Cancer Res Treat.
2018 Jul;50(3):777-790. 10.4143/crt.2017.255.
Neutropenia during the First Cycle of Induction Chemotherapy Is Prognostic for Poor Survival in Locoregionally Advanced Nasopharyngeal Carcinoma: A Real-World Study in an Endemic Area
- Affiliations
-
- 1Department of Radiation Oncology, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangzhou, China. majun2@mail.sysu.edu.cn
- 2Department of Radiology, Hainan Province People’s Hospital, Haikou, China.
- 3Department of Medical Statistics and Epidemiology, School of Public Health, Sun Yat-sen University, Guangzhou, China.
- KMID: 2417867
- DOI: http://doi.org/10.4143/crt.2017.255
Abstract
- PURPOSE
The purpose of this study was to investigate the effect of neutropenia during the first cycle of induction chemotherapy (IC-1) on survival in locoregionally advanced nasopharyngeal carcinoma (LANPC).
MATERIALS AND METHODS
Eligible patients (n=545) with LANPC receiving IC+concurrent chemoradiotherapy were included. Based on nadir neutrophil afterIC-1, all patientswere categorized into three groups: no/grade 1-2/grade 3-4 neutropenia. Five-year overall survival (OS) and disease-free survival (DFS) were compared between groups and subgroups stratified by IC regimen. We also explored the occurrence of IC-1-induced myelosuppression events and the minimal value of post-treatment neutrophil-to-lymphocyte ratio (post-NLRmin). Univariate/multivariate analyses were performed to investigate the effect of IC-1-induced neutropenia, timing of neutropenia, number of myelosuppression events, and high post-NLRmin on OS/DFS.
RESULTS
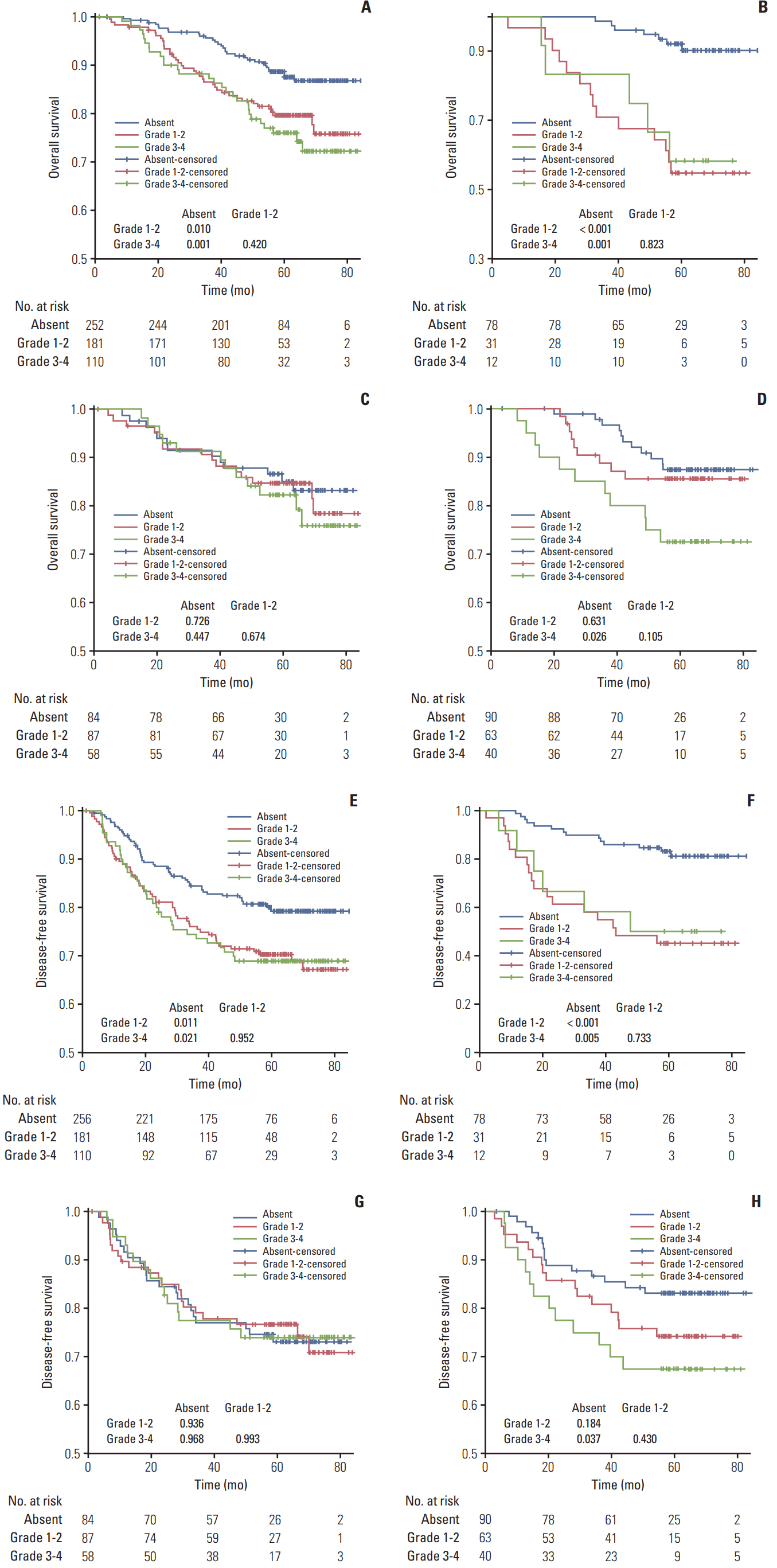
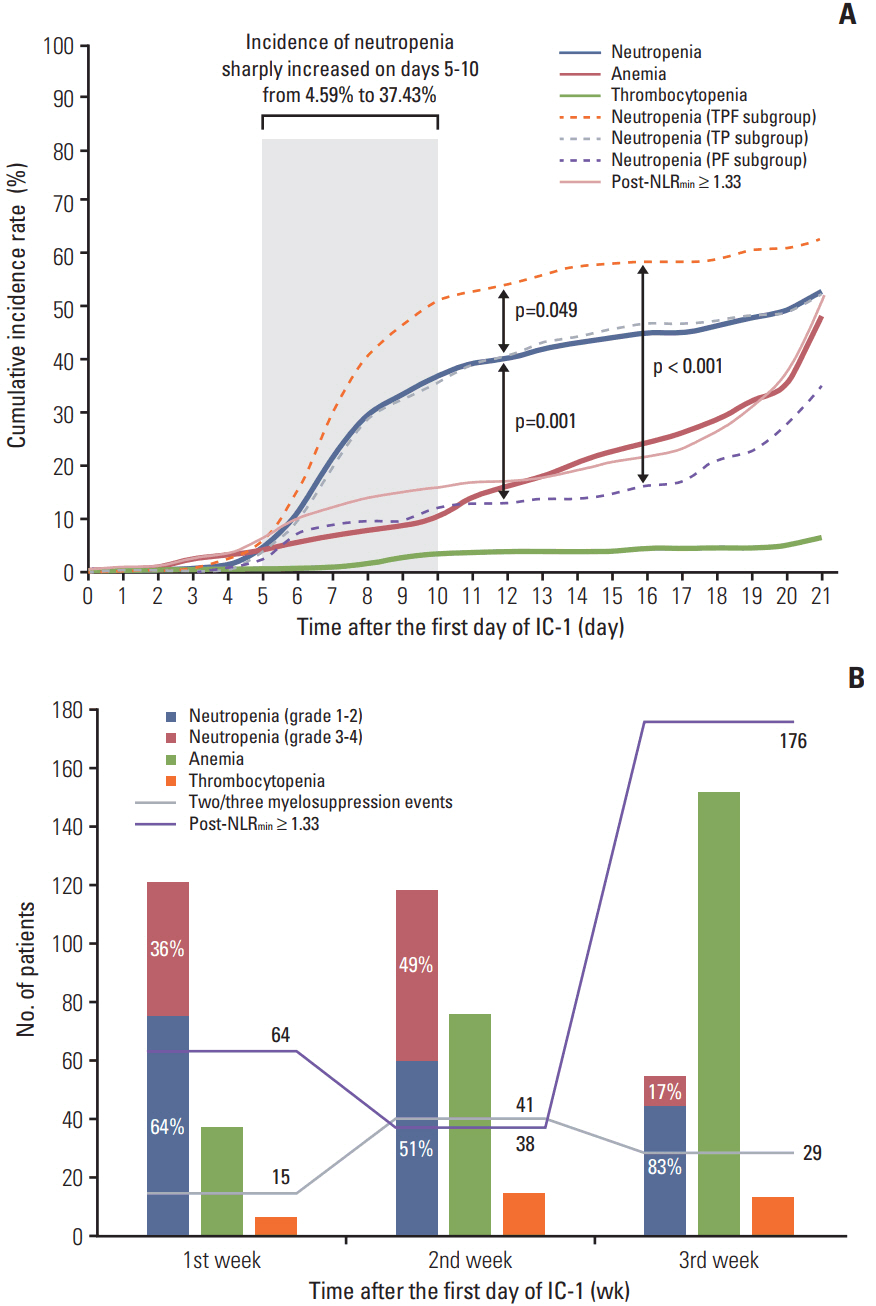
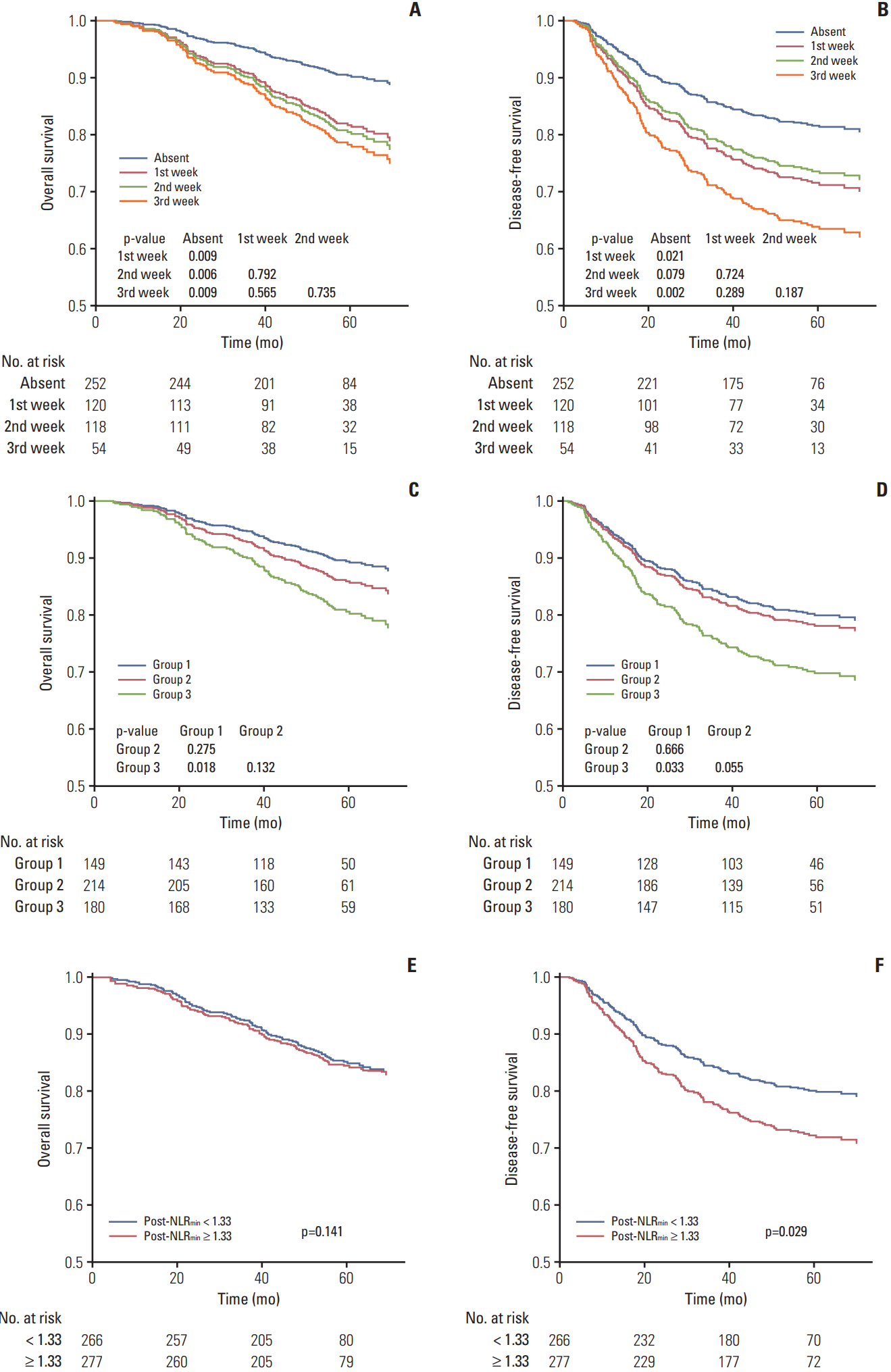
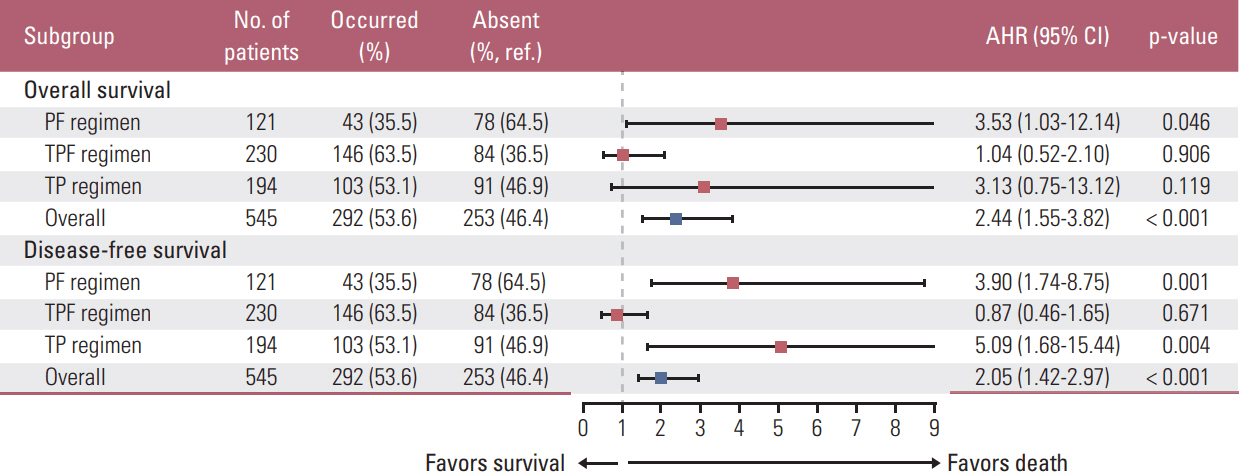
Grade 1-2/grade 3-4 neutropeniawere associatedwith poorer OS/DFS than no neutropenia (all p < 0.05); OS/DFS were not significantly different between patients experiencing grade 1-2 vs. 3-4 neutropenia. Neutropenia had no significant effect on OS/DFS in patients receiving docetaxel-cisplatin-5-fluorouracil (TPF). Grade 1-2 (grade 3-4) neutropenia negatively influenced OS/DFS in patients receiving cisplatin-5-fluorouracil (PF) (PF and docetaxel-cisplatin [TP]; all p < 0.05). Neutropenia, two/three myelosuppression events, and high post-NLRmin (≥ 1.33) was most frequent on days 5-10, second and third week of IC-1, respectively. After adjustment for covariates, IC-1-induced neutropenia, two/three myelosuppression events, and post-NLRmin ≥ 1.33were validated as negative predictors of OS/DFS (all p < 0.05); timing of neutropenia had no significant effect.
CONCLUSION
Occurrence of neutropenia, number of myelosuppression events, and high post-NLRmin during PF/TP IC-1 have prognostic value for poor survival in LANPC.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Mao YP, Xie FY, Liu LZ, Sun Y, Li L, Tang LL, et al. Re-evaluation of 6th edition of AJCC staging system for nasopharyngeal carcinoma and proposed improvement based on magnetic resonance imaging. Int J Radiat Oncol Biol Phys. 2009; 73:1326–34.
Article2. Sun Y, Li WF, Chen NY, Zhang N, Hu GQ, Xie FY, et al. Induction chemotherapy plus concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in locoregionally advanced nasopharyngeal carcinoma: a phase 3, multicentre, randomised controlled trial. Lancet Oncol. 2016; 17:1509–20.3. Kuderer NM, Dale DC, Crawford J, Cosler LE, Lyman GH. Mortality, morbidity, and cost associated with febrile neutropenia in adult cancer patients. Cancer. 2006; 106:2258–66.
Article4. Lyman GH, Kuderer NM, Crawford J, Wolff DA, Culakova E, Poniewierski MS, et al. Predicting individual risk of neutropenic complications in patients receiving cancer chemotherapy. Cancer. 2011; 117:1917–27.
Article5. Chen Y, Wang Y, Shi Y, Dai G. Timing of chemotherapy-induced neutropenia predicts prognosis in metastatic colon cancer patients: a retrospective study in mFOLFOX6 -treated patients. BMC Cancer. 2017; 17:242.
Article6. Lee CY, Park SY, Shin TR, Park YB, Kim CH, Jang SH, et al. Early-onset neutropenia during perioperative chemotherapy is predictive of increased survival in patients with completely resected non-small cell lung cancer: a retrospective analysis. Anticancer Res. 2013; 33:2755–61.7. Kishida Y, Kawahara M, Teramukai S, Kubota K, Komuta K, Minato K, et al. Chemotherapy-induced neutropenia as a prognostic factor in advanced non-small-cell lung cancer: results from Japan Multinational Trial Organization LC00-03. Br J Cancer. 2009; 101:1537–42.
Article8. Di Maio M, Gridelli C, Gallo C, Shepherd F, Piantedosi FV, Cigolari S, et al. Chemotherapy-induced neutropenia and treatment efficacy in advanced non-small-cell lung cancer: a pooled analysis of three randomised trials. Lancet Oncol. 2005; 6:669–77.
Article9. Tewari KS, Java JJ, Gatcliffe TA, Bookman MA, Monk BJ. Chemotherapy-induced neutropenia as a biomarker of survival in advanced ovarian carcinoma: an exploratory study of the Gynecologic Oncology Group. Gynecol Oncol. 2014; 133:439–45.
Article10. Kim JJ, Park JY, Kim DY, Kim JH, Kim YM, Nam JH, et al. Is chemotherapy-induced neutropenia a prognostic factor in patients with ovarian cancer? Acta Obstet Gynecol Scand. 2010; 89:623–8.
Article11. Kumpulainen EJ, Hirvikoski PP, Johansson RT. Neutropenia during adjuvant chemotherapy of breast cancer is not a predictor of outcome. Acta Oncol. 2009; 48:1204–6.
Article12. Bogani G, Sabatucci I, Maltese G, Lecce F, Signorelli M, Martinelli F, et al. Chemotherapy-related leukopenia as a biomarker predicting survival outcomes in locally advanced cervical cancer. Eur J Obstet Gynecol Reprod Biol. 2017; 208:41–5.
Article13. Miyoshi N, Yano M, Takachi K, Kishi K, Noura S, Eguchi H, et al. Myelotoxicity of preoperative chemoradiotherapy is a significant determinant of poor prognosis in patients with T4 esophageal cancer. J Surg Oncol. 2009; 99:302–6.
Article14. Blay JY, Chauvin F, Le Cesne A, Anglaret B, Bouhour D, Lasset C, et al. Early lymphopenia after cytotoxic chemotherapy as a risk factor for febrile neutropenia. J Clin Oncol. 1996; 14:636–43.
Article15. Crawford J, Dale DC, Lyman GH. Chemotherapy-induced neutropenia: risks, consequences, and new directions for its management. Cancer. 2004; 100:228–37.16. Wong G, Chapman JR. Cancers after renal transplantation. Transplant Rev (Orlando). 2008; 22:141–9.
Article17. Xu C, Chen YP, Liu X, Li WF, Chen L, Mao YP, et al. Establishing and applying nomograms based on the 8th edition of the UICC/AJCC staging system to select patients with nasopharyngeal carcinoma who benefit from induction chemotherapy plus concurrent chemoradiotherapy. Oral Oncol. 2017; 69:99–107.
Article18. Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancerrelated inflammation and treatment effectiveness. Lancet Oncol. 2014; 15:e493–503.
Article19. Sherman RE, Anderson SA, Dal Pan GJ, Gray GW, Gross T, Hunter NL, et al. Real-world evidence: what is it and what can it tell us? N Engl J Med. 2016; 375:2293–7.20. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958; 53:457–81.
Article21. Neyeloff JL, Fuchs SC, Moreira LB. Meta-analyses and Forest plots using a microsoft excel spreadsheet: step-by-step guide focusing on descriptive data analysis. BMC Res Notes. 2012; 5:52.
Article22. Li XH, Chang H, Xu BQ, Tao YL, Gao J, Chen C, et al. An inflammatory biomarker-based nomogram to predict prognosis of patients with nasopharyngeal carcinoma: an analysis of a prospective study. Cancer Med. 2017; 6:310–9.
Article23. Azab B, Mohammad F, Shah N, Vonfrolio S, Lu W, Kedia S, et al. The value of the pretreatment neutrophil lymphocyte ratio vs. platelet lymphocyte ratio in predicting the long-term survival in colorectal cancer. Cancer Biomark. 2014; 14:303–12.
Article24. Ferrucci PF, Ascierto PA, Pigozzo J, Del Vecchio M, Maio M, Antonini Cappellini GC, et al. Baseline neutrophils and derived neutrophil-to-lymphocyte ratio: prognostic relevance in metastatic melanoma patients receiving ipilimumab. Ann Oncol. 2016; 27:732–8.
Article25. Liang W, Shen G, Zhang Y, Chen G, Wu X, Li Y, et al. Development and validation of a nomogram for predicting the survival of patients with non-metastatic nasopharyngeal carcinoma after curative treatment. Chin J Cancer. 2016; 35:98.
Article26. Peng H, Chen L, Zhang Y, Li WF, Mao YP, Zhang F, et al. Prognostic value of the cumulative cisplatin dose during concurrent chemoradiotherapy in locoregionally advanced nasopharyngeal carcinoma: a secondary analysis of a prospective phase III clinical trial. Oncologist. 2016; 21:1369–76.
Article27. Burdach S, van Kaick B, Laws HJ, Ahrens S, Haase R, Korholz D, et al. Allogeneic and autologous stem-cell transplantation in advanced Ewing tumors: an update after long-term followup from two centers of the European Intergroup study EICESS. Stem-Cell Transplant Programs at Dusseldorf University Medical Center, Germany and St. Anna Kinderspital, Vienna, Austria. Ann Oncol. 2000; 11:1451–62.28. Liu LT, Chen QY, Tang LQ, Guo SS, Guo L, Mo HY, et al. The prognostic value of treatment-related lymphopenia in nasopharyngeal carcinoma patients. Cancer Res Treat. 2017; 50:19–29.
Article29. Sun W, Zhang L, Luo M, Hu G, Mei Q, Liu D, et al. Pretreatment hematologic markers as prognostic factors in patients with nasopharyngeal carcinoma: neutrophil-lymphocyte ratio and platelet-lymphocyte ratio. Head Neck. 2016; 38 Suppl 1:E1332–40.
Article30. An X, Ding PR, Wang FH, Jiang WQ, Li YH. Elevated neutrophil to lymphocyte ratio predicts poor prognosis in nasopharyngeal carcinoma. Tumour Biol. 2011; 32:317–24.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Induction Chemotherapy Plus Concurrent Chemoradiotherapy Versus Concurrent Chemoradiotherapy Alone in Locoregionally Advanced Nasopharyngeal Carcinoma in Children and Adolescents: A Matched Cohort Analysis
- Less is more: role of additional chemotherapy to concurrent chemoradiotherapy in locoregionally advanced nasopharyngeal cancer management
- Locoregionally advanced nasopharyngeal carcinoma treated with intensity-modulated radiotherapy plus concurrent weekly cisplatin with or without neoadjuvant chemotherapy
- Prognostic Value of Serum Epstein-Barr Virus Antibodies and Their Correlation with TNM Classification in Patients with Locoregionally Advanced Nasopharyngeal Carcinoma
- Neoadjuvant Chemotherapy and Radiation Therapy inAdvanced Stage Nasopharyngeal Carcinoma