarskov B, Rosenberg J, Kehlet H. Characteristics and prediction of early pain after laparoscopic cholecystectomy. Pain. 2001; 90:261–269. PMID: 11207398.
Article5. Hudcova J, McNicol E, Quah C, Lau J, Carr DB. Patient controlled opioid analgesia versus conventional opioid analgesia for postoperative pain. Cochrane Database Syst Rev. 2006; CD003348. PMID: 17054167.
Article6. Capdevila X, Moulard S, Plasse C, Peshaud JL, Molinari N, Dadure C, et al. Effectiveness of epidural analgesia, continuous surgical site analgesia, and patient-controlled analgesic morphine for postoperative pain management and hyperalgesia, rehabilitation, and health-related quality of life after open nephrectomy: a prospective, randomized, controlled study. Anesth Analg. 2017; 124:336–345. PMID: 27918333.
Article7. Oh YJ, Lee JR, Choi YS, Koh SO, Na S. Randomized controlled comparison of combined general and epidural anesthesia versus general anesthesia on diaphragmatic function after laparoscopic prostatectomy. Minerva Anestesiol. 2013; 79:1371–1380. PMID: 23857436.8. Webster TM, Herrell SD, Chang SS, Cookson MS, Baumgartner RG, Anderson LW, et al. Robotic assisted laparoscopic radical prostatectomy versus retropubic radical prostatectomy: a prospective assessment of postoperative pain. J Urol. 2005; 174:912–914. PMID: 16093986.
Article9. Joshi GP, Jaschinski T, Bonnet F, Kehlet H. PROSPECT Collaboration. Optimal pain management for radical prostatectomy surgery: what is the evidence? BMC Anesthesiol. 2015; 15:159. PMID: 26530113.
Article10. Mir MC, Joseph B, Zhao R, Bolton DM, Gyomber D, Lawrentschuk N. Effectiveness of epidural versus alternate analgesia for pain relief after radical prostatectomy and correlation with biochemical recurrence in men with prostate cancer. Res Rep Urol. 2013; 5:139–145. PMID: 24400245.11. Wheatley RG, Schug SA, Watson D. Safety and efficacy of postoperative epidural analgesia. Br J Anaesth. 2001; 87:47–61. PMID: 11460813.
Article12. Carvalho B, George RB, Cobb B, McKenzie C, Riley ET. Implementation of programmed intermittent epidural bolus for the maintenance of labor analgesia. Anesth Analg. 2016; 123:965–971. PMID: 27464978.
Article13. Doyle E, Robinson D, Morton NS. Comparison of patient-controlled analgesia with and without a background infusion after lower abdominal surgery in children. Br J Anaesth. 1993; 71:670–673. PMID: 8251277.
Article14. Hwang BY, Kwon JY, Lee DW, Kim E, Kim TK, Kim HK. A randomized clinical trial of nefopam versus ketorolac combined with oxycodone in patient-controlled analgesia after gynecologic surgery. Int J Med Sci. 2015; 12:644–649. PMID: 26283884.
Article15. Royse CE, Royse AG, Deelen DA. An audit of morphine versus fentanyl as an adjunct to ropivacaine 0.2% for high thoracic epidural analgesia. Anaesth Intensive Care. 2005; 33:639–644. PMID: 16235484.
Article16. Delvecchio L, Bettinelli S, Klersy C, Allegri M, Cavalloro F, Braschi A. Comparing the efficacy and safety of continuous epidural analgesia in abdominal and urological surgery between two opioids with different kinetic properties: morphine and sufentanyl. Minerva Anestesiol. 2008; 74:69–76. PMID: 18288069.17. Agarwal A, Pandey R, Dhiraaj S, Singh PK, Raza M, Pandey CK, et al. The effect of epidural bupivacaine on induction and maintenance doses of propofol (evaluated by bispectral index) and maintenance doses of fentanyl and vecuronium. Anesth Analg. 2004; 99:1684–1688. PMID: 15562054.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Postoperative Analgesia and Side Effects by Patient-Controlled Epidural and Intravenous Analgesia after Cesarean Section
- Modern techniques to optimize neuraxial labor analgesia
- Efficacy of Nei-Guan acupressure on Nausea and Vomiting in Patients undergoing laparoscopic prostatectomy with Intravenous Patient Controlled Analgesia
- Labor Analgesia
- Post-thoracotomy Analgesia & ICU Length of Stay: Comparison of Thoracic Epidrual Morphine Infusion and Lumbar Epidural Plus Intravenous Morphine Infusion