Cancer Res Treat.
2018 Jul;50(3):670-680. 10.4143/crt.2017.051.
Comparison of Native Escherichia coli L-Asparaginase versus Pegylated Asparaginase, in Combination with Ifosfamide, Methotrexate, Etoposide, and Prednisolone, in Extranodal NK/T-Cell Lymphoma, Nasal Type
- Affiliations
-
- 1Department of Pharmacy, Seoul National University Hospital, Seoul, Korea.
- 2Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea. gabriel9@snu.ac.kr
- 3Seoul National University Cancer Research Institute, Seoul, Korea.
- 4College of Pharmacy and Institute of Pharmaceutical Science and Technology, Hanyang University, Guri, Korea.
- 5Department of Radiation Oncology, Seoul National University Hospital, Seoul, Korea.
- KMID: 2417856
- DOI: http://doi.org/10.4143/crt.2017.051
Abstract
- PURPOSE
The aim of this study was to compare asparaginase-related toxicities in two asparaginase preparations, namely native Escherichia coli L-asparaginase (L-ASP) and pegylated asparaginase (PEG-ASP) in combination with ifosfamide, methotrexate, etoposide, and prednisolone (IMEP) in natural killer (NK)/T-cell lymphoma (NTCL).
MATERIALS AND METHODS
A total of 41 NTCL patients who received IMEP plus native E. coli L-ASP or PEG-ASP at Seoul National University Hospital were included in this study between January 2013 and March 2016. IMEP/ASP treatment consisted of ifosfamide, methotrexate, etoposide, plus native E. coli L-ASP (6,000 IU/m2 on days 1, 3, 5, 7, 9, and 11) or PEG-ASP (2,500 IU/m2 on day 1) every 3 weeks. ASP-related toxicities, toxicity patterns, length of hospital stay, and clinical outcomes were compared between the different treatment groups.
RESULTS
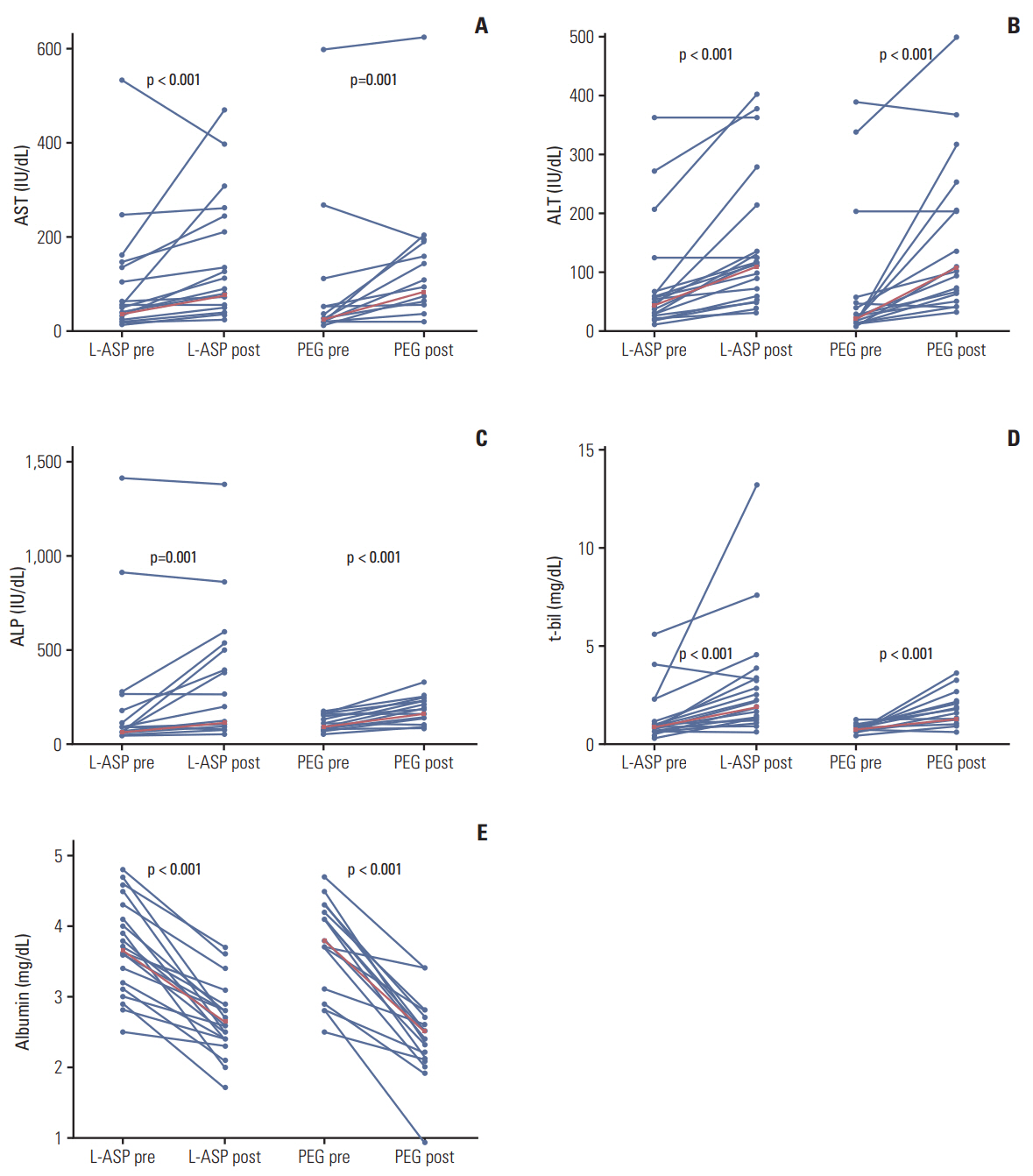
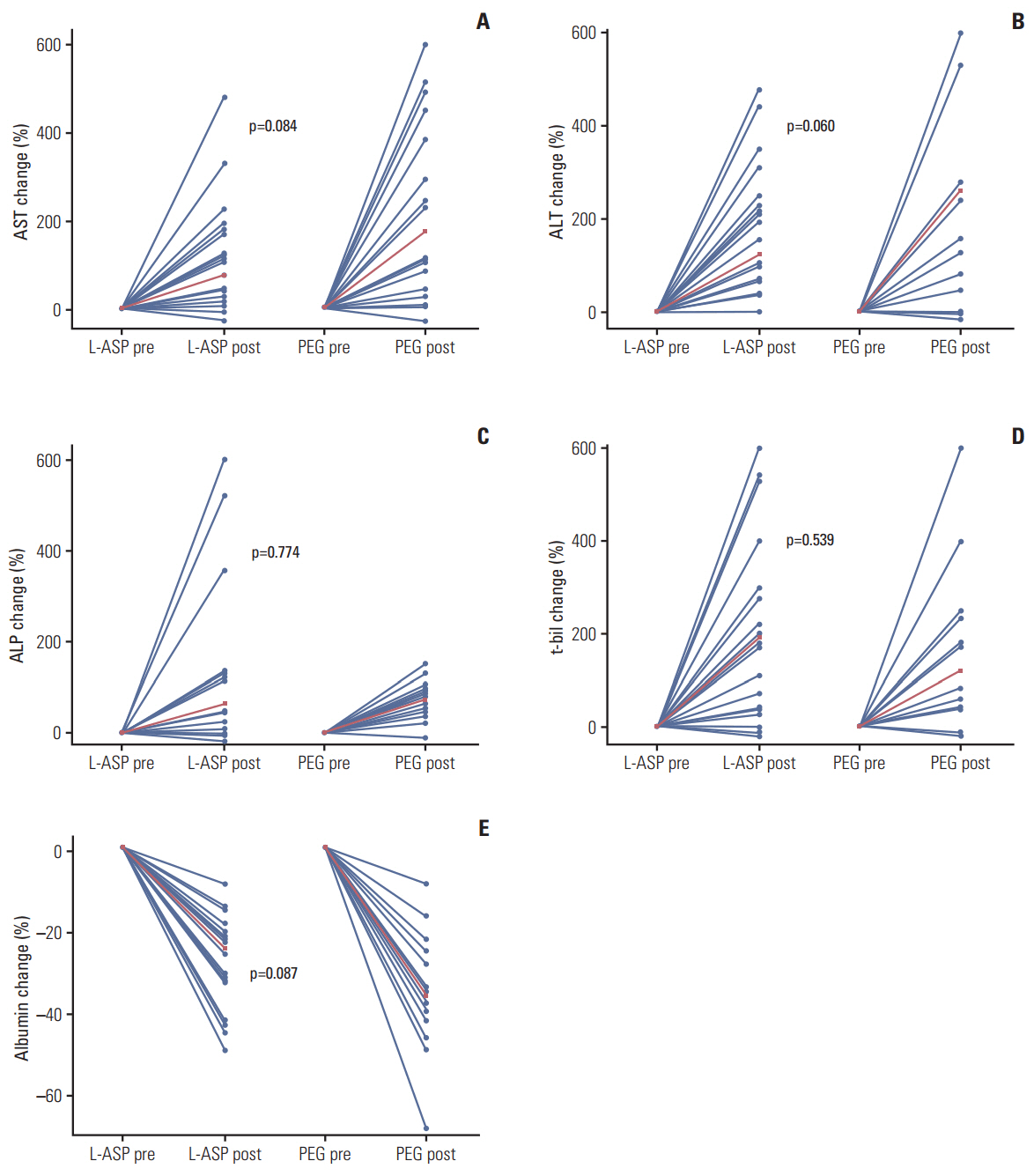
The frequency of ASP-related toxicities was similar between the IMEP plus native E. coli L-ASP group and the PEG-ASP group apart from hypofibrinogenemia (native E. coli L-ASP vs. PEG-ASP group, 86.4% vs. 36.8%; p=0.001). Although post-treatment transaminase and albumin levels were significantly high and low, respectively, hepatotoxicity gradients before and after treatment did not differ significantly between the groups. Since PEG-ASP was given at an outpatient clinic in some patients, length of hospital stay was significantly shorter in the IMEP plus PEG-ASP group (median, 4.0 vs. 6.0 days; p=0.002). A favorable tendency of clinical outcomes was observed in NTCL patients treated with IMEP plus PEG-ASP (complete remission rate, 73.7% vs. 45.5%; p=0.067).
CONCLUSION
IMEP plus PEG-ASP showed similar ASP-related toxicities, shorter length of hospital stay, and a trend towards improved clinical outcomes compared with IMEP plus native E. coli L-ASP in NTCL.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Sabattini E, Bacci F, Sagramoso C, Pileri SA. WHO classification of tumours of haematopoietic and lymphoid tissues in 2008: an overview. Pathologica. 2010; 102:83–7.2. Kwong YL, Chan AC, Liang R, Chiang AK, Chim CS, Chan TK, et al. CD56+ NK lymphomas: clinicopathological features and prognosis. Br J Haematol. 1997; 97:821–9.3. Yamaguchi M, Kita K, Miwa H, Nishii K, Oka K, Ohno T, et al. Frequent expression of P-glycoprotein/MDR1 by nasal T-cell lymphoma cells. Cancer. 1995; 76:2351–6.
Article4. Kwong YL, Kim WS, Lim ST, Kim SJ, Tang T, Tse E, et al. SMILE for natural killer/T-cell lymphoma: analysis of safety and efficacy from the Asia Lymphoma Study Group. Blood. 2012; 120:2973–80.
Article5. Yamaguchi M, Kwong YL, Kim WS, Maeda Y, Hashimoto C, Suh C, et al. Phase II study of SMILE chemotherapy for newly diagnosed stage IV, relapsed, or refractory extranodal natural killer (NK)/T-cell lymphoma, nasal type: the NK-Cell Tumor Study Group study. J Clin Oncol. 2011; 29:4410–6.
Article6. Jaccard A, Gachard N, Marin B, Rogez S, Audrain M, Suarez F, et al. Efficacy of L-asparaginase with methotrexate and dexamethasone (AspaMetDex regimen) in patients with refractory or relapsing extranodal NK/T-cell lymphoma, a phase 2 study. Blood. 2011; 117:1834–9.
Article7. Tong WH, Pieters R, Kaspers GJ, te Loo DM, Bierings MB, van den Bos C, et al. A prospective study on drug monitoring of PEGasparaginase and Erwinia asparaginase and asparaginase antibodies in pediatric acute lymphoblastic leukemia. Blood. 2014; 123:2026–33.
Article8. Pieters R, Hunger SP, Boos J, Rizzari C, Silverman L, Baruchel A, et al. L-asparaginase treatment in acute lymphoblastic leukemia: a focus on Erwinia asparaginase. Cancer. 2011; 117:238–49.9. Silverman LB, Gelber RD, Dalton VK, Asselin BL, Barr RD, Clavell LA, et al. Improved outcome for children with acute lymphoblastic leukemia: results of Dana-Farber Consortium Protocol 91-01. Blood. 2001; 97:1211–8.
Article10. Kearney SL, Dahlberg SE, Levy DE, Voss SD, Sallan SE, Silverman LB. Clinical course and outcome in children with acute lymphoblastic leukemia and asparaginase-associated pancreatitis. Pediatr Blood Cancer. 2009; 53:162–7.
Article11. Grace RF, Dahlberg SE, Neuberg D, Sallan SE, Connors JM, Neufeld EJ, et al. The frequency and management of asparaginase-related thrombosis in paediatric and adult patients with acute lymphoblastic leukaemia treated on Dana-Farber Cancer Institute consortium protocols. Br J Haematol. 2011; 152:452–9.
Article12. Henriksen LT, Harila-Saari A, Ruud E, Abrahamsson J, Pruunsild K, Vaitkeviciene G, et al. PEG-asparaginase allergy in children with acute lymphoblastic leukemia in the NOPHO ALL2008 protocol. Pediatr Blood Cancer. 2015; 62:427–33.
Article13. Vrooman LM, Stevenson KE, Supko JG, O'Brien J, Dahlberg SE, Asselin BL, et al. Postinduction dexamethasone and individualized dosing of Escherichia coli L-asparaginase each improve outcome of children and adolescents with newly diagnosed acute lymphoblastic leukemia: results from a randomized study: Dana-Farber Cancer Institute ALL Consortium Protocol 00-01. J Clin Oncol. 2013; 31:1202–10.14. Park YK, Abuchowski A, Davis S, Davis F. Pharmacology of Escherichia coli-L-asparaginase polyethylene glycol adduct. Anticancer Res. 1981; 1:373–6.15. Stock W, Douer D, DeAngelo DJ, Arellano M, Advani A, Damon L, et al. Prevention and management of asparaginase/pegasparaginase-associated toxicities in adults and older adolescents: recommendations of an expert panel. Leuk Lymphoma. 2011; 52:2237–53.
Article16. Place AE, Stevenson KE, Vrooman LM, Harris MH, Hunt SK, O'Brien JE, et al. Intravenous pegylated asparaginase versus intramuscular native Escherichia coli L-asparaginase in newly diagnosed childhood acute lymphoblastic leukaemia (DFCI 05-001): a randomised, open-label phase 3 trial. Lancet Oncol. 2015; 16:1677–90.17. Avramis VI, Sencer S, Periclou AP, Sather H, Bostrom BC, Cohen LJ, et al. A randomized comparison of native Escherichia coli asparaginase and polyethylene glycol conjugated asparaginase for treatment of children with newly diagnosed standard-risk acute lymphoblastic leukemia: a Children's Cancer Group study. Blood. 2002; 99:1986–94.18. Bi XW, Xia Y, Zhang WW, Sun P, Liu PP, Wang Y, et al. Radiotherapy and PGEMOX/GELOX regimen improved prognosis in elderly patients with early-stage extranodal NK/T-cell lymphoma. Ann Hematol. 2015; 94:1525–33.
Article19. Wang JH, Wang L, Liu CC, Xia ZJ, Huang HQ, Lin TY, et al. Efficacy of combined gemcitabine, oxaliplatin and pegaspargase (P-gemox regimen) in patients with newly diagnosed advanced-stage or relapsed/refractory extranodal NK/T-cell lymphoma. Oncotarget. 2016; 7:29092–101.
Article20. Asselin BL, Whitin JC, Coppola DJ, Rupp IP, Sallan SE, Cohen HJ. Comparative pharmacokinetic studies of three asparaginase preparations. J Clin Oncol. 1993; 11:1780–6.
Article21. Muller HJ, Loning L, Horn A, Schwabe D, Gunkel M, Schrappe M, et al. Pegylated asparaginase (Oncaspar) in children with ALL: drug monitoring in reinduction according to the ALL/NHL-BFM 95 protocols. Br J Haematol. 2000; 110:379–84.22. Panetta JC, Gajjar A, Hijiya N, Hak LJ, Cheng C, Liu W, et al. Comparison of native E. coli and PEG asparaginase pharmacokinetics and pharmacodynamics in pediatric acute lymphoblastic leukemia. Clin Pharmacol Ther. 2009; 86:651–8.
Article23. Pileri SA, Grogan TM, Harris NL, Banks P, Campo E, Chan JK, et al. Tumours of histiocytes and accessory dendritic cells: an immunohistochemical approach to classification from the International Lymphoma Study Group based on 61 cases. Histopathology. 2002; 41:1–29.
Article24. Kim SJ, Yoon DH, Jaccard A, Chng WJ, Lim ST, Hong H, et al. A prognostic index for natural killer cell lymphoma after non-anthracycline-based treatment: a multicentre, retrospective analysis. Lancet Oncol. 2016; 17:389–400.
Article25. Lee J, Suh C, Park YH, Ko YH, Bang SM, Lee JH, et al. Extranodal natural killer T-cell lymphoma, nasal-type: a prognostic model from a retrospective multicenter study. J Clin Oncol. 2006; 24:612–8.
Article26. Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007; 25:579–86.
Article27. Dinndorf PA, Gootenberg J, Cohen MH, Keegan P, Pazdur R. FDA drug approval summary: pegaspargase (oncaspar) for the first-line treatment of children with acute lymphoblastic leukemia (ALL). Oncologist. 2007; 12:991–8.
Article28. Howard SC, Pui CH. Endocrine complications in pediatric patients with acute lymphoblastic leukemia. Blood Rev. 2002; 16:225–43.
Article29. Hongo T, Okada S, Ohzeki T, Ohta H, Nishimura S, Hamamoto K, et al. Low plasma levels of hemostatic proteins during the induction phase in children with acute lymphoblastic leukemia: a retrospective study by the JACLS. Japan Association of Childhood Leukemia Study. Pediatr Int. 2002; 44:293–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extranodal NK/T cell lymphoma
- A Clinical Study of the Side Effects of L-Asparaginase
- Effectiveness of L-asparaginase-based regimens compared to anthracycline-based regimens in newly diagnosed extranodal NK/T-cell lymphoma, nasal type: a single Mexican center experience
- Extranodal NK/T Cell Lymphoma, Nasal Type that Occurred in Patients with Atrophic Rhinitis
- A Case of Cerebral Infarction in a Child with Acute Lymphoblastic Leukemia Developed during Chemotherapy with E coli Asparaginase