Korean J Pain.
2018 Jul;31(3):155-173. 10.3344/kjp.2018.31.3.155.
Chronic postsurgical pain: current evidence for prevention and management
- Affiliations
-
- 1Department of Anaesthesiology and Critical Care, B. P. Koirala Institute of Health Sciences, Dharan, Nepal.
- 2Department of Anesthesiology, Siriraj Hospital, Mahidol University, Bangkok, Thailand. pramoteo@hotmail.com
- KMID: 2417954
- DOI: http://doi.org/10.3344/kjp.2018.31.3.155
Abstract
- Chronic postsurgical pain (CPSP) is an unwanted adverse event in any operation. It leads to functional limitations and psychological trauma for patients, and leaves the operative team with feelings of failure and humiliation. Therefore, it is crucial that preventive strategies for CPSP are considered in high-risk operations. Various techniques have been implemented to reduce the risk with variable success. Identifying the risk factors for each patient and applying a timely preventive strategy may help patients avoid the distress of chronic pain. The preventive strategies include modification of the surgical technique, good pain control throughout the perioperative period, and preoperative psychological intervention focusing on the psychosocial and cognitive risk factors. Appropriate management of CPSP patients is also necessary to reduce their suffering. CPSP usually has a neuropathic pain component; therefore, the current recommendations are based on data on chronic neuropathic pain. Hence, voltage-dependent calcium channel antagonists, antidepressants, topical lidocaine and topical capsaicin are the main pharmacological treatments. Paracetamol, NSAIDs and weak opioids can be used according to symptom severity, but strong opioids should be used with great caution and are not recommended. Other drugs that may be helpful are ketamine, clonidine, and intravenous lidocaine infusion. For patients with failed pharmacological treatment, consideration should be given to pain interventions; examples include transcutaneous electrical nerve stimulation, botulinum toxin injections, pulsed radiofrequency, nerve blocks, nerve ablation, neuromodulation and surgical management. Physical therapy, cognitive behavioral therapy and lifestyle modifications are also useful for relieving the pain and distress experienced by CPSP patients.
Keyword
MeSH Terms
-
Acetaminophen
Analgesics, Opioid
Anti-Inflammatory Agents, Non-Steroidal
Antidepressive Agents
Botulinum Toxins
Calcium Channel Blockers
Capsaicin
Chronic Pain
Clonidine
Cognitive Therapy
Drug Therapy
Humans
Incidence
Ketamine
Lidocaine
Life Style
Nerve Block
Neuralgia
Pain Management
Pain, Intractable
Pain, Postoperative
Perioperative Period
Physical Therapy Modalities
Psychological Trauma
Risk Factors
Surgical Procedures, Operative
Transcutaneous Electric Nerve Stimulation
Acetaminophen
Analgesics, Opioid
Anti-Inflammatory Agents, Non-Steroidal
Antidepressive Agents
Botulinum Toxins
Calcium Channel Blockers
Capsaicin
Clonidine
Ketamine
Lidocaine
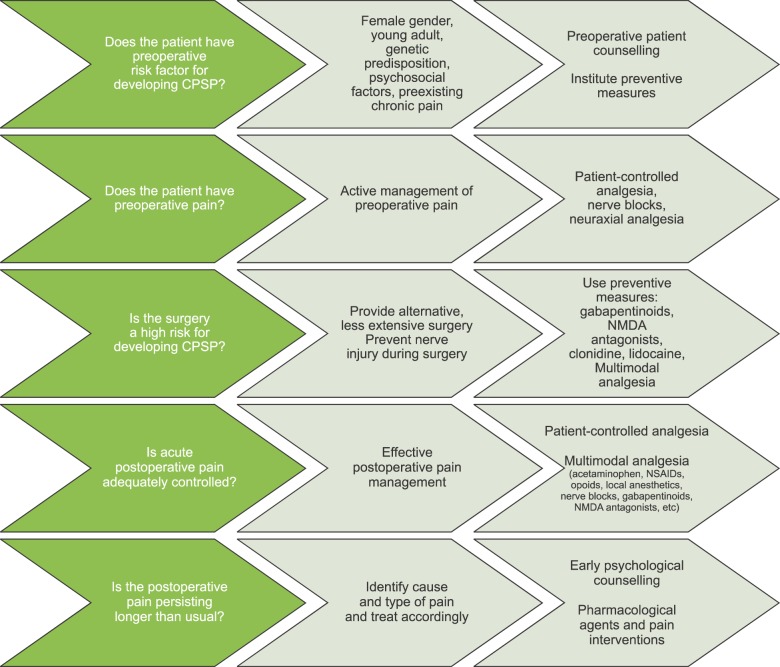
Figure
Cited by 2 articles
-
Perioperative stress prolong post-surgical pain via miR-339-5p targeting oprm1 in the amygdala
Yi Zhu, Mei Sun, Peng Liu, Weidong Shao, Ming Xiong, Bo Xu
Korean J Pain. 2022;35(4):423-432. doi: 10.3344/kjp.2022.35.4.423.A randomized double-blind controlled study comparing erector spinae plane block and thoracic paravertebral block for postoperative analgesia after breast surgery
Aumjit Wittayapairoj, Nattanan Sinthuchao, Ongart Somintara, Viriya Thincheelong, Wilawan Somdee
Anesth Pain Med. 2022;17(4):445-453. doi: 10.17085/apm.22157.
Reference
-
1. Macrae WA, Davies HT. Chronic postsurgical pain. In : Crombie IK, Linton S, Croft P, Von Korff M, LeResche L, editors. Epidemiology of pain. Seattle, WA: IASP Press;1999. p. 125–142.3. Werner MU, Kongsgaard UE. I. Defining persistent postsurgical pain: is an update required? Br J Anaesth. 2014; 113:1–4. PMID: 24554546.
Article4. Fletcher D, Stamer UM, Pogatzki-Zahn E, Zaslansky R, Tanase NV, Perruchoud C, et al. Chronic postsurgical pain in Europe: an observational study. Eur J Anaesthesiol. 2015; 32:725–734. PMID: 26241763.5. Schug SA, Pogatzki-Zahn EM. Chronic pain after surgery or injury. Pain: clinical updates. Washington, D.C.: International Association for the Study of Pain;2011. p. 19.6. Saxena AK, Chilkoti GT, Chopra AK, Banerjee BD, Sharma T. Chronic persistent post-surgical pain following staging laparotomy for carcinoma of ovary and its relationship to signal transduction genes. Korean J Pain. 2016; 29:239–248. PMID: 27738502.
Article8. Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006; 367:1618–1625. PMID: 16698416.
Article9. Alfieri S, Rotondi F, Di Giorgio A, Fumagalli U, Salzano A, Di Miceli D, et al. Influence of preservation versus division of ilioinguinal, iliohypogastric, and genital nerves during open mesh herniorrhaphy: prospective multicentric study of chronic pain. Ann Surg. 2006; 243:553–558. PMID: 16552209.
Article10. McCormack K, Scott NW, Go PM, Ross S, Grant AM. EU Hernia Trialists Collaboration. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev. 2003; CD001785. PMID: 12535413.
Article11. Karthikesalingam A, Markar SR, Holt PJ, Praseedom RK. Meta-analysis of randomized controlled trials comparing laparoscopic with open mesh repair of recurrent inguinal hernia. Br J Surg. 2010; 97:4–11. PMID: 20013926.
Article12. Bignell M, Partridge G, Mahon D, Rhodes M. Prospective randomized trial of laparoscopic (transabdominal preperitoneal-TAPP) versus open (mesh) repair for bilateral and recurrent inguinal hernia: incidence of chronic groin pain and impact on quality of life: results of 10 year follow-up. Hernia. 2012; 16:635–640. PMID: 22767210.
Article13. Recker DC, Perry PM. Postsurgical pain syndromes: Chronic pain after hysterectomy and cesarean section. Tech Reg Anesth Pain Manage. 2011; 15:133–139.
Article14. Brandsborg B. Pain following hysterectomy: epidemiological and clinical aspects. Dan Med J. 2012; 59:B4374. PMID: 22239844.15. Gottschalk A, Cohen SP, Yang S, Ochroch EA. Preventing and treating pain after thoracic surgery. Anesthesiology. 2006; 104:594–600. PMID: 16508407.
Article16. Vilardo L, Shah M. Chronic pain after hip and knee replacement. Tech Reg Anesth Pain Manage. 2011; 15:110–115.
Article17. Huang AP, Sakata RK. Pain after sternotomy - review. Braz J Anesthesiol. 2016; 66:395–401. PMID: 27343790.
Article18. Kraychete DC, Sakata RK, Lannes LO, Bandeira ID, Sadatsune EJ. Postoperative persistent chronic pain: what do we know about prevention, risk factors, and treatment. Braz J Anesthesiol. 2016; 66:505–512. PMID: 27591465.
Article19. Jung BF, Ahrendt GM, Oaklander AL, Dworkin RH. Neuropathic pain following breast cancer surgery: proposed classification and research update. Pain. 2003; 104:1–13. PMID: 12855309.
Article20. Clarke H, Woodhouse LJ, Kennedy D, Stratford P, Katz J. Strategies aimed at preventing chronic post-surgical pain: comprehensive perioperative pain management after total joint replacement surgery. Physiother Can. 2011; 63:289–304. PMID: 22654235.
Article21. Reddi D. Preventing chronic postoperative pain. Anaesthesia. 2016; 71(Suppl 1):64–71. PMID: 26620149.
Article22. Karanikolas M, Aretha D, Tsolakis I, Monantera G, Kiekkas P, Papadoulas S, et al. Optimized perioperative analgesia reduces chronic phantom limb pain intensity, prevalence, and frequency: a prospective, randomized, clinical trial. Anesthesiology. 2011; 114:1144–1154. PMID: 21368651.
Article23. Buvanendran A. Multimodal analgesia for perioperative pain management. IARS 2011 review course lectures. Washington, D.C.: International Association for the Study of Pain;2011.24. Albi-Feldzer A, Mouret-Fourme EE, Hamouda S, Motamed C, Dubois PY, Jouanneau L, et al. A double-blind randomized trial of wound and intercostal space infiltration with ropivacaine during breast cancer surgery: effects on chronic postoperative pain. Anesthesiology. 2013; 118:318–326. PMID: 23340351.
Article25. Andreae MH, Andreae DA. Regional anaesthesia to prevent chronic pain after surgery: a Cochrane systematic review and meta-analysis. Br J Anaesth. 2013; 111:711–720. PMID: 23811426.
Article26. Borghi B, D'Addabbo M, White PF, Gallerani P, Toccaceli L, Raffaeli W, et al. The use of prolonged peripheral neural blockade after lower extremity amputation: the effect on symptoms associated with phantom limb syndrome. Anesth Analg. 2010; 111:1308–1315. PMID: 20881281.
Article27. Van de Ven TJ, John Hsia HL. Causes and prevention of chronic postsurgical pain. Curr Opin Crit Care. 2012; 18:366–371. PMID: 22732437.
Article28. Humble SR, Dalton AJ, Li L. A systematic review of therapeutic interventions to reduce acute and chronic postsurgical pain after amputation, thoracotomy or mastectomy. Eur J Pain. 2015; 19:451–465. PMID: 25088289.
Article29. Clarke H, Bonin RP, Orser BA, Englesakis M, Wijeysundera DN, Katz J. The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. Anesth Analg. 2012; 115:428–442. PMID: 22415535.
Article30. Sentürk M, Ozcan PE, Talu GK, Kiyan E, Camci E, Ozyalçin S, et al. The effects of three different analgesia techniques on long-term postthoracotomy pain. Anesth Analg. 2002; 94:11–15. PMID: 11772793.
Article31. Gupta A, Gandhi K, Viscusi ER. Persistent postsurgical pain after abdominal surgery. Tech Reg Anesth Pain Manage. 2011; 15:140–146.
Article32. Clarke H, Poon M, Weinrib A, Katznelson R, Wentlandt K, Katz J. Preventive analgesia and novel strategies for the prevention of chronic post-surgical pain. Drugs. 2015; 75:339–351. PMID: 25752774.
Article33. Fassoulaki A, Triga A, Melemeni A, Sarantopoulos C. Multimodal analgesia with gabapentin and local anesthetics prevents acute and chronic pain after breast surgery for cancer. Anesth Analg. 2005; 101:1427–1432. PMID: 16244006.
Article34. Mishriky BM, Waldron NH, Habib AS. Impact of pregabalin on acute and persistent postoperative pain: a systematic review and meta-analysis. Br J Anaesth. 2015; 114:10–31. PMID: 25209095.
Article35. Schmidt PC, Ruchelli G, Mackey SC, Carroll IR. Perioperative gabapentinoids: choice of agent, dose, timing, and effects on chronic postsurgical pain. Anesthesiology. 2013; 119:1215–1221. PMID: 24051389.36. Martinez V, Pichard X, Fletcher D. Perioperative pregabalin administration does not prevent chronic postoperative pain: systematic review with a meta-analysis of randomized trials. Pain. 2017; 158:775–783. PMID: 28296652.
Article37. Amr YM, Yousef AA. Evaluation of efficacy of the perioperative administration of Venlafaxine or gabapentin on acute and chronic postmastectomy pain. Clin J Pain. 2010; 26:381–385. PMID: 20473044.
Article38. Wong K, Phelan R, Kalso E, Galvin I, Goldstein D, Raja S, et al. Antidepressant drugs for prevention of acute and chronic postsurgical pain: early evidence and recommended future directions. Anesthesiology. 2014; 121:591–608. PMID: 25222675.
Article39. McGreevy K, Bottros MM, Raja SN. Preventing chronic pain following acute pain: risk factors, preventive strategies, and their efficacy. Eur J Pain Suppl. 2011; 5:365–372. PMID: 22102847.
Article40. McNicol ED, Schumann R, Haroutounian S. A systematic review and meta-analysis of ketamine for the prevention of persistent post-surgical pain. Acta Anaesthesiol Scand. 2014; 58:1199–1213. PMID: 25060512.
Article41. Grigoras A, Lee P, Sattar F, Shorten G. Perioperative intravenous lidocaine decreases the incidence of persistent pain after breast surgery. Clin J Pain. 2012; 28:567–572. PMID: 22699129.
Article42. Chaparro LE, Smith SA, Moore RA, Wiffen PJ, Gilron I. Pharmacotherapy for the prevention of chronic pain after surgery in adults. Cochrane Database Syst Rev. 2013; CD008307. PMID: 23881791.
Article43. Fransen M, Anderson C, Douglas J, MacMahon S, Neal B, Norton R, et al. Safety and efficacy of routine postoperative ibuprofen for pain and disability related to ectopic bone formation after hip replacement surgery (HIPAID): randomised controlled trial. BMJ. 2006; 333:519. PMID: 16885182.
Article44. Reuben SS, Ekman EF. The effect of initiating a preventive multimodal analgesic regimen on long-term patient outcomes for outpatient anterior cruciate ligament reconstruction surgery. Anesth Analg. 2007; 105:228–232. PMID: 17578979.
Article45. Weis F, Kilger E, Roozendaal B, de Quervain DJ, Lamm P, Schmidt M, et al. Stress doses of hydrocortisone reduce chronic stress symptoms and improve health-related quality of life in high-risk patients after cardiac surgery: a randomized study. J Thorac Cardiovasc Surg. 2006; 131:277–282. PMID: 16434254.
Article46. Nielsen RV, Fomsgaard J, Mathiesen O, Dahl JB. The effect of preoperative dexamethasone on pain 1 year after lumbar disc surgery: a follow-up study. BMC Anesthesiol. 2016; 16:112. PMID: 27852230.47. Hinrichs-Rocker A, Schulz K, Järvinen I, Lefering R, Simanski C, Neugebauer EA. Psychosocial predictors and correlates for chronic post-surgical pain (CPSP) - a systematic review. Eur J Pain. 2009; 13:719–730. PMID: 18952472.
Article48. Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain: risk factors and protective factors. Expert Rev Neurother. 2009; 9:723–744. PMID: 19402781.
Article50. Derry S, Moore RA. Topical capsaicin (low concentration) for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2012; CD010111. PMID: 22972149.
Article51. Derry S, Rice AS, Cole P, Tan T, Moore RA. Topical capsaicin (high concentration) for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2017; CD007393. PMID: 28085183.
Article52. Fleming JA, O'Connor BD. Use of lidocaine patches for neuropathic pain in a comprehensive cancer centre. Pain Res Manag. 2009; 14:381–388. PMID: 19862373.
Article53. Nicolaou A, Nicholson B, Hans G, Brasseur L. Outcome predictors for treatment success with 5% lidocaine medicated plaster in low back pain with neuropathic components and neuropathic pain after surgical and nonsurgical trauma. J Pain Res. 2011; 4:25–38. PMID: 21386952.54. Correa-Illanes G, Roa R, Piñeros JL, Calderón W. Use of 5% lidocaine medicated plaster to treat localized neuropathic pain secondary to traumatic injury of peripheral nerves. Local Reg Anesth. 2012; 5:47–53. PMID: 23152700.55. Hans G, Joukes E, Verhulst J, Vercauteren M. Management of neuropathic pain after surgical and non-surgical trauma with lidocaine 5% patches: study of 40 consecutive cases. Curr Med Res Opin. 2009; 25:2737–2743. PMID: 19788351.
Article56. Bischoff JM, Petersen M, Uçeyler N, Sommer C, Kehlet H, Werner MU. Lidocaine patch (5%) in treatment of persistent inguinal postherniorrhaphy pain: a randomized, doubleblind, placebo-controlled, crossover trial. Anesthesiology. 2013; 119:1444–1452. PMID: 23887198.
Article57. Glantz L, Godovic G, Lekar M, Kramer M, Eidelman LA. Efficacy of transdermal nitroglycerin combined with etodolac for the treatment of chronic post-thoracotomy pain: an open-label prospective clinical trial. J Pain Symptom Manage. 2004; 27:277–281. PMID: 15038339.
Article58. Ho KY, Huh BK, White WD, Yeh CC, Miller EJ. Topical amitriptyline versus lidocaine in the treatment of neuropathic pain. Clin J Pain. 2008; 24:51–55. PMID: 18180637.
Article59. Lynch ME, Clark AJ, Sawynok J. A pilot study examining topical amitriptyline, ketamine, and a combination of both in the treatment of neuropathic pain. Clin J Pain. 2003; 19:323–328. PMID: 12966259.
Article60. Lynch ME, Clark AJ, Sawynok J, Sullivan MJ. Topical amitriptyline and ketamine in neuropathic pain syndromes: an open-label study. J Pain. 2005; 6:644–649. PMID: 16202956.
Article61. Abdi S, Datta S, Trescot AM, Schultz DM, Adlaka R, Atluri SL, et al. Epidural steroids in the management of chronic spinal pain: a systematic review. Pain Physician. 2007; 10:185–212. PMID: 17256030.62. Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. Management of pain of post lumbar surgery syndrome: one-year results of a randomized, double-blind, active controlled trial of fluoroscopic caudal epidural injections. Pain Physician. 2010; 13:509–521. PMID: 21102963.63. Manchikanti L, Malla Y, Cash KA, McManus CD, Pampati V. Fluoroscopic cervical interlaminar epidural injections in managing chronic pain of cervical postsurgery syndrome: preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012; 15:13–25. PMID: 22270734.64. Sharpstone D, Colin-Jones DG. Chronic, non-visceral abdominal pain. Gut. 1994; 35:833–836. PMID: 8020814.
Article65. Guirguis MN, Abd-Elsayed AA, Girgis G, Soliman LM. Ultrasound-guided transversus abdominis plane catheter for chronic abdominal pain. Pain Pract. 2013; 13:235–238. PMID: 22734804.
Article66. Lindsetmo RO, Stulberg J. Chronic abdominal wall pain--a diagnostic challenge for the surgeon. Am J Surg. 2009; 198:129–134. PMID: 19555786.
Article67. Wang LK, Chen HP, Chang PJ, Kang FC, Tsai YC. Axillary brachial plexus block with patient controlled analgesia for complex regional pain syndrome type I: a case report. Reg Anesth Pain Med. 2001; 26:68–71. PMID: 11172515.
Article68. Fabregat G, Asensio-Samper JM, Palmisani S, Villanueva-Pérez VL, De Andrés J. Subcutaneous botulinum toxin for chronic post-thoracotomy pain. Pain Pract. 2013; 13:231–234. PMID: 22716282.
Article69. Smoot D, Zielinski M, Jenkins D, Schiller H. Botox A injection for pain after laparoscopic ventral hernia: a case report. Pain Med. 2011; 12:1121–1123. PMID: 21668748.
Article70. Argoff CE. A focused review on the use of botulinum toxins for neuropathic pain. Clin J Pain. 2002; 18:S177–S181. PMID: 12569966.
Article71. Ganapathy S, Brookes J. Chronic postsurgical pain after nonarthroplasty orthopedic surgery. Tech Reg Anesth Pain Manage. 2011; 15:116–123.
Article72. Ramanavarapu V, Simopoulos TT. Pulsed radiofrequency of lumbar dorsal root ganglia for chronic post-amputation stump pain. Pain Physician. 2008; 11:561–566. PMID: 18690285.73. Manchikanti L, Singh V. Managing phantom pain. Pain Physician. 2004; 7:365–375. PMID: 16858476.
Article74. Stolker RJ, Vervest AC, Groen GJ. The treatment of chronic thoracic segmental pain by radiofrequency percutaneous partial rhizotomy. J Neurosurg. 1994; 80:986–992. PMID: 8189279.
Article75. Cohen SP, Sireci A, Wu CL, Larkin TM, Williams KA, Hurley RW. Pulsed radiofrequency of the dorsal root ganglia is superior to pharmacotherapy or pulsed radiofrequency of the intercostal nerves in the treatment of chronic postsurgical thoracic pain. Pain Physician. 2006; 9:227–235. PMID: 16886031.76. Byrd D, Mackey S. Pulsed radiofrequency for chronic pain. Curr Pain Headache Rep. 2008; 12:37–41. PMID: 18417022.
Article77. Rea W, Kapur S, Mutagi H. Radiofrequency therapies in chronic pain. Contin Educ Anaesth Crit Care Pain. 2011; 11:35–38.
Article78. Kastler A, Aubry S, Piccand V, Hadjidekov G, Tiberghien F, Kastler B. Radiofrequency neurolysis versus local nerve infiltration in 42 patients with refractory chronic inguinal neuralgia. Pain Physician. 2012; 15:237–244. PMID: 22622908.79. Subedi B, Grossberg GT. Phantom limb pain: mechanisms and treatment approaches. Pain Res Treat. 2011; 2011:864605. PMID: 22110933.
Article80. Graybill J, Conermann T, Kabazie AJ, Chandy S. Spinal cord stimulation for treatment of pain in a patient with post thoracotomy pain syndrome. Pain Physician. 2011; 14:441–445. PMID: 21927048.81. Shipton E. Post-surgical neuropathic pain. ANZ J Surg. 2008; 78:548–555. PMID: 18593408.
Article82. Wong L. Intercostal neuromas: a treatable cause of postoperative breast surgery pain. Ann Plast Surg. 2001; 46:481–484. PMID: 11352419.
Article83. Williams EH, Williams CG, Rosson GD, Heitmiller RF, Dellon AL. Neurectomy for treatment of intercostal neuralgia. Ann Thorac Surg. 2008; 85:1766–1770. PMID: 18442581.
Article84. Caviggioli F, Maione L, Forcellini D, Klinger F, Klinger M. Autologous fat graft in postmastectomy pain syndrome. Plast Reconstr Surg. 2011; 128:349–352. PMID: 21788826.
Article85. Hakeem A, Shanmugam V. Current trends in the diagnosis and management of post-herniorraphy chronic groin pain. World J Gastrointest Surg. 2011; 3:73–81. PMID: 21765970.
Article86. Eccleston C. Role of psychology in pain management. Br J Anaesth. 2001; 87:144–152. PMID: 11460803.
Article87. Turk DC, Audette J, Levy RM, Mackey SC, Stanos S. Assessment and treatment of psychosocial comorbidities in patients with neuropathic pain. Mayo Clin Proc. 2010; 85:S42–S50. PMID: 20194148.
Article88. Brox JI, Reikerås O, Nygaard Ø, Sørensen R, Indahl A, Holm I, et al. Lumbar instrumented fusion compared with cognitive intervention and exercises in patients with chronic back pain after previous surgery for disc herniation: a prospective randomized controlled study. Pain. 2006; 122:145–155. PMID: 16545523.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Evaluation of Zomepirac in the Treatment of Chronic Pain
- Practical strategies for the prevention and management of chronic postsurgical pain
- Effectiveness of Duloxetine for Postsurgical Chronic Neuropathic Disorders after Spine and Spinal Cord Surgery
- Opioid Pharmacotherapy for Chronic Noncancer Pain: The American Experience
- Cell based therapy for the management of chronic pain