Cancer Res Treat.
2018 Jul;50(3):975-983. 10.4143/crt.2017.459.
Patterns of Rectal Cancer Radiotherapy Adopting Evidence-Based Medicine: An Analysis of the National Database from 2005 to 2016
- Affiliations
-
- 1Department of Radiation Oncology, Hanyang University Hospital, Seoul, Korea.
- 2Department of Health Policy and Management, Seoul National University College of Medicine, Seoul, Korea. yoonkim@snu.ac.kr
- 3Institute of Health Policy and Management, Medical Research Center, Seoul National University, Seoul, Korea.
- KMID: 2417886
- DOI: http://doi.org/10.4143/crt.2017.459
Abstract
- PURPOSE
Not many studies have evaluated the adoption and dissemination of evidence-based medicine in rectal cancer radiotherapy (RT). We aimed to analyze the differences by institutional characteristics and geography in adopting evidence-based care for rectal cancer RT and factors affecting the adoption in Korea.
MATERIALS AND METHODS
Korean National Health Insurance Service claims database was used. All rectal cancer patients treated with radical surgery and adjuvant RT at the same institution in 2005-2016 were included in this study. RT within 3 months before and after surgery was regarded as preoperative and postoperative RT, respectively.
RESULTS
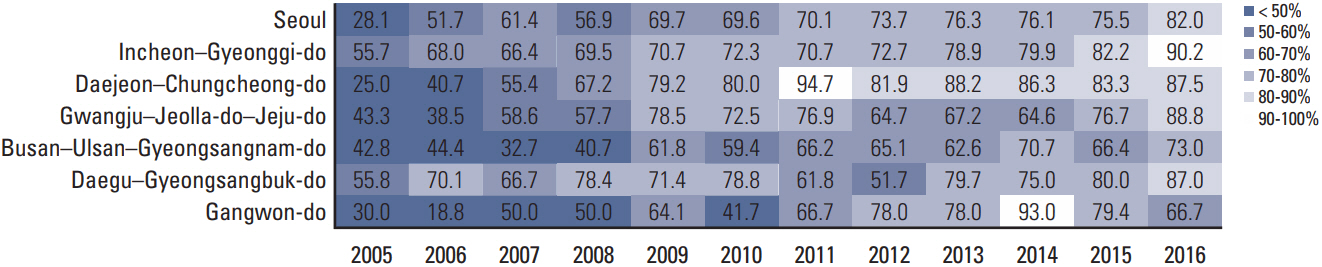
A total of 16,827 patients treated in 83 institutions were included in the analysis. The use of preoperative RT has substantially increased over time, from 40.6% in 2005 to 84.2% in 2016 all over the nation. The proportion of preoperative RT (54.8%) exceeded that of postoperative RT (45.2%) in 2006. However, a wide range of institutional and regional variation was observed. Compared to high-volume institutions, low-volume institutions showed late adoption and variable dissemination patterns of preoperative RT. Busan-Ulsan-Gyeongsangnam-do and Gangwon-do showed slower adoption and less use of preoperative RT than other region.
CONCLUSION
We demonstrated gradual and steady increase in adoption of preoperative RT in rectal cancer treatment nationally from 2005 to 2016. Institutional variations between high- and low-volume institutions were observed.
MeSH Terms
Figure
Cited by 1 articles
-
CCR6 Is a Predicting Biomarker of Radiosensitivity and Potential Target of Radiosensitization in Rectal Cancer
Hui Chang, Jia-wang Wei, Ya-lan Tao, Pei-rong Ding, Yun-fei Xia, Yuan-hong Gao, Wei-wei Xiao
Cancer Res Treat. 2018;50(4):1203-1213. doi: 10.4143/crt.2017.538.
Reference
-
References
1. Gastrointestinal Tumor Study Group. Prolongation of the disease-free interval in surgically treated rectal carcinoma. N Engl J Med. 1985; 312:1465–72.2. Krook JE, Moertel CG, Gunderson LL, Wieand HS, Collins RT, Beart RW, et al. Effective surgical adjuvant therapy for highrisk rectal carcinoma. N Engl J Med. 1991; 324:709–15.
Article3. Fitzgerald TL, Biswas T, O'Brien K, Zervos EE, Wong JH. Neoadjuvant radiotherapy for rectal cancer: adherence to evidence-based guidelines in clinical practice. World J Surg. 2013; 37:639–45.
Article4. Sauer R, Becker H, Hohenberger W, Rodel C, Wittekind C, Fietkau R, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004; 351:1731–40.
Article5. Koperny M, Lesniak W, Jankowski M, Bala M. The Cochrane collaboration: the role in the evolution of evidence-based medicine and development of cooperation in Poland. Przegl Epidemiol. 2016; 70:508–20.6. Reddy SS, Handorf B, Farma JM, Sigurdson ER. Trends with neoadjuvant radiotherapy and clinical staging for those with rectal malignancies. World J Gastrointest Surg. 2017; 9:97–102.
Article7. Murphy CC, Harlan LC, Lund JL, Lynch CF, Geiger AM. Patterns of colorectal cancer care in the United States: 1990-2010. J Natl Cancer Inst. 2015; 107:djv198.
Article8. Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. 2009; 24:63–71.
Article9. Ki YJ, Kim HJ, Kim MS, Park CM, Ko MJ, Seo YS, et al. Association between metformin use and survival in nonmetastatic rectal cancer treated with a curative resection: a nationwide population study. Cancer Res Treat. 2017; 49:29–36.
Article10. Sheldon TA, Guyatt GH, Haines A. Getting research findings into practice. When to act on the evidence. BMJ. 1998; 317:139–42.
Article11. Shiffman RN, Dixon J, Brandt C, Essaihi A, Hsiao A, Michel G, et al. The GuideLine Implementability Appraisal (GLIA): development of an instrument to identify obstacles to guideline implementation. BMC Med Inform Decis Mak. 2005; 5:23.
Article12. National Cancer Center. Cancer registration statistics data [Internet]. Goyang: National Cancer Center;2017. [cited 2017 Sep 1]. Available from: http://www.ncc.re.kr/cancerStatsList.ncc?searchKey=total&searchValue=&pageNum=1.13. Stewart DB, Hollenbeak C, Desharnais S, Camacho F, Gladowski P, Goff VL, et al. Rectal cancer and teaching hospitals: hospital teaching status affects use of neoadjuvant radiation and survival for rectal cancer patients. Ann Surg Oncol. 2013; 20:1156–63.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trends in intensity-modulated radiation therapy use for rectal cancer in the neoadjuvant setting: a National Cancer Database analysis
- Controversial issues in radiotherapy for rectal cancer: a systematic review
- Effect of chemotherapy and radiotherapy on cognitive impairment in colorectal cancer: evidence from Korean National Health Insurance Database Cohort
- Evidence-based National Cancer Screening program of Korea
- Recent Trend of the Postoperative Adjuvant Therapy in Endometrial Cancer